Diagnosis of neurodegenerative dementia: where do we stand, now?
Introduction
Dementia is an “umbrella term”, including disorders characterized by loss of cognitive functioning, such as thinking, remembering, and reasoning, and by impairment of behavioral abilities under particular conditions to such an extent that person’s daily life activities are compromised. Alzheimer’s disease (AD) is the first cause of dementia, followed by Lewy body and frontotemporal dementia. The prevalence of dementia is dramatically increasing in late life, and there are no effective interventions that can modify the disease course after clinical onset to date. In this context, early diagnosis, patient’s stratifications and identification of presymptomatic individuals at higher risk of developing a type of dementia, represent the main goals, also in order to “prevent the preventable”, intervening early on the known modifiable risk factors.
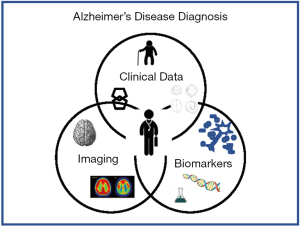
The modern concept for diagnosing dementia integrates clinical and neuropsychological examinations, together with evidences from genetics, biochemical and imaging tools, which can provide evidence indicative of the neuropathological process of the disease. Notwithstanding, both clinical and laboratory issues point out a few critical flaws about the integration and the use of cerebrospinal fluid (CSF) biomarkers, especially amongst those physicians that are skeptic on the value of biomarkers for investigating the neurodegenerative processes.
This review focuses on the evolution of the concept for diagnosing AD, and the advantage in integrating CSF biomarkers in clinical practice. Then, we will discuss the limitations and drawbacks of wide application of CSF biomarkers, and the role of the laboratory medicine to convey these biomarkers from “research” toward “clinical practice”.
The evolution of the diagnosis of Alzheimer’s dementia
AD is a complex multi-factorial disease and represents one of the greatest epidemic and health challenges among neurodegenerative disorders in the elderly. The most common cases are sporadic, characterized by late onset (LOAD) beyond the age of 65, while up to 5% are rare familiar cases (familial AD, FAD) with onset before 65 years.
For decades, AD was considered as a clinical and pathological entity (1). In 1984, the clinical criteria for the diagnosis of AD were centered around the observation of typical amnestic multidomain symptoms, which were assumed to be related to AD neuropathological changes at autopsy post-mortem, characterized by amyloid plaques and neurofibrillary tangles, the histological hallmarks of the disease. However, when symptoms were not manifest, preclinical neuropathological changes of AD could not be explorable. Following this paradigm, the clinical symptoms may define the presence of probable AD in patients who were alive, while the concept of clinical manifestation and disease were interrelated. These criteria do not include laboratory tests, except eventual instrumental examinations for the exclusion of secondary type of dementia (1).
The diagnostic approach was completely changed after discovering the radiotracer Pittsburgh compound-B (PiB), which can bind to aggregates of the Aβ peptide with high affinity in vitro. Thereafter a positron emission tomography (PET) method was developed for in vivo evaluation of Aβ plaque burden in vivo (2).
In 2006, the observation that plaque amyloid deposition in brain tissue in vivo results in low Aβ42 levels in CSF has revolutionized the idea of biomarkers for AD, thus providing the evidence of a fluid measurable marker of AD correlated with neuropathological process during the course of disease. Moreover, an unimaginable diagnostic opportunity emerged from the observations of amyloid plaque deposition detected by PET imaging associated with low CSF Aβ42 in apparently cognitive normal individuals, thus leading to the hypothesis of potential use of Aβ42 as biomarker of (preclinical) AD antecedent cognitive decline (3). Aside CSF low Aβ42, the high values of both t-tau and p-tau in CSF represent measurable markers of neurodegeneration and are pivotal for the in vivo diagnosis of AD (4).
