The economic case for US hospitals to revise their approach to heart failure readmission reduction
Introduction
US health care expenditures continue to rise, in 2016 reaching $3.3 trillion, accounting for 17.9% of the US gross domestic product (GDP) (1). This is more than the total GDP of the United Kingdom or France, and only slightly lower than the total GDP of Germany (2). While much of the historical increase in health care expenditures reflects the development of new treatments that have greatly improved health (3), currently there is widespread agreement that the system suffers from serious inefficiencies and persistent racial and socioeconomic disparities. To begin wringing these inefficiencies out of the health care system, US health care reform identified hospital readmission as a key area for improving care coordination and achieving potential savings (4). Unplanned hospital readmissions are associated with poor health outcomes and they account for more than $17 billion in Medicare expenditures annually, based on the best available information at this time (5). High readmission rates have also been documented in populations other than Medicare, such as Veterans Affairs hospitals (6) and non-elderly adults (7).
Two criteria for evaluating areas of impact on hospital readmissions included volume and costs. Based on these criteria, in 2010, the HRRP selected acute myocardial infarction (AMI), heart failure (HF), and pneumonia (PN) as target areas to reduce hospital readmissions for the Medicare population (in the later years of the HRRP, additional conditions were added). These conditions were chosen because of their high disease prevalence and their associated high costs for total admissions and readmissions for Medicare beneficiaries (8), as well as large variability in their readmission rates across hospitals (9).
Volume: rising disease prevalence, high numbers of hospital admission and readmission
In 2012, an estimated 5.8 million Americans 18 years of age or older had HF, of which approximately 60% were 65 years of age or older. By 2030, the prevalence of HF is expected to increase to over 8 million Americans 18 years of age or older, of which approximately 70% will be 65 years of age or older, due in part to the aging US population (10). Hospitalizations are common after HF diagnosis, with 83% of patients hospitalized at least once and 43% hospitalized at least four times (11). Congestive HF (non-hypertensive), which is an advanced form of HF, has the highest readmission rates (12) and has been one of the top principal diagnoses among hospital stays for persons 65 years of age or older (13).
Costs: increasing health care expenditures
With the rising prevalence of HF, we can expect an associated rise in HF healthcare expenditures. By 2030, the total cost of HF is projected to increase to $69.7 billion, from $30.7 billion in 2012 (10). Cost of HF care will increase almost 3-fold for those over 65 years of age, whereas a 1.6-fold increase is expected for those aged 45–64 years and a 2-fold increase for those aged 18–44 years (10). HF was the sixth most expensive condition treated in US hospitals at $10.2 billion (13), with readmissions accounting for $2.7 billion in 2013 (12). Those over 65 years of age have lower indirect costs because they are less likely to be employed, while for persons under 65 years of age indirect costs associated with productivity losses become more significant.
Large variation in HF readmission rates and costs: an opportunity for improvement
Besides volume and costs, another important consideration for the HRRP was the large variation in the risk standardized 30-day readmission rates (RSRR) across hospitals for the targeted conditions. Variation in RSRRs reflects differences in performance across hospitals; wider distributions suggest more variation in quality, thus, larger potential for improvement. A notable number of AMI, HF and PN readmissions are believed to be preventable through rigorous improvements in quality of care, including intensified post-discharge care coordination and patient follow-ups (5,14).
During the July 2012 and June 2015 period, hospital-level 30-day RSRRs following HF, AMI and PN ranged from 15.5% to 30.4%, 13.5% to 19.5%, and 12.9% to 23.1%, respectively. Additionally, HF had the highest absolute difference (14.9 percentage points) in RSRRs across all hospitals, and the highest median RSRR (21.6%) among all conditions (9). Various factors at different levels—patient, hospital or community—may be contributing to this variability. The HRRP is designed to narrow this variation by comparing a hospital’s performance to its national peers’ performances.
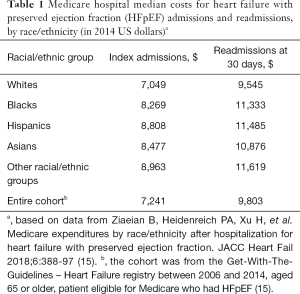
Considerable variation has also been observed in hospitalization and readmission costs by race/ethnicity and socioeconomic status. A recent study found that Medicare expenditures for HF with preserved ejection fraction (HFpEF) patients were higher for patients of black, Asian and other non-white race/ethnic groups (Table 1) (15). This prompts consideration for existing racial/ethnic disparities in access to quality care by lower socioeconomic communities. Improving health care delivery, as well as primary and secondary prevention for vulnerable populations, would reduce the acute care costs for these populations (16,17), as well as the RSSR variation across hospitals.
