Management and weaning from mechanical ventilation in neurologic patients
Background
Brain injured (BI) patients such as traumatic brain injury (TBI), subarachnoid haemorrhage (SAH) intra-cranial haemorrhage or stroke are often admitted in the intensive care unit (ICU) for neurological surveillance (1). Whenever arousal is importantly impaired, mechanical ventilation (MV) becomes mandatory in order to protect the airway from aspiration and prevents hypoxemia and hypercapnia. These respiratory complications are major systemic factors of secondary brain insults, and thus impair the outcome (2). Patients with severe BI display a prolonged MV duration, compared to other ICU patients. In an observational multi-centre nationwide study (3), patients with BI displayed a high duration of MV compared to other ICU subgroups. These findings were witnessed in all types of BI injury: TBI, stroke and SAH compared to the general ICU population. Other studies in the neuro-ICU field (4,5) still suggested long duration of MV, although there was no comparison with the general ICU population. Although the management of MV is of daily concern for attending physicians, there is currently little data in patients undergoing severe BI. The weaning process of MV in these patients, once the neurological management acute phase is over, remains poorly described and the latest guidelines on the subject did not propose any specific recommendations in patients with BI (6). Recently, new data have highlighted specific extubation and weaning management of patients with TBI and SAH (7-9).
In this review, we will discuss the latest data about the MV management and potential new weaning strategies in patients with BI.
MV management
After BI, one of the priorities is to secure the airway when the Glasgow Coma Score (GCS) is ≤8 (2). Endotracheal intubation prevents aspiration and enables ventilatory management with MV. Second, in the first days following BI, hypoxemia and hyper/hypocapnia lead to secondary brain insults, which alter the outcome (10). Treatment of hypoxemia can be modulated via FiO2 to ensure a PaO2 target >60 mmHg (2). Moreover, PaO2 could be modulated with the help of PtiO2 monitoring in order to avoid cerebral ischemia (11,12). PaCO2 is the second respiratory parameter that must be controlled because it is a powerful determinant of cerebral blood flow. PaCO2 directly controls cerebral blood vessels dilation and contraction and has immediate effects on intra-cranial pressure (2). An adequate control of PaCO2 within a 35–45 mmHg range is a therapeutic target all along the course of MV during BI (2). Nonetheless, the latest guidelines in TBI patients (2) did not propose any recommendation to manage PaCO2, and both tidal volume and respiratory rates are left at the physician’s discretion. The fear of hypercapnia in these patients, has lead practitioners to set the tidal volume at 9 mL/kg of ideal predicted body weight in patients with BI (3). Moreover, in this large observational study, a significantly lower proportion of patients with BI received protective ventilation compared to the non-neurologic patients (3). The respiratory management of patients with BI could nonetheless bear major clinical impact on the outcome. High tidal volume leads to ventilator-induced lung injury (13), and in neuro-ICU studies high tidal volume is associated with an increased rate of acute respiratory distress syndrome (ARDS) which alters patient’s outcome (14,15).
Recently, the safety and efficacy of protective ventilation in BI patients was tested in two before-after studies. The first study was monocentric in 2 ICUs and included 499 patients with TBI, SAH and stroke (5). The bundle of care associated a protective ventilation strategy [tidal volume between 6–8 mL/kg of ideal predicted bodyweight and positive end-expiratory pressure (PEEP) >3 cmH2O] and early extubation with a GCS ≥10 (5). There was a significant increase in the number of ventilatory-free days during the intervention period. However, another before-after multi-centre study performed in a large population of patients with BI did no confirm these results (4). Indeed, protective ventilation (≤7 mL/kg of ideal predicted body weight and a PEEP between 6–8 cmH2O) associated with early extubation in 749 BI patients showed no differences in the number of ventilatory-free days in the intervention period. However, in the sub-group of patients receiving both protective ventilation and early extubation there was a significant improvement of the number of ventilatory-free days and the mortality rate. In both studies (4,5), protective ventilation did not alter the outcome and did not bear clinically relevant effects on intracranial pressure. In the end, it remains mandatory to monitor the level of PaCO2 within normal ranges. These new data highly suggest that protective ventilation with a moderate tidal volume (6–8 mL/kg of ideal body weight) could be safely applied in BI patients and could bear significant positive effects, while keeping PaCO2 in normal range by adjusting the respiratory rate as recommended by the current international guidelines (2).