In 2011, the recommendation for AD diagnosis have been revised by both the International Working Group (IWG) (4) and the US National Institute on Aging-Alzheimer’s Association (NIA-AA) (5-7). The new criteria abandon the old concept of AD dementia, based on the clinical assessment and autopsy confirmation, introducing a paradigm shift which points to early in vivo diagnosis of AD before development of dementia, thus representing a step forward from clinical-autoptic paradigm, registering the clinical consequences of completed pathological process to a clinical-biological paradigm, which emphasis on measurable in vivo evidences of developing AD pathology (8,9), which can be investigated by both CSF and topographical markers (assessed by PiB-PET and MRI).
The new recommendations created separate sets of diagnostic levels or “clinical” stages of AD, i.e., symptomatic AD, with mild cognitive impairment (MCI) or overt dementia (5,6), and non-symptomatic preclinical AD (7), identifying individuals not yet cognitively impaired but with abnormal AD biomarkers. The criteria for clinical symptomatic phases of AD were conceived to both aid the routine diagnostic procedures and providing a common lexicon to classify the clinical stages of Alzheimer’s pathology (2,3,5).
These last guidelines have been revised in 2018 by a NIA-AA leadership commissioned working group, with the aim to unify and update the 2011 recommendations (10). The absolute revolution of this so called “research framework” is that AD can be now defined in living persons as a biological construct, which can be identified by the assessment of changes of biomarkers that are indicative of disease’s neuropathology, independently by the manifestation of clinical symptoms. Biofluid and imaging biomarkers are grouped into the formula [AT (N)], which included Aβ deposition (A = low CSF Aβ or amyloid PET), pathologic tau (T = increased CSF p-tau and tau-PET) and neurodegeneration (N = increased CSF tau, FDG PET, MRI). Altered Aβ deposition with normal tau biomarkers define “Alzheimer’s pathologic change”, whereas evidence of both Aβ deposition and pathologic tau can identify “Alzheimer’s disease”, thus distinguishing earlier and later phases of the “Alzheimer’s continuum”. This research framework creates a novel algorithm for identifying and classifying pathological stages across disease’s entire spectrum, to facilitate standardized reporting of research findings across the field. However, it is not intended for general clinical practice, but it constitutes a research framework which have to be tested and modified (if needed) before being introduced into common clinical routine (10).
The CSF biomarker analysis has been currently accepted and adopted in general clinical practice, with some differences and limitations between countries. The Guidelines from the European Federation of Neurological Societies (EFNS) recommend the use of CSF biomarkers for the differential diagnosis in case of both typical and atypical AD (11,12). In Italy, the CSF biomarkers are included in the diagnostic criteria for AD in a limited number of centers, specialized for diagnosing dementia, located in about 65% of the Italian regions (13).
The use of CSF Biomarkers in clinical setting
The amyloid β1-42 (Aβ42) and its ratio with amyloid β 1-40 (Aβ42/Aβ40), together with biomarkers of neurodegeneration, total tau protein and phosphorylated tau181 (t-tau and p-tau), constitute the panel of CSF biomarkers for diagnosing AD (5,10,14). Changes in these core biomarkers allow to identify AD pathology also in the early, prodromal phase of disease (8,15-17). The same biomarkers are used also for the differential diagnosis with other forms of dementia, as exclusion criteria (9,18-21).
Decrease of Aβ42, together with increase of t-tau and p-tau, represent the “AD signature” detectable in the CSF, which is supposed to reflect the main neuropathological hallmarks of this condition, which encompass formation of amyloid plaques and neurofibrillary tangles. Therefore, Aβ is considered a marker of “amyloidosis”, although the concentration observed in the CSF mainly reflect a threshold value, which is indicative of either physiological or pathological status, but it is not associated with clinical phenotype, such as typical or atypical cognitive onset, severity, disease progression or response to treatment (22,23). Recently, the Aβ42/Aβ40 ratio has demonstrated to increase the diagnostic value of Aβ42 (18) by reducing the differences due to inter-individual variability, in particular to those individuals who are over or low producer of total Aβ (24). Moreover, Aβ42/Aβ 40 ratio is useful for reducing the bias attributable to preanalytical or analytical factors (25,26). An increased tau value in CSF is considered a marker of neuronal damage, which can be observed in AD as well as in different traumatic, infectious, prion or organic brain disorders. Oppositely, the tau hyperphosphorylation is a specific process characterizing AD pathogenesis, and its increase in CSF is hence pivotal for the diagnosis. Unlike Aβ, enhanced tau value may be related with the degree of cognitive decline and with diffuse neurodegeneration. Indeed, very high levels of both t-tau and p-tau may be associated with a rapid and severe progression (27,28), or to malignant forms of AD with higher risk of mortality (29). Interestingly, tau CSF increase is sometimes not associated to low Aβ42 levels, and this finding may represent a specific biochemical pattern of “suspected non-amyloid patient or non-Alzheimer’s disease pathophysiology” (SNAP), which represent a novel concept of distinct Tau pathology separated from AD (30). This is an interesting issue for both clinical classification and patient stratification.
