High prevalence and seasonal variation of hypovitaminosis D in patients scheduled for lower extremity total joint arthroplasty
Introduction
Vitamin D insufficiency and deficiency have been demonstrated in high prevalence in populations around the world and represent a major health concern (1). A recent discovery that most tissues and cells in the body have a vitamin D receptor and that some of these cells possess enzymes required to convert the primary circulating form of vitamin D, 25-hydroxyvitamin D, to the active form, 1,25-dihydroxyvitamin D has provided new insights into the function of this vitamin (2). Besides its central physiological role in calcium homeostasis and bone mineralization, vitamin D acts as a modulator of cell growth, neuromuscular function, and immunomodulation. In addition, many studies are investigating the role that vitamin D may play in decreasing the risk of many chronic illnesses, including cancers, autoimmune diseases, and infectious diseases (3-6).
Several studies performed in the orthopaedic field have identified a widespread hypovitaminosis D in patients scheduled for surgery (6-19). However, the etiology and risks factors linked to low levels of vitamin D in patients scheduled for elective lower extremity total joint arthroplasty (TJA) have not been well-characterized. This has become of increased interested after reports have linked the low levels of vitamin D with potential negative effects on functional recovery after surgery and an increased risk of developing infection (11,20,21). However, although an association between low vitamin D levels and potential negative effects on patients’ outcomes have been shown in some studies, there is little work demonstrating the risk factors associated with low vitamin D levels and the seasonal variation in patients scheduled for elective lower extremity TJA.
Therefore, the primary purposes of this study were: (I) to assess the prevalence of pre-operative vitamin D deficiency and insufficiency in patients undergoing primary TJA; (II) to evaluate the risk factors for hypovitaminosis D; and (III) to determine seasonal variation in such population.
Methods
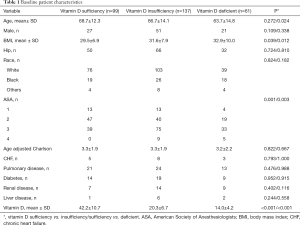
After institutional review board approval was obtained, a total of 905 patients who underwent primary TJA, at a single institution by a single orthopaedic surgeon, from January 1st 2006 to December 31st 2016 were identified from a query of the electronic medical database. After a review of their charts, we identified 226 [116 primary total hip arthroplasties (THAs) and 120 primary total knee arthroplasty patients (TKA)], who had a vitamin D measurement in their preoperative evaluation (Table 1). Demographics, comorbidities, and perioperative data were retrospectively collected from electronic medical records.
Full table
All patients were treated at the same location, which has a latitude of 41.5, and longitude of −81.6 (GPS coordinates of 41° 30' N and 81° 40' W—North Mid-West region of the United States). Specifically, we recorded vitamin D level screening (serum 25-(OH)D levels) at the time of preoperative evaluation (within the range of 1 year before the date of the surgery) for patients scheduled for TJA. Currently, there is no universally accepted classification of vitamin D levels, therefore, status was categorized based on two of the most often used cut-off points No consensus exists on the definition of vitamin D deficiency or the optimal level of total serum 25-hydroxyvitamin D [25-(OH)D] (the major form of vitamin D that circulates in the body). Depending on which cut point is used [usually <50 or <75 nmol/L (<20 or <30 ng/mL)]. We therefore defined vitamin D status categories non-mutually as: vitamin D sufficiency as a serum 25-(OH)D level greater than 30 ng/mL, vitamin D insufficiency as <30 ng/mL and vitamin D deficiency as < 20 ng/mL. The following variables were also recorded: age, sex, race, body mass index (BMI), American Society of Anesthesiologists’ (ASA) score and the age-adjusted Charlson comorbidity index (CCI) (22,23). All data collected was done by patients’ electronic medical record retrospective chart review by one of the authors (NS Piuzzi).
Differences in the continuous variables were analyzed using Students t-test or analysis of variance (ANOVA). Bonferronni method was used to do pairwise comparisons between multiple groups when more than one group was present. Fisher’s exact tests or Chi-squared tests were used to assess the difference in proportions. Separate comparisons were made between sufficient and insufficient groups, and sufficient and deficient groups. A multivariable logistic regression model was created to identify the independent risk factors for deficient and insufficient vitamin D levels compared to sufficient levels. Variables which were found to be significant at an alpha level of 0.150 in the univariate analysis were used to create the initial model. The predictive variables included in the final model were selected by stepwise backward elimination using P<0.05 as the cut-off for inclusion. Statistical analysis was performed using Stata Statistical Software: Release 12 (College Station, Texas, US: StataCorp LP).