Full table
The case for a new approach to reduce HF readmissions
Prior to the HRRP, hospitals had no financial incentives to reduce readmissions because Medicare reimbursed hospitals through a fee-for-service model. Moreover, hospitals that reduced readmissions might even lose revenues unless they could fill unused beds with other patients (18). During the period 2010–2012, after the program was announced but before penalties were implemented, the readmission rates decreased markedly. After 2012, however, the decrease slowed (19). For HF, the 30-day risk adjusted readmission rate declined from 23.5% in 2008 to 21.4% in 2014 (20). The race-based gap between whites and blacks also narrowed, with a significantly greater decline among blacks than among whites (21). Overall, however, the readmission reduction was modest, while concerns were increasing about the HRRP’s unintended consequences, such as replacing inpatient admissions with observation stays and delaying readmissions beyond the 30-day period. These changes, if true, could impact health outcomes, especially for HF patients. HF involves multiple comorbidities, such as worsening of renal function, sleep-disordered breathing, hypertension, atrial fibrillation, type II diabetes, and others (22-24). This complexity makes HF clinical outcomes more sensitive if there are delays in hospital admissions or readmissions. Indeed, recently there have been several reports on possible increase in mortality rates associated with the HRRP implementation for HF patients (25-28).
Reducing the rates of readmissions generally requires considerable resources. Hospitals are more likely to allocate these resources for revenue generating activities than for readmission reductions despite the large HRRP penalties. There are two main reasons: (I) it is almost impossible for a hospital to predict whether or not it would be penalized by the HRRP. CMS uses a complex formula to estimate the excess readmission rate (ERR) for each hospital. This involves a benchmarking procedure which makes each hospital’s penalty dependent on the performance of the other hospitals. Therefore, reducing the risk of penalty becomes a moving target for each hospital; (II) much of the observed hospital readmission rates remain unexplained by the case-mix adjustments used in the ERR calculations. The final penalties are highly dependent on the patients that a hospital receives over the evaluation period, another consideration largely out of a hospital’s control (29). These uncertainties may reduce the effect of the HRRP on a hospital’s incentives to plan for readmission reduction (30).
Overall, analysis of the first five years of the program has indicated that for many hospitals, the HRRP leads to persistent penalization and limited capacity to reduce penalty burden (31). As a result, new approaches and alternative structures are needed to avoid persistent penalization, while still motivating reductions in hospital readmissions (31,32). Many hospitals have incurred hundreds of thousands of dollars in penalties, whereas the worst-performing hospitals have incurred millions of dollars in penalties (31). Furthermore, among fee-for-service Medicare beneficiaries discharged after HF hospitalization, implementation of the HRRP was temporally associated with a reduction in 30-day and 1-year readmissions but an increase in 30-day and 1-year mortality (25). Other independent investigations have also suggested that the HRRP implementation was associated with an increase in mortality after HF hospitalization, prompting reconsideration of the HRRP in HF (26-28).
Employer self-insurance: a new pathway to readmission reduction
From a standpoint of incentives, it is important that those who pay for prevention also benefit from it financially (33). When a hospital pays to prevent readmissions and is successful, it leads to loss of revenue under the fee-for-service payment method (unless the hospital can fill its beds with other patients for whom they receive higher net returns). Through alternative payments, such as Accountable Care Organizations (ACOs) or bundled payments, this may be corrected. We propose employer self-insurance as another mechanism that could provide financial rationale for increased investment in readmission reduction by a hospital.
Self-insurance is already accepted by the majority of large employers as a strategy to control the rise in their healthcare expenditures. More than half of colleges and universities self-insure the health care coverage they offer to their employees, i.e., pay for their own employees’ health expenses rather than buy insurance from insurance companies. Being self-insured has tax benefits, and it incorporates provider network solutions, wellness programs and disease management programs. Although these components are expected to reduce the risk of employees’ utilization of high-cost healthcare services, economic literature shows that the results of the wellness programs are mixed. At least in the short to medium term, wellness programs, which are essentially preventive care, are not likely to moderate the growing medical expenditure (34). Furthermore, specific interventions would still be necessary to reduce readmissions especially for a complex condition like HF. The design and implementation of these HF readmission reduction interventions would vary among universities and hospitals, but the key is that they would become available not only to the university employees and retirees, but to all patients. When effective, these readmission reduction interventions would lead to reduced medical costs for the employer much faster (i.e., within a 30-day period), than most of the wellness programs which, at best, would take years.