Another issue regarding the ventilatory settings is the level of PEEP that should be set: PEEP increases the intra-thoracic pressure and may impair central venous return, leading to increased intracranial pressure. However, this assumption has been poorly documented in the ICU literature. One study driven in a small sample of nine patients with BI (16), showed a positive correlation between PEEP and intra-cranial pressure. In another study including patients with SAH (17), PEEP impaired cerebral blood flow but through a mean arterial pressure decreased and without modifying intracranial pressure. Considering these data, it was therefore advocated to use a low or zero PEEP in patients with BI to avoid intracranial pressure increase. Pelosi et al. confirmed that a vast majority of patients with BI were delivered a PEEP ≤5 cmH2O (3). The concept of “low/zero PEEP” was challenged by recent data showing the safety of moderate levels of PEEP. In a pilot prospective study performed in 20 patients with TBI, the results suggested that a PEEP increase to 15 cmH2O could have beneficial effects on brain tissue oxygenation evaluated with PtiO2 (18). Our group confirmed that PEEP >5 cmH2O did not alter the intracranial pressure in severe BI patients (4,5). In definite, it seems that the zero-PEEP policy should be abandoned in neuro-ICUs and that an increase of PEEP could be safely applied in patients with BI, provided normovolemia in patients.
Weaning from MV and extubation
In series of BI patients, the extubation failure rate was up to 38% (19), but other descriptive studies also suggest that the extubation failure rate is high in this specific ICU population (7). Like for MV management, the latest guidelines on the subject did not describe the weaning management of BI patients (6). Observational studies also suggest that extubation is often delayed, probably because of the physician’s inability to accurately evaluate the level of arousal during the recovery phase (20). The burden of both delayed extubation and extubation failure is high in patients with BI: nosocomial pneumonia, longer MV duration, increased ICU length of stay and higher mortality (7,8,20).
The level of arousal to safely perform extubation remains controversial. Coplin et al. have pointed out that delaying extubation in order to obtain sustained neurological improvement during the recovery phase, would not guarantee successful extubation (20). Such strategy is also associated with morbidity (20). A algorithm-based extubation (GCS ≥8 with audible cough during suctioning) was tested in a randomized-controlled study, and improved the extubation success rate (21). Namen et al. showed that a GCS of 8 had the highest area under the receiver operating curve for predicting successful extubation (19). However, all authors do not retrieve the GCS as a predictive factor of successful extubation (8,9). A possible explanation is that the GCS has never been validated in intubated patients, and it should be kept in mind that the quantification of the verbal component is impossible and often arbitrarily scored. This could explain why the GCS used alone has been inconsistently pointed out as a factor of extubation success.
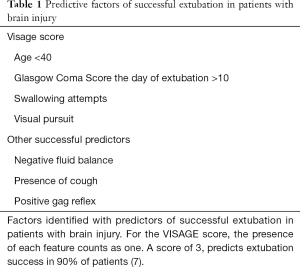
Recent data have evaluated new physical features compatible with successful extubation in patients with severe BI. In a multi-centric study in 437 patients, age <40 years old, visual pursuit, attempts of swallowing and a GCS >10 on the day of extubation were predictors of successful extubation (7). Based on these items the VISAGE score was built. When 3 items are present, the score predicts more than 90% of extubation success. Other observational studies have found similar results for these clinical signs [visual pursuit and preserved upper airway reflexes (8), younger age (9)], but also new factors [negative fluid balance and the presence of cough (9,22)] were described as good predictors of extubation success (Table 1). Overall, it seems that the presence sub-optimal consciousness level with at least one functional airway operators help to decrease the rate of delayed extubation without inducing a higher rate of extubation failure.