Changes in the concentrations of these biomarkers may be observed in CSF decades before the onset of cognitive symptoms, thus representing useful predictive tools, with decrease of Aβ eventually occurring even twenty years before clinical manifestation, in healthy stages, while tau change later on (6).
The sensitivity reported in different studies is variable, ranging from 76% to 96% for Aβ42 (31), and combined with 65–80% specificity and 40–86% sensitivity for tau (9,32). Thus, combinations of fluid and imaging biomarkers may help improving the diagnostic accuracy and have a better predictive value also for disease severity (33). Different ratios have been proposed, with several and novel candidate markers to increase the diagnostic performance and to follow the variation of each of them throughout the disease course (34). In this view, the collection of data emerged from different omics technologies have changed the approach in our knowledge of AD at multiple levels, thus integrating data from genomic, transcriptomic, epigenomic, proteomic and metabolomic. Then, the Omics era has opened new frontiers toward the development of personalized diagnostic and therapeutic tools (35). Several major genetics or proteomics research programs are nowadays ongoing, then there is a great hope for novel discoveries over the coming years.
Evidences suggest that different genetic factors may play a crucial role in the onset of sporadic cases of AD. The apolipoprotein E (ApoE) gene codes for an apolipoprotein and a transporter of cholesterol that is found in the brain, and represent the main known genetic risk factor for AD. Three different allelic variants, epsilon 2 (ε2), 3 (ε3) and 4 (ε4), have different frequency in the general populations and in AD patients, in particular, carriers of ApoE ε4 are 3 to 4 folds more likely to develop AD respect to non ε4 carriers (36). Actually, several genome wide association studies (GWAS) have identified novel promising risk genes for AD, but they have not yet been included in diagnostic or screening procedures.
The laboratory in the validation of CSF Biomarkers
Integrated clinic-biological diagnosis for AD includes the measurement of the neurodegenerative biomarkers in the CSF (37-40) (Figure 1). Nevertheless, the interpretation of test results needs expertise and caution. Clinical discrepancies of results and analytical issues lowered the accuracy of CSF markers. For example, variability due to the operator or methodological platforms, pre and post analytical procedures, represent the major criticisms for the diffusion of CSF biomarkers as diagnostic tool.
The role of laboratory is crucial for the standardization and harmonization of analytical procedures and criteria for interpretation and use of test results, thus also including cut-off values and decision limits (41).
CSF biomarkers can be measured by using different single or multi analyte test (e.g., enzyme-linked immunosorbent assays (ELISAs) or xMAP technology). Recently, fully automated chemiluminescent methods have been developed, that are expected to reduce the variability compared to manual measurement, and could further facilitate the accreditation of these measurements according to quality regulations (42,43). Several national and international initiative are ongoing, with the common aim to standardize the use and interpretation of AD CSF biomarkers. Since 2009, the Alzheimer’s Association Quality Control (AA QC) program, aim at monitoring analytical variability for CSF biomarkers between laboratories worldwide (44). Moreover, the BIOMARKAPD (biomarkers for AD and Parkinson’s disease) project, that is supported by the European Joint Program Neurodegenerative Disease Research (JPND) consortium, focuses on the definition of certified reference materials for harmonizing assays (45). However, the great effort of all these initiatives is to reach the reproducibility and consistency of measurements, the worldwide comparison of the results, a consensus on the use of CSF biomarkers and finally to reduce debate in clinical value and interpretation for diagnosing AD (46).
