Hypertension and cardiovascular disease in the sub-Saharan African context
Introduction
Sub-Saharan Africa’s (sSA) epidemiological transition has been coined as a ‘double burden of disease’, from managing care for communicable diseases, such as tuberculosis and malaria, to the increasing prevalence of non-communicable diseases (NCDs) (1). Specifically, the incidence of hypertension (HTN) and cardiovascular disease (CVD), encompassing heart disease and stroke, has been increasing over the last several decades in sSA and can be attributed to many economic, cultural and social determinants of health (2). To illustrate, a systematic analysis of the Global Burden of Disease Study in 2013 elucidated that morbidity due to CVD in sSA had increased 81% since 1990 (2).
Contemporaneously, steep increases in the prevalence of HTN in sSA can be attributed to many of the same risk factors identified in reports from industrialized countries: increased salt intake and body weight, higher levels of stress, and decreased physical activity (1). Additionally, there are unique factors that explain the higher incidence of HTN in sSA, including the prevalence in urban areas, the frequent under-diagnosis of CVD and the severity of its complications, which place a public health and economic burden on these low and middle-income nations. Furthermore, the association of obesity and metabolic syndrome in sSA populations are affected by severe poverty, famine and civil strife, making the overall prevalence of HTN difficult to determine (3-5). Although HTN, CVD and associated risk factors are becoming more prevalent across sSA, disparities in the incidence of NCDs persist among subpopulations, regions and by socio-economic status, highlighting the importance to reveal and address these challenges to improve patient outcomes.
This editorial will comment on the past, present and future status of HTN and CVD in sSA and seek to unmask the potential root causes for the looming burden in CVD morbidity and mortality. The aim of this commentary is to also propose possible solutions to curb the upcoming CVD tsunami in sSA. In addressing HTN and CVD, we reflect on areas of national, regional, urban/rural, socioeconomic status and racial/ethnic disparities. Considering the extensive published research on black Africans and CVD burden in South Africa, much of the paper focuses on this subpopulation and region.
A historical overview: a snapshot of the state of NCDs in sSA
The surge of NCDs in sSA is multifactorial, often attributed to industrialization/urbanization, increasing life expectancies, availability of vaccines and more prevalent sedentary lifestyles (1). Moreover, historical data have all identified disparities in the diagnosis of NCDs among race, socio-economic status and age. To illustrate, a study in 1982 investigated the age-adjusted prevalence of HTN in an adult population in Durban, a metropolitan city in South Africa, using the World Health Organization’s (WHO) then-current definition of HTN as a systolic pressure ≥160 mmHg (6). Results showed that urban Blacks of the Zulu tribe had the highest prevalence of HTN at 25%, followed by White residents at 17%, ethnic Indians at 14% and rural Blacks at 9% (6). In comparison, a recent 2017 study investigating regional differences in the prevalence of HTN did not find a marked urban-rural difference in women, with 53.4% of hypertensive women in urban town of Soweto, South Africa and 52.1% in rural Agincourt, South Africa (7). However, there was a significantly higher prevalence of HTN in men in Soweto at 54.7%, compared to rural Agincourt and Dikgale at 39.9% and 29.2%, respectively (7).
Obesity in sSA
Obesity, defined as a body mass index ≥30 kg/m3 has been associated with increased blood pressure levels, especially in black patients. In 1998, the first South African Demographic and Health Survey (SADHS) was conducted, which analyzed obesity rates in a random sample of 13,802 subjects aged 15 years and older and identified obesity in 30% of females and 8% of males (8). Comparatively, the SADHS was conducted again in 2016 and found that the prevalence of obesity increased from 30% to 68% of black women and from 8% to 31% in black men (8). It has been suggested that in Africa, the rural diet is relatively healthy to avoid risk factors for HTN and CVD, but due to urbanization, has been replaced foods in higher fat and a low carbohydrate intake. Consequently, black South Africans, who are more susceptible to these social determinants and may consume increasingly non-healthy dietary eating patterns and are more likely to lead to strokes than white South Africans. As such, it is especially important that those at risk population for CVD maintain healthy weight and decrease sodium intake.