Full table
Several issues still remain regarding extubation success. All these cohorts creating new scores of extubation success or failure lack external validation, which renders the generalizability of the results questionable. Second, although the elaboration of bundles of care are mandatory to improve outcomes (23), they remain complicated to apply at bedside in a daily practice (4). Further studies could be driven to confirm the findings of the latest studies, in order to confirm which markers are predictive of successful extubation.
The indications and timing of tracheostomy after BI
Tracheostomy appears an interesting therapeutic alternative in the case of complicated weaning process like in patients with BI. In a monocentric retrospective study in a TBI population (24), a propensity score analysis suggested a benefit of early tracheostomy in the first 5 days after intubation, with fewer pneumonia, lower MV duration and ICU length of stay. In a second retrospective study performed in a large multi-centre data-bases (25), the propensity score analysis also favoured early tracheostomy. The mortality rate was similar between patients with early and late tracheostomy in both studies. The main drawback of non-specific databases studies, is that the indication of tracheostomy remains unknown and it is hard to select the best candidates for early tracheostomy in daily practice. In one randomized-controlled study with patients with stroke and SAH, early tracheostomy did not result in a reduction of the ICU length of stay but resulted in lower mortality (26). These results should be cautiously interpreted since mortality was a secondary outcome.
To this day there are no guidelines regarding the management of tracheostomy in patients with BI. Tracheostomy could be a part of therapeutic arsenal be should definitely be performed according to written local protocols.
Conclusions
Patients undergoing BI from trauma or intra-cranial haemorrhage display a high prevalence of respiratory complications longer durations of MV and high rates of extubation failure, compared to other ICU patients. New data about MV management have been tested in the neuro-ICU setting. It is now clear that PEEP has minor effects on cerebral perfusion pressure. Protective ventilation with low tidal volumes (6–8 mL/kg of ideal body weight), could be safely applied to BI patients, but its benefits has not been formally proven. Extubation remains challenging in the neuro-ICU setting. Very simple clinical signs like visual pursuit, cough, swallowing have been described as good predicting factors of successful extubation and could be useful in guiding extubation. Finally, the exact timing and indications of tracheostomy remains uncertain and should be better delineated.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Esteban A, Anzueto A, Frutos F, et al. Characteristics and outcomes in adult patients receiving mechanical ventilation: a 28-day international study. JAMA 2002;287:345-55. [Crossref] [PubMed]
- Carney N, Totten AM, O'Reilly C, et al. Guidelines for the Management of Severe Traumatic Brain Injury, Fourth Edition. Neurosurgery 2017;80:6-15.
- Pelosi P, Ferguson ND, Frutos-Vivar F, et al. Management and outcome of mechanically ventilated neurologic patients*. Crit Care Med 2011;39:1482-92. [Crossref] [PubMed]
- Asehnoune K, Mrozek S, Perrigault PF, et al. A multi-faceted strategy to reduce ventilation-associated mortality in brain-injured patients. The BI-VILI project: a nationwide quality improvement project. Intensive Care Med 2017;43:957-70. [Crossref] [PubMed]
- Roquilly A, Cinotti R, Jaber S, et al. Implementation of an evidence-based extubation readiness bundle in 499 brain-injured patients. a before-after evaluation of a quality improvement project. Am J Respir Crit Care Med 2013;188:958-66. [Crossref] [PubMed]
- Boles J-M, Bion J, Connors A, et al. Weaning from mechanical ventilation. Eur Respir J 2007;29:1033-56. [Crossref] [PubMed]