Concluding remarks
Early and timely diagnosis of AD is a big challenge. The analysis of biochemical and molecular biomarkers gives a unique opportunity to investigate the underlying pathophysiological mechanisms of neurodegeneration, thus providing an added value in terms of diagnosis, prognostication and therapeutic strategy. Advanced analytical techniques and several international quality control programs may help harmonizing assays procedures and reducing assays variability across centers in a limited timeframe, thus encouraging routine uses of CSF biomarkers for characterizing the biological signature of neurodegenerative disorders in clinical setting.
Acknowledgements
Dedicated to the memory of Prof. Mario Lo Bello, a year since he passed.
Funding: The study has been supported in part by the Italian Ministry of Healthy (GR-2011-02349822).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- McKhann G, Drachman D, Folstein M, et al. Clinical diagnosis of Alzheimer's disease: report of the NINCDS-ADRDA Work Group under the auspices of Department of Health and Human Services Task Force on Alzheimer's Disease. Neurology 1984;34:939-44. [Crossref] [PubMed]
- Ikonomovic MD, Klunk WE, Abrahamson EE, et al. Post-mortem correlates of in vivo PiB-PET amyloid imaging in a typical case of Alzheimer's disease. Brain 2008;131:1630-45. [Crossref] [PubMed]
- Fagan AM, Mintun MA, Mach RH, et al. Inverse relation between in vivo amyloid imaging load and cerebrospinal fluid Abeta42 in humans. Ann Neurol 2006;59:512-9. [Crossref] [PubMed]
- Dubois B, Feldman HH, Jacova C, et al. Revising the definition of Alzheimer's disease: a new lexicon. Lancet Neurol 2010;9:1118-27. [Crossref] [PubMed]
- McKhann GM, Knopman DS, Chertkow H, et al. The diagnosis of dementia due to Alzheimer's disease: recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer's disease. Alzheimers Dement 2011;7:263-9. [Crossref] [PubMed]
- Albert MS, DeKosky ST, Dickson D, et al. The diagnosis of mild cognitive impairment due to Alzheimer's disease: recommendations from the National Institute on Aging-Alzheimer's Association workgroups on diagnostic guidelines for Alzheimer's disease. Alzheimers Dement 2011;7:270-9. [Crossref] [PubMed]
- Sperling RA, Aisen PS, Beckett LA, et al. Toward defining the preclinical stages of Alzheimer's disease: recommendations from the National Institute on Aging-Alzheimer's Association workgroups on diagnostic guidelines for Alzheimer's disease. Alzheimers Dement 2011;7:280-92. [Crossref] [PubMed]
- Le Bastard N, Martin JJ, Vanmechelen E, et al. Added diagnostic value of CSF biomarkers in differential dementia diagnosis. Neurobiol Aging 2010;31:1867-76. [Crossref] [PubMed]
- Sancesario GM, Bernardini S. How many biomarkers to discriminate neurodegenerative dementia? Crit Rev Clin Lab Sci 2015;52:314-26. [Crossref] [PubMed]
- Jack CR Jr, Bennett DA, Blennow K, et al. NIA-AA Research Framework: Toward a biological definition of Alzheimer's disease. Alzheimers Dement 2018;14:535-62. [Crossref] [PubMed]
- Hort J, O'Brien JT, Gainotti G, et al. EFNS guidelines for the diagnosis and management of Alzheimer's disease. Eur J Neurol 2010;17:1236-48. [Crossref] [PubMed]
- Sorbi S, Hort J, Erkinjuntti T, et al. EFNS-ENS Guidelines on the diagnosis and management of disorders associated with dementia. Eur J Neurol 2012;19:1159-79. [Crossref] [PubMed]
