Patient satisfaction and outcomes of static progressive stretch bracing: a 10-year prospective analysis
Introduction
Many non-surgical and surgical treatment modalities have been developed for patients suffering from shoulder, elbow, forearm, wrist, knee and ankle pathologies. Often surgical treatment plans are reserved for patients suffering from chronic stiffness that has not been relieved with other non-surgical treatment modalities. To help avoid potential joint stiffness, the pathological joint should be identified within 6 months or less after the initial trauma and treated with non-surgical treatment modalities, including turnbuckle, static progressive stretch (SPS), and/or dynamic braces (1,2). Although each type of brace seeks to achieve a similar ultimate goal, each bracing modality involves a different mechanism of action. Turnbuckle braces function by applying a low intensity, static force on the joint in order to aid in the release of a contracture, and are manually adjusted to generate the necessary tension level (3). SPS braces provide a low intensity, manually adjustable force that is incrementally increased as joint tissues relax in response to stress loads applied (4). SPS braces commonly work bi-directionally, allowing flexion and extension therapy with one device. Dynamic braces provide a constant level of low intensity force to the joint over a prolonged treatment time, commonly known as “creep” (5). Dynamic braces commonly work in one direction only, requiring one device to provide flexion and a second to provide extension stretch.
The ultimate goal of each of the above bracing modalities is to help patients regain a functional range of motion (ROM) to carry out activities of daily living (ADLs). For the elbow, normal ROM to successfully complete ADLs has been suggested to be 100 degrees of flexion (range, 30 to 130 degrees) along with 100 degrees of forearm rotation (50 degrees pronation and supination) (6). The mean shoulder ROM for ADLs has been described to be 121 degrees flexion, 46 degrees extension, 128 degrees of shoulder abduction, 116 degrees of shoulder cross-body abduction, 90 degrees of external rotation with abduction of 59 degrees, and 102 degrees of internal rotation with 0 degrees of abduction (7). Functional ROM for the wrist has been shown to be 38 degrees of wrist flexion, 40 degrees of wrist extension, 38 degrees of ulnar deviation, and 28 degrees of radial deviation (8). For the knee, it has been reported that less than 90 degrees of knee flexion is required for gait, 90 to 120 degrees is required for stairs and chairs, and that 110 degrees of flexion is an appropriate goal for patient to achieve in order to carry out ADLs (9). The mean maximum ankle ROM to carry out ADLs has been suggested to be 28 degrees of dorsiflexion and 37 degrees of plantar flexion (10).
Recent studies have reported on the advantages of these braces for patient care (11,12). Using these studies in practice is critical, as current changes to the healthcare system are pushing for more evidence-based treatment plans in order to provide the most effective care for patients. An important part of this push for better patient treatment is based on patient reported outcomes. Although, in general, these above three brace types have been shown to have successful outcomes, there are a number of different manufacturers, and company specific designs might affect outcomes. Therefore, the purpose of this study was to analyze 10 years of prospectively collected patient satisfaction and outcomes data from a single brace company. Specifically, we evaluated: (I) mobility, (II) pain, (III) stiffness, (IV) swelling, and (V) any adverse events of patients treated with an SPS brace.
Methods
Patient selection
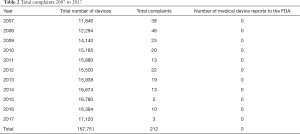
From 2007 to 2017, data from patients treated with a Static Progressive Stretch Brace (Joint Active Systems Inc., Effingham, IL, USA) were prospectively collected. The data was organized on a quarterly system, from which overall value means were calculated. A total of 167,751 patients were treated from January 1st, 2007 to December 31st, 2017, with the yearly breakdown of 11,846 patients in 2007, 12,294 patients in 2008, 14,140 patients in 2009, 15,185 patients in 2010, 15,880 patients in 2011, 15,500 patients in 2012, 15,938 patients in 2013, 16,674 patients in 2014, 16,780 patients in 2015, 16,394 patients in 2016, and 17,120 patients in 2017. Patient demographics of those who were treated were 41% male and 49% female; for 10% gender was not identified. The mean age was 48 years. The primary diagnosis or reason for treatment with each brace can be noted in Table 1. From all patients treated, 50 per month (600 per year) were randomly and prospectively selected to complete the survey.

Full table
Patient survey
Patients were given a cross-sectional survey addressing various outcomes such as pain, stiffness, swelling, and mobility. More specifically, each of those outcomes were assessed by asking “Are you having pain?”, “Do you have any stiffness?”, “Do you have any swelling?”, and “Do you feel your mobility has improved?” For questions concerning pain, stiffness, and swelling, patients who responded to the survey question answered either “yes” or “no”. Responses from 2007 to 2017 were collected and analyzed for pain, stiffness, and swelling. For mobility, patients answered either “yes”, “no”, or “undecided”. Any patient complaints, as well as device related serious injuries, were also tabulated.