- Asehnoune K, Seguin P, Lasocki S, et al. Extubation Success Prediction in a Multicentric Cohort of Patients with Severe Brain Injury. Anesthesiology 2017;127:338-46. [Crossref] [PubMed]
- Godet T, Chabanne R, Marin J, et al. Extubation Failure in Brain-injured Patients: Risk Factors and Development of a Prediction Score in a Preliminary Prospective Cohort Study. Anesthesiology 2017;126:104-14. [Crossref] [PubMed]
- McCredie VA, Ferguson ND, Pinto RL, et al. Airway Management Strategies for Brain-injured Patients Meeting Standard Criteria to Consider Extubation. A Prospective Cohort Study. Ann Am Thorac Soc 2017;14:85-93. [Crossref] [PubMed]
- Rosenfeld JV, Maas AI, Bragge P, et al. Early management of severe traumatic brain injury. Lancet 2012;380:1088-98. [Crossref] [PubMed]
- Longhi L, Pagan F, Valeriani V, et al. Monitoring brain tissue oxygen tension in brain-injured patients reveals hypoxic episodes in normal-appearing and in peri-focal tissue. Intensive Care Medicine 2007;33:2136-42. [Crossref] [PubMed]
- Okonkwo DO, Shutter LA, Moore C, et al. Brain Oxygen Optimization in Severe Traumatic Brain Injury Phase-II. Crit Care Med 2017;45:1907-14. [Crossref] [PubMed]
- Gattinoni L, Protti A, Caironi P, et al. Ventilator-induced lung injury: The anatomical and physiological framework. Crit Care Med 2010;38:S539-48. [Crossref] [PubMed]
- Mascia L, Zavala E, Bosma K, et al. High tidal volume is associated with the development of acute lung injury after severe brain injury: an international observational study. Crit Care Med 2007;35:1815-20. [Crossref] [PubMed]
- Bellani G, Laffey JG, Pham T, et al. Epidemiology, Patterns of Care, and Mortality for Patients With Acute Respiratory Distress Syndrome in Intensive Care Units in 50 Countries. JAMA 2016;315:788. [Crossref] [PubMed]
- Zhang XY, Yang ZJ, Wang QX, et al. Impact of positive end-expiratory pressure on cerebral injury patients with hypoxemia. Am J Emerg Med 2011;29:699-703. [Crossref] [PubMed]
- Muench E, Bauhuf C, Roth H, et al. Effects of positive end-expiratory pressure on regional cerebral blood flow, intracranial pressure, and brain tissue oxygenation*. Crit Care Med 2005;33:2367-72. [Crossref] [PubMed]
- Nemer SN, Caldeira JB, Santos RG, et al. Effects of positive end-expiratory pressure on brain tissue oxygen pressure of severe traumatic brain injury patients with acute respiratory distress syndrome: A pilot study. J Crit Care 2015;30:1263-6. [Crossref] [PubMed]
- Namen AM, Ely EW, Tatter SB, et al. Predictors of successful extubation in neurosurgical patients. Am J Respir Crit Care Med 2001;163:658-64. [Crossref] [PubMed]
- Coplin WM, Pierson DJ, Cooley KD, et al. Implications of extubation delay in brain-injured patients meeting standard weaning criteria. Am J Respir Crit Care Med 2000;161:1530-6. [Crossref] [PubMed]
- Navalesi P, Frigerio P, Moretti MP, et al. Rate of reintubation in mechanically ventilated neurosurgical and neurologic patients: Evaluation of a systematic approach to weaning and extubation. Crit Care Med 2008;36:2986-92. [Crossref] [PubMed]
- Dos Reis HFC, Gomes-Neto M, Almeida MLO, et al. Development of a risk score to predict extubation failure in patients with traumatic brain injury. J Crit Care 2017;42:218-22. [Crossref] [PubMed]
- Rhodes A, Phillips G, Beale R, et al. The Surviving Sepsis Campaign bundles and outcome: results from the International Multicentre Prevalence Study on Sepsis (the IMPreSS study). Intensive Care Med 2015;41:1620-8. [Crossref] [PubMed]
- Hyde GA, Savage SA, Zarzaur BL, et al. Early tracheostomy in trauma patients saves time and money. Injury 2015;46:110-14. [Crossref] [PubMed]
- Alali AS, Scales DC, Fowler RA, et al. Tracheostomy timing in traumatic brain injury: a propensity-matched cohort study. J Trauma Acute Care Surg 2014;76:70-6; discussion 76-8. [Crossref] [PubMed]
- Bösel J, Schiller P, Hook Y, et al. Stroke-Related Early Tracheostomy Versus Prolonged Orotracheal Intubation in Neurocritical Care Trial (SETPOINT): A Randomized Pilot Trial. Stroke 2013;44:21-8. [Crossref] [PubMed]