- Sancesario GM, Toniolo S, Chiasserini D, et al. The Clinical Use of Cerebrospinal Fluid Biomarkers for Alzheimer's Disease Diagnosis: The Italian Selfie. J Alzheimers Dis 2017;55:1659-66. [Crossref] [PubMed]
- Dubois B, Feldman HH, Jacova C, et al. Advancing research diagnostic criteria for Alzheimer's disease: the IWG-2 criteria. Lancet Neurol 2014;13:614-29. [Crossref] [PubMed]
- Hansson O, Zetterberg H, Buchhave P, et al. Association between CSF biomarkers and incipient Alzheimer's disease in patients with mild cognitive impairment: a follow-up study. Lancet Neurol 2006;5:228-34. [Crossref] [PubMed]
- Schoonenboom NS, Reesink FE, Verwey NA, et al. Cerebrospinal fluid markers for differential dementia diagnosis in a large memory clinic cohort. Neurology 2012;78:47-54. [Crossref] [PubMed]
- Engelborghs S, De Vreese K, Van de Casteele T, et al. Diagnostic performance of a CSF-biomarker panel in autopsy-confirmed dementia. Neurobiol Aging 2008;29:1143-59. [Crossref] [PubMed]
- Janelidze S, Zetterberg H, Mattsson N, et al. CSF Abeta42/Abeta40 and Abeta42/Abeta38 ratios: better diagnostic markers of Alzheimer disease. Ann Clin Transl Neurol 2016;3:154-65. [Crossref] [PubMed]
- Schirinzi T, Sancesario GM, Di Lazzaro G, et al. Clinical value of CSF amyloid-beta-42 and tau proteins in Progressive Supranuclear Palsy. J Neural Transm (Vienna) 2018. [Epub ahead of print]. [Crossref] [PubMed]
- Schirinzi T, Sancesario GM, Di Lazzaro G, et al. Cerebrospinal fluid biomarkers profile of idiopathic normal pressure hydrocephalus. J Neural Transm (Vienna) 2018;125:673-9. [Crossref] [PubMed]
- Schirinzi T, Sancesario GM, Ialongo C, et al. A clinical and biochemical analysis in the differential diagnosis of idiopathic normal pressure hydrocephalus. Front Neurol 2015;6:86. [Crossref] [PubMed]
- Schirinzi T, Di Lazzaro G, Sancesario GM, et al. Levels of amyloid-beta-42 and CSF pressure are directly related in patients with Alzheimer's disease. J Neural Transm (Vienna) 2017;124:1621-5. [Crossref] [PubMed]
- Schirinzi T, Di Lorenzo F, Sancesario GM, et al. Amyloid-Mediated Cholinergic Dysfunction in Motor Impairment Related to Alzheimer's Disease. J Alzheimers Dis 2018;64:525-32. [Crossref] [PubMed]
- Wiltfang J, Esselmann H, Bibl M, et al. Amyloid beta peptide ratio 42/40 but not A beta 42 correlates with phospho-Tau in patients with low- and high-CSF A beta 40 load. J Neurochem 2007;101:1053-9. [Crossref] [PubMed]
- Nutu M, Zetterberg H, Londos E, et al. Evaluation of the cerebrospinal fluid amyloid-beta1-42/amyloid-beta1-40 ratio measured by alpha-LISA to distinguish Alzheimer's disease from other dementia disorders. Dement Geriatr Cogn Disord 2013;36:99-110. [Crossref] [PubMed]
- Sauvee M. Additional use of Abeta(4)(2)/Abeta(4)(0) ratio with cerebrospinal fluid biomarkers P-tau and Abeta(4)(2) increases the level of evidence of Alzheimer's disease pathophysiological process in routine practice. J Alzheimers Dis 2014;41:377-86. [Crossref] [PubMed]
- Kester MI, van der Vlies AE, Blankenstein MA, et al. CSF biomarkers predict rate of cognitive decline in Alzheimer disease. Neurology 2009;73:1353-8. [Crossref] [PubMed]
- Koch G, Belli L, Giudice TL, et al. Frailty among Alzheimer's disease patients. CNS Neurol Disord Drug Targets 2013;12:507-11. [Crossref] [PubMed]