For a hospital that is a part of a self-insured university, reducing readmission rates would not only reduce the risk of an HRRP penalty, it also would lead to net revenues through two additional mechanisms: (I) avoided readmissions could lead to savings for the university due to averted rehospitalization costs for its employees and retirees. The university could share these savings with the hospital; and (II) the hospital could fill beds currently occupied by readmitted patients with new admissions who have higher contribution margins (i.e., revenues minus costs) than the readmissions. These key effects, however, have not been studied when it comes to increased incentives due to self-insurance. A study based on actual hospital data, combined with microsimulations and scenario analysis involving self-insurance could provide strong economic rationale for increased investment in readmission reduction by a hospital.
Discussion
US health care expenditures are believed to be unsustainable. The 2017 report of the Boards of Trustees of the Federal Hospital Insurance and Federal Supplementary Medical Insurance Trust Funds has projected that Medicare’s Hospital Insurance (HI) trust fund will remain solvent—i.e., able to pay 100% of the costs of the hospital insurance coverage that Medicare provides—through 2029. In 2029, when the HI trust fund is projected to be depleted, incoming payroll taxes and other revenues will be sufficient to pay 88% of Medicare hospital insurance costs (35). With the implementation of the HRRP, each year Medicare withholds hundreds of millions of dollars from hospital payments. For example, in 2018 under the HRRP, CMS is estimated to withhold $564 million in payments—up slightly from the $528 million withheld for FY 2017 (36). There are, however, other aspects to consider, even from the CMS perspective. The HRRP creates opportunities for hospitals to game the system, such as delaying admissions or readmissions. Furthermore, recent reports have raised concerns about potential increased mortality in HF patients as an unintended consequence (25-28).
An emerging body of economic studies indicate that the uncertainties associated with the HRRP penalization may reduce a hospital’s incentive to plan for and invest in readmission reduction (29,30). There is, however, a gap in the literature on hospital incentives to invest in readmission reduction beyond avoiding HRRP penalties. Hospitals have been investing in quality improvement (QI) interventions since the beginning of the HRRP, but neither the costs of implementation nor the potential savings associated with declines in hospitalization, have been systematically evaluated, especially for the long-term effect. Furthermore, it remains unclear whether effective readmission reduction interventions tend to produce net savings or losses for a hospital. In a systematic review and meta-analysis study on the economic evaluation of QI interventions designed to prevent hospital readmissions, only one of the 48 eligible studies had the hospital perspective, i.e., estimated the net financial impact of readmission reduction program on the hospital (37). This was a study on HF readmission prevention which found that the intervention significantly reduced adjusted 30-day readmission rates to the hospital, Baylor Medical Center Garland (BMCG) (by 48% during the post-intervention period). This was better than the secular reductions seen at all other facilities in the health care system. The intervention had little effect on length of stay or total 60-day direct costs for BMCG. However, under the current payment system, i.e., fee-for-service, the intervention reduced the hospital financial contribution margin, i.e., revenues minus costs, on average $227 for each Medicare patient with HF (38).
Incorporating the effect of being self-insured in the estimation of the financial impact of readmission reduction could demonstrate better financial outcomes for a hospital. Economics can help identify all the relevant costs and benefits of readmission reduction interventions from hospital perspective. This is necessary for determining the optimal level of investment, as well as finding the most cost-effective ways to reduce readmissions, while ensuring the highest safety and quality of life for the patients.
Conclusions
HF is a growing public health problem in the US and globally. It also has one of the highest hospital admission and readmission rates and costs. The existing US policies, such as the HRRP, may need to be reconsidered for HF due to its modest effect, and most importantly, its association with increased mortality in the HF Medicare population (24-27). One of the reasons for less than optimal hospital investment in preventing hospital admissions or readmissions is that the generated savings from prevention may not accrue to the hospital. In particular, readmission reduction interventions may add significant costs and may cause revenue loss for the hospital unless the unused hospital beds are filled with other patients (18).
Self-insured universities are already paying for prevention interventions through their wellness and chronic disease management programs. Incorporating readmission reduction interventions as a self-insurance feature could result in faster improved health outcomes and faster return on investment than the wellness programs, both for the university and the hospital. It is possible that some hospitals and academic centers already account for this factor. Increased investment in readmission reduction interventions, which would be justified due to self-insurance, is likely to have a spillover effect beyond the employees and the retirees of the university, i.e., other patient populations could benefit from it as well. To our knowledge, however, there are no empirical studies that have explored this question. Such studies could translate health economics principles into an innovative approach for reducing hospital readmissions.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Centers for Medicare and Medicaid Services. National Health Expenditures 2016 Highlights. Available online: https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/NationalHealthExpendData/Downloads/highlights.pdf, last accessed June 10, 2018.