Results
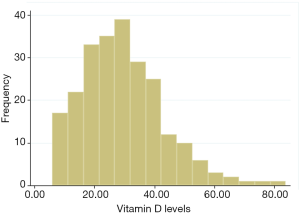
The mean vitamin D serum level for all patients was 29.5±13.8 ng/mL (range, 5.9 to 83.9 ng/mL) (Figure 1). There were 99/226 (43.8%) patients in the vitamin D sufficient group (mean vitamin D level 42.2±10.7 ng/mL, range, 30.1 to 83.9 ng/mL), 137/226 patients (60.6%) in the insufficient group (<30 ng/mL) (mean vitamin D 20.3±6.7 ng/mL, range, 20.2 to 29.9 ng/mL), of which 61/226 (26.9%) were in the deficient group (<20 ng/mL) (mean vitamin D level 14.0±4.2 ng/mL, range, 5.9 to 19.9 ng/mL).
The baseline characteristics of patients in the sufficient and insufficient/deficient groups are shown in Table 1. Body mass index (P=0.039) and ASA (P=0.001) were associated with vitamin D insufficiency, while age (P=0.024), BMI (P=0.012) and ASA (P=0.003) were associated with vitamin D deficiency. On multivariate analysis, an ASA score ≥3 was an independent risk factor for vitamin D insufficiency [OR =2.44 (1.44–4.14), P<0.001], while ASA ≥3 [OR =3.57 (1.73–7.35), P<0.001] and younger age [OR =0.96 (0.93–0.99), P=0.002] were independent risk factors for vitamin D deficiency. BMI failed to be an independent risk factor for vitamin D deficiency (P=0.280) or insufficiency (P=0.095), and hence was eliminated during stepwise elimination. Other factors assessed in the study like gender, race, joint type and comorbidities failed to demonstrate any association with vitamin D deficiency or insufficiency (P>0.05) (Table 1).
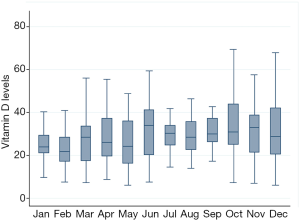
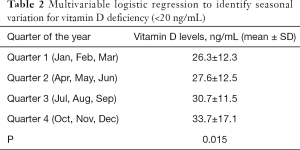
The levels of vitamin D had significant quarterly seasonal changes (P=0.015) (Table 2). The lowest mean levels of Vitamin D were found in quarter 1 (January, February, and March), while the highest mean levels were found in quarter 4 (October, November, and December) (quarter 1 vs. quarter 4 were similar: 33.7±17.1 vs. 26.3±12.3, P=0.019) (Figure 2).
Full table
Discussion
There have been several studies published recently demonstrating a high prevalence of hypovitaminosis D in patients who are scheduled to undergo orthopaedic surgery (6-19). In addition, some reports have shown that the low levels of vitamin D may be associated with potential negative effects on functional recovery after surgery, and increased risk of developing infection (11,20,21). However, what patients are at increased risk of having low vitamin D levels prior to their elective surgery has not been well-characterized. In addition, there is a paucity of reports demonstrating the relationship between low vitamin D levels and the time of the year when TJA surgeries are scheduled. Therefore, the purpose of this study was to assess the prevalence, evaluate the risk factors, and to determine seasonal variation of hypovitaminosis D in patients scheduled to undergo lower extremity TJA. We have identified a high prevalence of vitamin D insufficiency and deficiency in this patient population. Specifically, this was more commonly present in patients who are younger, have high BMI, high ASA scores, and were sampled in January, February, and March. Furthermore, we were able to identify that an ASA score ≥3 was associated with vitamin D insufficiency, while ASA ≥3 and younger age were associated with vitamin D deficiency.