- Wallin AK, Blennow K, Zetterberg H, et al. CSF biomarkers predict a more malignant outcome in Alzheimer disease. Neurology 2010;74:1531-7. [Crossref] [PubMed]
- Dani M, Brooks DJ, Edison P. Suspected non-Alzheimer's pathology - Is it non-Alzheimer's or non-amyloid? Ageing Res Rev 2017;36:20-31. [Crossref] [PubMed]
- Blennow K, Zetterberg H. Cerebrospinal fluid biomarkers for Alzheimer's disease. J Alzheimers Dis 2009;18:413-7. [Crossref] [PubMed]
- Blennow K, Zetterberg H, Minthon L, et al. Longitudinal stability of CSF biomarkers in Alzheimer's disease. Neurosci Lett 2007;419:18-22. [Crossref] [PubMed]
- Liguori C, Chiaravalloti A, Sancesario G, et al. Cerebrospinal fluid lactate levels and brain [18F]FDG PET hypometabolism within the default mode network in Alzheimer's disease. Eur J Nucl Med Mol Imaging 2016;43:2040-9. [Crossref] [PubMed]
- Liguori C, Stefani A, Sancesario G, et al. CSF lactate levels, tau proteins, cognitive decline: a dynamic relationship in Alzheimer's disease. J Neurol Neurosurg Psychiatry 2015;86:655-9. [Crossref] [PubMed]
- Sancesario GM, Bernardini S. Alzheimer's disease in the omics era. Clin Biochem 2018;59:9-16. [Crossref] [PubMed]
- Bu G. Apolipoprotein E and its receptors in Alzheimer's disease: pathways, pathogenesis and therapy. Nat Rev Neurosci 2009;10:333-44. [Crossref] [PubMed]
- Martorana A. Alzheimer's Disease and the Routine Clinical Use of CSF Biomarkers. CNS Neurol Disord Drug Targets 2017;16:407-13. [Crossref] [PubMed]
- Molinuevo JL, Blennow K, Dubois B, et al. The clinical use of cerebrospinal fluid biomarker testing for Alzheimer's disease diagnosis: a consensus paper from the Alzheimer's Biomarkers Standardization Initiative. Alzheimers Dement 2014;10:808-17. [Crossref] [PubMed]
- Blennow K, Dubois B, Fagan AM, et al. Clinical utility of cerebrospinal fluid biomarkers in the diagnosis of early Alzheimer's disease. Alzheimers Dement 2015;11:58-69. [Crossref] [PubMed]
- Mouton-Liger F, Wallon D, Troussiere AC, et al. Impact of cerebro-spinal fluid biomarkers of Alzheimer's disease in clinical practice: a multicentric study. J Neurol 2014;261:144-51. [Crossref] [PubMed]
- Plebani M. Harmonization in laboratory medicine: the complete picture. Clin Chem Lab Med 2013;51:741-51. [Crossref] [PubMed]
- Le Bastard N, Coart E, Vanderstichele H, et al. Comparison of two analytical platforms for the clinical qualification of Alzheimer's disease biomarkers in pathologically-confirmed dementia. J Alzheimers Dis 2013;33:117-31. [Crossref] [PubMed]
- Bjerke M, Portelius E, Minthon L, et al. Confounding factors influencing amyloid Beta concentration in cerebrospinal fluid. Int J Alzheimers Dis 2010;2010.
- Mattsson N, Andreasson U, Persson S, et al. CSF biomarker variability in the Alzheimer's Association quality control program. Alzheimers Dement 2013;9:251-61. [Crossref] [PubMed]
- Bjerke M, Andreasson U, Kuhlmann J, et al. Assessing the commutability of reference material formats for the harmonization of amyloid-beta measurements. Clin Chem Lab Med 2016;54:1177-91. [Crossref] [PubMed]
- Niemantsverdriet E, Valckx S, Bjerke M, et al. Alzheimer's disease CSF biomarkers: clinical indications and rational use. Acta Neurol Belg 2017;117:591-602. [Crossref] [PubMed]