The CVD impact of hyperinsulinemia, metabolic syndrome and type 2 diabetes mellitus (T2DM)
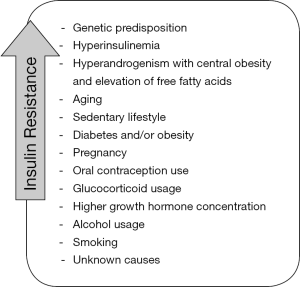
The relationship between T2DM and HTN has been well reported, where CVD is the leading cause of morbidity and mortality individuals with diabetes (9). Insulin resistance and HTN are conditions of metabolic syndrome that often co-exist, with 50% of hypertensive patients with hyperinsulinemia and up to 80% of individuals with T2DM diagnosed with HTN (10). Moreover, 59% of women and 29% of men in South Africa over the age of 15 are overweight or obese, underscoring these risk factors for CVD (11). While plasma insulin levels are consistently elevated in patients with T2DM who are obese, insulin resistance is often seen in patients with healthy body weight as well. The association between obesity and metabolic syndrome in sSA has been studied using the insulin clamp technique, and has elucidated several factors that may lead to insulin resistance, illustrated in Figure 1.
Geography and economics: the impact of regions and socioeconomic status
As previously noted, there are widely available published data on public health in SA and this country is an excellent source to examine the impacts of geography and socioeconomic status, along with race/ethnicity. As of 2017, South Africa was the fifth most populous nation in Africa with 54,841,552 citizens and a population growth rate of 0.99% (12). Within the country, 80.2% of individuals identify as black African, 8.8% colored (a term used on the national census for citizens from mixed race ancestry), 8.4% white and 2.5% Indian/Asian (12). With a gross domestic product (GDP) per capita of $13,400 USD South Africa is considered a lower or middle-income country, and a Gini index of 62.5 ranks South Africa second as the nation with the highest income inequality between the rich and poor (12).
There are many economic factors that continue to hinder access to healthcare in sSA. To illustrate, as 16.6% of the population in South Africa lives below the poverty line, defined as earning less than $1 USD a day (12). While patient education and preventative care could help alleviate this burden of CVD on the country, South Africa spends only 8.8% of its GDP on health expenditures. This represents the economic constraints of disseminating a public health campaign to prevent CVD. Although social and cultural factors may prevent effective implementations of public health policies, there are strategies for their application that have been well described to be successful frameworks on the prevention, management and control of HTN, summarized in Table 1 (13).

Full table
Economist Jeffrey Sachs in his widely acclaimed book, “The end of poverty: how we can make it happen in our lifetime” describes why impoverished nations, including sSA, are unable to escape the cycle of poverty. Overall, eradicating poverty is an ambitious, but hopefully feasible goal. Nevertheless, gains in communicable diseases are undoubted but the difficulty remains, while ensuring progress in income and other dimensions of poverty eradication, concomitantly avoiding a rise in HTN and CVD (14).
Poverty and low socioeconomic status: a persistent concern
As previously noted, poverty may be categorized as those earning less than $1 USD per day, with life expectancy correlating strongly with income in sSA. There is a strong relationship between poverty and available healthcare faced by developing nations. Therefore, low-income patients are inherently susceptible to other secondary factors that may explain these disparities in the incidence of NCDs. The majority of physicians in South Africa work in the private sector (70%), leaving the remaining 30% to care for 85% of South Africans who do not have private health insurance (15). The situation is worse for South Africans living in rural areas, where 46% the country’s 49 million rural residents are served by only 12% of doctors and 19% of nurses (16).
Considering the above forces on patient care, what strategies can be employed to avoid premature CVD? The current approach to CVD prevention is not to focus solely on high-risk patients, but also to promote adoption of a culture where individuals change lifestyle habits to reduce risk factors for developing HTN, heart disease and stroke. Even when treatable cases are presented, particular attention should be given to the cost-effectiveness of therapies, as many countries in sSA have severe constraints in resources. For some nations, the health budget per capita does not exceed $10 USD per year, which is insufficient not only to meet the needs of CVD patients, but also to address the double burden represented by infectious diseases, particularly human immunodeficiency virus/acquired immunodeficiency syndrome (HIV/AIDS).