This study is not without limitations. The effects of vitamin D prescribed supplementation were not assessed, nor did we evaluate the counter use of vitamin D supplements (e.g., pharmacies, drug stores, and supermarkets). The daily sunlight exposure of the patients was not determined, nor did we assessed how many patients treated did not reside in the geographical area. The vitamin D levels were not correlated with clinical outcomes of the surgery. Additionally, the study has all the limitations associated with its retrospective design and chart review method. Also, the majority of the patients did not have a vitamin D measurement and might have introduced a sampling bias in the study, which limit the estimation of prevalence. Furthermore, we the decision to measure vitamin D levels might have been random, and patient that were already on vitamin D supplementation might have not been reassessed. Nevertheless, the relatively large number of patients, and sizeable number of events of low serum vitamin D level encounter provided important data on this unsolved clinical findings, and associated risk factors. Finally, to our knowledge, there is not a study with this type of information on such particular cohort of patients undergoing TJA available in the literature.
Several studies have found similarly high rates of hypovitaminosis D in general orthopaedic populations. Maier et al. (24) measured vitamin D levels of 1,119 consecutive patients who were admitted under an orthopaedic service in a region of Germany, latitude (50° N). The authors found low vitamin D levels across all orthopaedic subspecialties with a mean vitamin D value of 17.3 ng/mL. Additionally, they reported this to be greater during winter (fewer sunshine hours), but did not find vitamin D levels to vary according to age, sex, and disease. Similarly, a study by Bogunovic et al. (25) further corroborated the higher prevalence of vitamin D deficiency in a study of patients scheduled to undergo orthopaedic surgery, performed in New York (40° N). In this study, they found that patients with darker skin tones (African-Americans and Hispanics) were 5.5 times more likely to have low vitamin D levels when compared to lighter skin tones (Whites and Asians) (P<0.001). Additionally, corroborating our findings, patients aged 51 to 70 years were 35% less likely to have low vitamin-D levels than patients between the ages of 18 and to 50 years (P=0.018). In a study of 206 healthy Hungarian males over 50 years of age, Bhattoa et al. (26) found a high prevalence of hypovitaminosis D (52.9%), and lower levels of vitamin D during their winter. Several other studies identified a high prevalence of hypovitaminosis D in orthopaedic populations as well (6-19,27).
Although many studies have described a high prevalence of hypovitaminosis D in orthopaedic population, only a few studies have identified potential risk factors in patients scheduled for elective TJA specifically. In a study of 62 consecutive patients scheduled for THA performed by Nawabi et al. (12), patients who had vitamin D deficiency had lower pre-operative Harris hip scores (32 vs. 42 points; P=0.018) and were less likely to have excellent outcomes (5 vs. 30 patients; P=0.038). In a study of 109 consecutive patients undergoing total hip, knee, or shoulder arthroplasty Maier et al. (21) demonstrated significantly lower levels of vitamin D in patients who had periprosthetic joint infections, when compared to patients undergoing primary arthroplasty (13.29 vs. 19.46 ng/mL; P<0.001). Although many of these studies describe an association, they do not prove causal relationship between low vitamin D levels and poor outcomes. Furthermore, although the definitive prevalence of hypovitaminosis D and the potential detrimental effect it could have on patient outcomes following TJA is still to be determined, there is a need to determine cost-benefit analysis of universal screening versus vitamin D supplementation in TJA preoperative guidelines. Since the most-effective method of improving patient care and reducing readmissions is to avoid complications (28-34), special consideration towards vitamin D assessment should be taken in the winter months, or immediate months after this season.
In patients who are found to be vitamin D insufficient or deficient, vitamin D supplementation has been shown to effectively improve vitamin D levels. There are multiple supplementation strategies, which vary depending on the cause of deficiency (e.g., decreased intake, low absorptive capacity, reduced sun exposure) and the patient. However, a standard regimen usually consists of a weekly dose of 50,000 IU vitamin D2 for 6 to 8 weeks, followed by every other week or every 4 weeks indefinitely (2). Alternatively, a daily supplementation with 1,000 IU of vitamin D3 or 3,000 IU of vitamin D2, which can be found over-the-counter in most pharmacies, is also effective if the initial serum vitamin D levels are above 10 to 20 ng/mL (2). Additionally, for patients taking vitamin D, a daily supplemental calcium dose of 1,000 to 1,300 mg is also recommended. Vitamin D levels should be reassessed 3 to 5 months after start of the therapy (35,36).