- World Bank National Accounts Data, and OECD National Accounts Data Files. Available online: https://data.worldbank.org/indicator/NY.GDP.MKTP.CD, last accessed June 10, 2018.
- Newhouse JP. Medical care costs: how much welfare loss? J Econ Perspect 1992;6:3-21. [Crossref] [PubMed]
- Orszag PR, Emanuel EJ. Health care reform and cost control. N Engl J Med 2010;363:601-3. [Crossref] [PubMed]
- Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med 2009;360:1418-28. [Crossref] [PubMed]
- Kaboli PJ, Go JT, Hockenberry J, et al. Associations between reduced hospital length of stay and 30-day readmission rate and mortality: 14-year experience in 129 Veterans Affairs hospitals. Ann Intern Med 2012;157:837-45. [Crossref] [PubMed]
- Jiang HJ, Wier LM. HCUP Statistical Brief #89. Agency for Healthcare Research and Quality, Rockville, MD; Apr. 2010. All-Cause hospital readmissions among non-elderly Medicaid patients. Available online: http://www.hcup-us.ahrq.gov/reports/statbriefs/sb89.pdf
- Thorpe JH, Cascio T. Medicare Hospital Readmissions Reduction Program. Legal Notes. 2011;3(4):1–3. Available online: http://www.rwjf.org/content/dam/web-assets/2011/10/medicare-hospital-readmissions-reduction-program
- Yale New Haven Health Services Corporation - Center for Outcomes Research and Evaluation (YNHHSC/CORE). Hospital Characteristics. Variation in 30-day readmission rates across hospitals following hospitalizations for acute myocardial infarction, chronic obstructive pulmonary disease, heart failure, pneumonia, and acute ischemic stroke. CORE, Yale September 2017. The analyses upon which this publication was based were performed under Task Order Number HHSM-500-2013-13018I, Task Order HHSM-500-T0001, entitled, “Measure & Instrument Development and Support (MIDS): Development, Reevaluation, and Implementation of Outcome/Efficiency Measures for Hospitals and Eligible Clinicians,” sponsored by the Centers for Medicare & Medicaid Services, Department of Health & Human Services.
- Heidenreich PA, Albert NM, Allen LA, et al. Forecasting the impact of heart failure in the United States: a policy statement from the American Heart Association. Circ Heart Fail 2013;6:606-19. [Crossref] [PubMed]
- Benjamin EJ, Virani SS, Callaway CW, et al. American Heart Association Council on Epidemiology and Prevention Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics—2018 update: a report from the American Heart Association. Circulation 2018;137:e67-492. [Crossref] [PubMed]
- Fingar K, Washington R. Trends in hospital readmissions for four high-volume conditions, 2009–2013. HCUP Statistical Brief #196. November 2015. Agency for Healthcare Research and Quality, Rockville, MD. Available online: http://www.hcup-us.ahrq.gov/reports/statbriefs/sb196-Readmissions-Trends-High-Volume-Conditions.pdf
- Torio CM, Moore BJ. National Inpatient Hospital Costs: The most expensive conditions by payer, 2013. HCUP Statistical Brief #204. May 2016. Agency for Healthcare Research and Quality, Rockville, MD. Available online: https://www.hcup-us.ahrq.gov/reports/statbriefs/sb204-Most-Expensive-Hospital-Conditions.jsp
- Vest JR, Gamm LD, Oxford BA, et al. Determinants of preventable readmissions in the United States: A systematic review. Implement Sci 2010;5:88. [Crossref] [PubMed]
- Ziaeian B, Heidenreich PA, Xu H, et al. Medicare expenditures by race/ethnicity after hospitalization for heart failure with preserved ejection fraction. JACC Heart Fail 2018;6:388-97. [Crossref] [PubMed]
- Nasser SA, Ferdinand KC. Community outreach to African-Americans: Implementations for controlling hypertension. Curr Hypertens Rep 2018;20:33. [Crossref] [PubMed]
- Ferdinand KC, Orenstein D, Hong Y, et al. Health economics of cardiovascular disease: Defining the research agenda. CVD Prev Control 2011;6:91-100. [Crossref]
- James J. Health Policy Brief: Medicare Hospital Readmissions Reduction Program. Health Affairs. 2013;12.