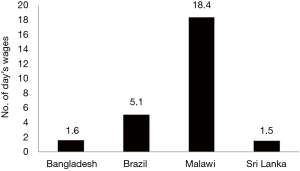
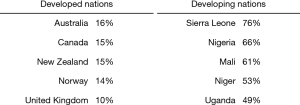
Primordial and primary prevention are key in avoiding the unnecessary rapid growth in CVD in sSA. However, secondary prevention, once HTN or CVD is present already, is also essential to decrease morbidity and mortality. Affordability is maybe defined as the number of day’s wages required for the lowest paid individual to purchase a 1-month supply of generic aspirin (100 mg), atenolol (100 mg), lisinopril (10 mg), and simvastatin (20 mg), daily (17). Coronary artery disease is a specific subset of CVD that also has important implications for prophylactic care, where affordability in a day’s wages in six low- or middle-income countries is shown in Figure 2 (18). Many patients in the developing world, such as Nigeria, purchase their anti-hypertensive medicines from out-of-pocket expenditures, whereas patients in the developed world, including the United States, and especially Canada, United Kingdom, and Australia have minimal out-of-pocket costs as compared to monthly wages, contrasted in Figure 3.
Urbanization and industrialization: increasing the burden of HTN and CVD
The relationship between urbanization and risk of CVD has been previously analyzed, revealing seemingly paradoxical results. While some studies suggest that with increased income, a Westernized diet and lifestyle would lead to increased risk of CVD, others conclude that increased resources available would lead to better access to preventative interventions and primary care (20). Researchers project that CVD will soon be responsible for more deaths in low- and middle-income countries, such as South Africa, than communicable diseases, including tuberculosis, HIV/AIDS and malaria (21). The WHO’s projections have been confirmed in sSA, as the prevalence of CVD continues to increase rapidly, with the majority of patients with CVD suffering from uncontrolled HTN (5). Specifically, in 2010, uncontrolled HTN in South Africa accounted for over 70% of all hypertensive patients (21). Appropriate diagnosis, accessibility to care and medications are critical in controlling HTN and CVD. On the other hand, social factors, including urbanization with increased impoverished neighborhoods, increased social disparity, crime, civil strife, poverty, famine, droughts and shortened lifespan due to the HIV/AIDS epidemic can impair the treatment for NCDs.
Adherence: a major factor to control HTN and CVD
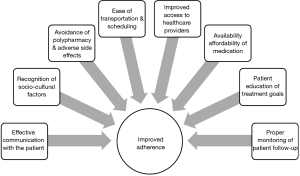
In 2013, CVD caused approximately 1 million deaths in sSA, an increase of 81% compared to 1990 (2). Furthermore, it was the sixth leading cause of disability, contributing to more than 11 million disability-adjusted life years, with uncontrolled HTN as the leading cause of dementia and renal failure, and a major cause of stroke. Adherence to medication is critical for the treatment of NCDs and to improve prognosis in patients with CVD. However, unique barriers to adherence exist in the sSA population and methods to improve adherence is illustrated in Figure 4.
Conclusions
Overall, HTN and CVD in the sSA context is facing a transitional disease paradigm, having to manage the burden of communicable disease prevalent from previous decades to the rise of NCDs. The increased prevalence of HTN and CVD has shown to be a multifactorial amalgam, where social determinants of health can restrict proper identification, evaluation and treatment for these chronic conditions. Many considerations are contributing to the rising incidence of CVD and management, and poverty continues to be the main underlying factor for the hindrance of patient care (22). As highlighted in this editorial, the state of CVD proves to be a complex issue, however, Nelson Mandela’s words in Organization of African Unity Summit in 1994 gives insight to the looming crises affecting the overall health and well-being in sSA.
“We must face the matter squarely that where there is something wrong in how we govern, known to ourselves, it must be said that the fault is not in our stars, but in ourselves. We know that we have it in ourselves, as Africans, to change all this. We must assert our will to do so—we must say that there is no obstacle big enough to stop us from bringing about an African renaissance.”—Nelson Mandela (23).