Conclusions
Patients scheduled for lower extremity TJA in a region of the United States, whose latitude is 41° 30' N, have an overall high prevalence of vitamin D insufficiency (60%) and deficiency (27%). Based on our findings, due to higher risk of hypovitaminosis D, particular attention should be placed in patients with an ASA score ≥3, and scheduled during winter season. Further research is needed to establish the definitive prevalence of hypovitaminosis D and the potential detrimental effect it could have on patient outcomes following TJA. Furthermore, cost-benefit analysis must determine if universal screening or treatment should be included in TJA preoperative guidelines. In summary, although we were able to identify several risk factors associated with low vitamin D insufficiency and deficiency, the effect of these conditions on patient outcomes following TJA remains to be determined, as there is a paucity of studies demonstrating causal relationship between low vitamin D levels and poor patient outcomes.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: This article received institutional review board approval (IRB 17-218) and written informed consent was waived.
References
- Mithal A, Wahl DA, Bonjour JP, et al. Global vitamin D status and determinants of hypovitaminosis D. Osteoporos Int 2009;20:1807-20. [Crossref] [PubMed]
- Holick MF. Vitamin D deficiency. N Engl J Med 2007;357:266-81. [Crossref] [PubMed]
- Grant WB, Holick MF. Benefits and requirements of vitamin D for optimal health: A review. Altern Med Rev 2005;10:94-111. [PubMed]
- Hollis BW. Circulating 25-Hydroxyvitamin D Levels Indicative of Vitamin D Sufficiency: Implications for Establishing a New Effective Dietary Intake Recommendation for Vitamin D. J Nutr 2005;135:317-22. [Crossref] [PubMed]
- Thomas MK, Lloyd-Jones DM, Thadhani RI, et al. Hypovitaminosis D in Medical Inpatients. N Engl J Med 1998;338:777-83. [Crossref] [PubMed]
- Waldron JL, Ashby HL, Cornes MP, et al. Vitamin D: a negative acute phase reactant. J Clin Pathol 2013;66:620-2. [Crossref] [PubMed]
- Laslett LL, Quinn S, Burgess JR, et al. Moderate vitamin D deficiency is associated with changes in knee and hip pain in older adults: a 5-year longitudinal study. Ann Rheum Dis 2014;73:697-703. [Crossref] [PubMed]
- Mabey T, Singhatanadgige W, Yingsakmongkol W, et al. Vitamin D and spine surgery. World J Orthop 2016;7:726. [Crossref] [PubMed]
- Maier GS, Horas K, Seeger JB, et al. Vitamin D insufficiency in the elderly orthopaedic patient: an epidemic phenomenon. Int Orthop 2015;39:787-92. [Crossref] [PubMed]
- Maier GS, Jakobs P, Roth KE, et al. Is there an epidemic vitamin D deficiency in German orthopaedic patients? Clin Orthop Relat Res 2013;471:3029-35. [Crossref] [PubMed]
- Maniar RN, Patil AM, Maniar AR, et al. Effect of Preoperative Vitamin D Levels on Functional Performance after Total Knee Arthroplasty. Clin Orthop Surg 2016;8:153-6. [Crossref] [PubMed]
- Nawabi DH, Chin KF, Keen RW, et al. Vitamin D deficiency in patients with osteoarthritis undergoing total hip replacement: a cause for concern? J Bone Joint Surg Br 2010;92:496-9. [Crossref] [PubMed]
- Pascual-Garrido C, Angeline ME, Ma R, et al. Low Levels of Vitamin D have a Deleterious Effect on the Articular Cartilage in a Rat Model. HSS J 2016;12:150-7. [Crossref] [PubMed]
- Peersman G, Bellemans J, Richart T. Is oral vitamin D a risk factor for prosthetic loosening? Acta Orthop Belg 2009;75:2-7. [PubMed]
- Rodriguez WJ, Gromelski J. Vitamin D status and spine surgery outcomes. ISRN Orthop 2013;2013. [Crossref] [PubMed]