- Zuckerman RB, Sehingold SH, Orav J, et al. Readmission, observation, and the Hospital Readmissions Reduction Program. N Engl J Med 2016;374:1543-51. [Crossref] [PubMed]
- Dharmarajan K, Wang Y, Lin Z, et al. Association of changing hospital readmission rates with mortality rates after hospital discharge. JAMA 2017;318:270-8. [Crossref] [PubMed]
- Figueroa JF, Zheng J, Orav EJ, et al. Medicare program associated with narrowing hospital readmission disparities between black and white patients. Health Aff (Millwood) 2018;37:654-61. [Crossref] [PubMed]
- Lüscher TF. Heart failure and comorbidities: renal failure, diabetes, atrial fibrillation, and inflammation. Eur Heart J 2015;36:1415-7. [Crossref] [PubMed]
- Ventura HO, Silver MA. Observations and reflections on the burden of hospitalizations for heart failure. Mayo Clin Proc 2017;92:175-8. [Crossref] [PubMed]
- Maréchaux S, Six-Carpentier MM, Bouabdallaoui N, et al. Prognostic importance of comorbidities in heart failure with preserved left ventricular ejection fraction. Heart Vessels 2011;26:313-20. [Crossref] [PubMed]
- Gupta A, Allen LA, Bhatt DL, et al. Association of the Hospital Readmissions Reduction Program implementation with readmission and mortality outcomes in heart failure. JAMA Cardiol 2018;3:44-53. [Crossref] [PubMed]
- Gupta A, Fonarow GC. The Hospital Readmissions Reduction Program—learning from failure of a healthcare policy. Eur J Heart Fail 2018. [Epub ahead of print]. [PubMed]
- Khera R, Pandey A, Ayers CR, et al. Contemporary epidemiology of heart failure in fee-for-service Medicare beneficiaries across healthcare settings. Circ Heart Fail 2017.10. [PubMed]
- Chatterjee P, Joynt Maddox KE. US national trends in mortality from acute myocardial infarction and heart failure: Policy success or failure? JAMA Cardiol 2018;3:336-40. [Crossref] [PubMed]
- Wilcock A, Escarce JJ, Huckfeldt PJ, et al. Luck of the draw: the role of chance in the assignment of Medicare readmission penalties. Paper presented at: Seventh Conference of the American Society of Health Economists (ASHEcon); June 11, 2018. Atlanta, GA. Available online: https://ashecon.confex.com/ashecon/2018/webprogram/Paper6647.html
- Zeiden E. How Hospitals Responded to the Financial Incentives of the HRRP. Paper presented at: Seventh Conference of the American Society of Health Economists (ASHEcon); June 11, 2018. Atlanta, GA.
- Thompson MP, Waters TM, Kaplan CM, et al. Most hospitals received annual penalties for excess readmissions, but some fared better than others. Health Aff (Millwood) 2017;36:893-901. [Crossref] [PubMed]
- Zhang DJ, Gurvich I, Van Mieghem JA, et al. Hospital Readmissions Reduction Program: An economic and operational analysis. Manag Sci 2016;62:3351-71. [Crossref]
- Katz MH. Interventions to decrease hospital readmission rates: Who saves? Who pays? Arch Intern Med 2011;171:1230-1. [Crossref] [PubMed]
- Danagoulian S. A health insurance plan with wellness features. Ph.D. Dissertation. Department of Economics. Cornell University. 2014. Available online: http://citeseerx.ist.psu.edu/viewdoc/download?doi=10.1.1.1019.6407&rep=rep1&type=pdf
- The Boards of Trustees, Federal Hospital Insurance and Federal Supplementary Medical Insurance Trust Funds. 2017 Annual Report of the Boards of Trustees of the Federal Hospital Insurance and Federal Supplementary Medical Insurance Trust Funds. Medicare Trustees Report. Available online: https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/ReportsTrustFunds/Downloads/TR2018.pdf
- Kaiser Health News. 2,573 hospitals will face readmission penalties this year. Is yours one of them? August 7, 2017. Available online: https://www.advisory.com/daily-briefing/2017/08/07/hospital-penalties
- Nuckols TK, Keeler E, Morton S, et al. Economic evaluation of quality improvement interventions designed to prevent hospital readmission: a systematic review and meta-analysis. JAMA Intern Med 2017;177:975-85. [Crossref] [PubMed]
- Stauffer BD, Fullerton C, Fleming N, et al. Effectiveness and cost of a transitional care program for heart failure: a prospective study with concurrent controls. Arch Intern Med 2011;171:1238-43. [Crossref] [PubMed]