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- van der Sande MA. Cardiovascular disease in sub-Saharan Africa: a disaster waiting to happen. Neth J Med 2003;61:32-6. [PubMed]
- Mensah GA, Roth GA, Sampson UK, et al. Mortality from cardiovascular diseases in sub-Saharan Africa, 1990-2013: a systematic analysis of data from the Global Burden of Disease Study 2013. Cardiovasc J Afr 2015;26:S6-10. [Crossref] [PubMed]
- Lawes CM, Vander Hoorn S, Rodgers A, et al. Global burden of blood-pressure-related disease, 2001. Lancet 2008;371:1513-8. [Crossref] [PubMed]
- WHO. The world health report 2003: shaping the future. Geneva: World Health Organization, 2003.
- Seedat YK. Why is control of hypertension in sub-Saharan Africa poor? Cardiovasc J Afr 2015;26:193-5. [Crossref] [PubMed]
- Seedat YK, Seedat MA, Hackland DB. Prevalence of hypertension in the urban and rural Zulu. J Epidemiol Community Health 1982;36:256-61. [Crossref] [PubMed]
- Gómez-Olivé FX, Ali SA, Made F, et al. Regional and Sex Differences in the Prevalence and Awareness of Hypertension: An H3Africa AWI-Gen Study Across 6 Sites in Sub-Saharan Africa. Glob Heart 2017;12:81-90. [Crossref] [PubMed]
- South Africa Demographic and Health Survey 2016: Key Indicators. Available online: https://dhsprogram.com/pubs/pdf/PR84/PR84.pdf
- de Boer IH, Bangalore S, Benetos A, et al. Diabetes and Hypertension: A Position Statement by the American Diabetes Association. Diabetes Care 2017;40:1273-84. [Crossref] [PubMed]
- Zhou MS, Wang A, Yu H. Link between insulin resistance and hypertension: What is the evidence from evolutionary biology? Diabetol Metab Syndr 2014;6:12. [Crossref] [PubMed]
- Department of Health, Medical Research Council, ORC Macro. 2007. South Africa Demographic and Health Survey 2003. Pretoria: Department of Health.
- The World Factbook 2018. Washington, DC: Central Intelligence Agency, 2018.
- Mohsen Ibrahim M. Hypertension in Developing Countries: A Major Challenge for the Future. Curr Hypertens Rep 2018;20:38. [Crossref] [PubMed]
- Sachs J. The end of poverty: How we can make it in our lifetime. London: Penguin Books, 2005.
- Jenkins LS, Gunst C, Blitz J, et al. What keeps health professionals working in rural district hospitals in South Africa? Afr J Prim Health Care Fam Med 2015.7. [PubMed]
- Burch V, Reid S. Fit for purpose? The appropriate education of health professionals in South Africa. S Afr Med J 2011;101:25-6. [Crossref] [PubMed]
- Seedat YK. Fixed drug combination in hypertension and hyperlipidaemia in the developing world. Cardiovasc J Afr 2008;19:124-6. [PubMed]
- Steinbrook R. Drug shortages and public health. N Engl J Med 2009;361:1525-7. [Crossref] [PubMed]
- World Health Organization. WHO African Region Expenditure Atlas, November 2014. Available online: http://www.who.int/iris/handle/10665/145197
- Danaei G, Singh GM, Paciorek CJ, et al. The global cardiovascular risk transition: associations of four metabolic risk factors with national income, urbanization, and Western diet in 1980 and 2008. Circulation 2013;127:1493-502.e1-8.
- Fuster V, Kelly BB. Promoting Cardiovascular Health in the Developing World: A Critical Challenge to Achieve Global Health. Washington (DC): National Academies Press (US), 2010.
- Seedat YK. Impact of poverty on hypertension and cardiovascular disease in sub-Saharan Africa. Cardiovasc J Afr 2007;18:316-20. [PubMed]
- Kippenberg HG, Mersmann B. The Humanities Between Global Integration and Cultural Diversity. Berlin, Boston: De Gruyter, 2016.