- Unnanuntana A, Rebolledo BJ, Gladnick BP, et al. Does Vitamin D Status Affect the Attainment of In-Hospital Functional Milestones After Total Hip Arthroplasty? J Arthroplasty 2012;27:482-9. [Crossref] [PubMed]
- Unnanuntana A, Saleh A, Nguyen JT, et al. Low vitamin D status does not adversely affect short-term functional outcome after total hip arthroplasty. J Arthroplasty 2013;28:315-22.e2. [Crossref] [PubMed]
- Wang XG, Yang B, Wang YH, et al. Serum Levels of 25-hydroxyvitamin D and Functional Outcome in Older Patients with Hip Fracture. J Arthroplasty 2015;30:891-4. [Crossref] [PubMed]
- Zhang FF, Driban JB, Lo GH, et al. Vitamin D Deficiency Is Associated with Progression of Knee Osteoarthritis. J Nutr 2014;144:2002-8. [Crossref] [PubMed]
- Lavernia CJ, Villa JM, Iacobelli DA, et al. Vitamin D insufficiency in patients with THA: Prevalence and effects on outcome. Clin Orthop Relat Res 2014;472:681-6. [Crossref] [PubMed]
- Maier GS, Horas K, Seeger JB, et al. Is there an association between periprosthetic joint infection and low vitamin D levels? Int Orthop 2014;38:1499-504. [Crossref] [PubMed]
- American Society of Anesthesiologists. New classification of physical status. Anesthesiology 1963;24:111.
- Charlson ME, Pompei P, Ales KL, et al. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 1987;40:373-83. [Crossref] [PubMed]
- Maier GS, Jakob P, Horas K, et al. Vitamin D deficiency in orthopaedic patients: A single center analysis. Acta Orthop Belg 2013;79:587-91. [PubMed]
- Bogunovic L, Kim AD, Beamer BS, et al. Hypovitaminosis D in Patients Scheduled to Undergo Orthopaedic Surgery. A Single-Center Analysis. J Bone Joint Surg Am 2010;92:2300-4. [Crossref] [PubMed]
- Bhattoa HP, Nagy E, More C, et al. Prevalence and seasonal variation of hypovitaminosis D and its relationship to bone metabolism in healthy Hungarian men over 50 years of age: The HunMen Study. Osteoporos Int 2013;24:179-86. [Crossref] [PubMed]
- Jansen JA, Haddad FS. High prevalence of vitamin D deficiency in elderly patients with advanced osteoarthritis scheduled for total knee replacement associated with poorer preoperative functional state. Ann R Coll Surg Engl 2013;95:569-72. [Crossref] [PubMed]
- Lespasio MJ, Piuzzi NS, Husni ME, et al. Knee Osteoarthritis: A Primer. Perm J 2017.21. [PubMed]
- Lespasio MJ, Sultan AA, Piuzzi NS, et al. Hip Osteoarthritis: A Primer. Perm J 2018.22. [PubMed]
- Cleveland Clinic Orthopaedic Arthroplasty. The Association Between Readmission and Patient Experience in a Total Hip Arthroplasty Population. J Arthroplasty 2018;33:1668-74. [Crossref] [PubMed]
- Ng M, Song S, George J, et al. Associations between seasonal variation and post-operative complications after total hip arthroplasty. Ann Transl Med 2017;5:S33. [Crossref] [PubMed]
- Piuzzi NS, Muschler GF. CORR Insights®: Which Clinical and Patient Factors Influence the National Economic Burden of Hospital Readmissions After Total Joint Arthroplasty. Clin Orthop Relat Res 2017;475:2938-40. [Crossref] [PubMed]
- Sultan AA, Sodhi N, Khlopas A, et al. Preface: ATM special section: lower extremity arthroplasty. Ann Transl Med 2017;5:S23. [Crossref] [PubMed]
- Willhuber GC, Stagnaro J, Petracchi M, et al. Short-term complication rate following orthopedic surgery in a tertiary care center in Argentina. SICOT J 2018;4:26. [Crossref] [PubMed]
- Sahota O. Understanding vitamin D deficiency. Age Ageing 2014;43:589-91. [Crossref] [PubMed]
- Tran EY, Uhl RL, Rosenbaum AJ. Vitamin D in Orthopaedics. JBJS Rev 2017;5. [Crossref] [PubMed]