Data analysis
All patient data was initially collected from the patient’s medical records. All corresponding demographic data was also collected based on the patient’s medical record. All personal patient information was de-identified and all pertinent information concerning pain, stiffness, swelling, mobility, and complaints were transferred to an Excel sheet for analysis. Patient responses were analyzed by taking the mean percentage of the quarterly responses to obtain a yearly mean percentage for each respective outcome. A yearly trend analysis was also performed.
Results
Mobility
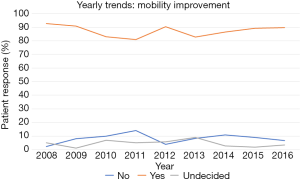
From 2008 to 2016, the percentage of patients who reported improved mobility after brace use remained fairly constant, with an overall mean of roughly 90%. On average, from 2008 to 2016, less than 10% of patients reported no improvement in mobility. The exact yearly trends for improvements in mobility can be seen in Figure 1.
Pain
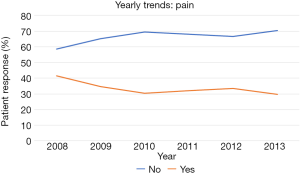
The yearly trends in pain revealed an increase in the percent of patients reporting no pain after brace use from 2008 to 2013. Specifically, in 2013, 70% of patients reported no pain after using their brace, while in 2008, 59% of patients reported no pain after using their brace. The exact yearly trends for pain can be seen in Figure 2.
Stiffness
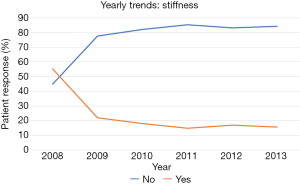
The yearly trends in stiffness indicate a decrease in stiffness after brace use from 2008 to 2013. Specifically, in 2013, 84% of patients reported no stiffness after using their brace, while in 2008, 45% of patients reported no stiffness after using their brace. The exact yearly trends for stiffness can be seen in Figure 3.
Swelling
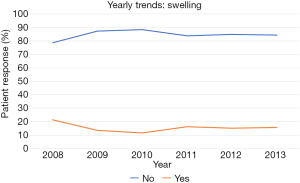
Similarly, the yearly trends in patients reporting no joint swelling after brace use increased from 2008 to 2013. Specifically, in 2013, 84% of patients reported no swelling after using their brace, while in 2008, 79% of patients reported no swelling after using their brace. The exact yearly trends for swelling can be seen in Figure 4.
Total complaints
Overall, the total number of complaints during the 10-year period were trended downwards from 2007 (n=38) to 2017 (n=3) (Table 2). In 2008 a peak of 46 complaints were made, while 2017 had the fewest complaints. From 2007 to 2017, no patients experienced any device related serious injuries. Majority of complaints were non-severe, such as slight discomfort due to device size. The number of complaints for each year can be seen in Table 2.
Full table
Discussion
Patients suffering from upper and/or lower extremity joint stiffness due to atraumatic or traumatic injury have multiple non-surgical to surgical treatment modalities to choose from. However, physicians and patients alike tend to prefer non-surgical treatment options. This preference has led to a number of different bracing modalities such as SPS, turnbuckle, and dynamic braces. SPS braces in particular have shown to provide better patient outcomes when compared to turnbuckle and dynamic braces (13). This study found that the yearly mean percentage for pain, stiffness, and swelling has steadily decreased in patients treated with an SPS brace. In 2008, 59% of patient reported no pain after treatment, while in 2013, that number increased to 70% of patients who reported no pain. Similar trends were seen in stiffness and swelling; in 2008, 45% of patients reported no stiffness and 79% of patients reported no swelling compared to 84% of patients who reported no stiffness and 84% of patients reported no swelling in 2013. Patients also consistently reported improvements in mobility. Based on these patient-reported clinical and satisfaction data, the braces analyzed in this study are highly effective and patient friendly, and should therefore be recommended to patients suffering from elbow, shoulder, or knee pathology.
In addition to the articulating joints covered in this analysis, several studies have also reported braces to be an effective non-surgical treatment modality for wrist, forearm, and ankle pathologies (4,14,15).
There are some limitations to this study. The patient data collected for this study was based on patients specifically treated with brace modalities from a single company. For this reason, the data could not be compared to other bracing companies. Additionally, this study analyzed patient reported satisfaction and outcomes data collected from surveys. However, as is part of any long-term study, some patients were lost to follow-up or simply did not complete the survey. However, given the large patient population and longevity of the patient responses over the years, this study still provides a comprehensive evaluation.
Conclusions
Overall, this study found that patients managed with an SPS brace over the past 10 years have experienced decreased pain, stiffness, and swelling after orthosis treatment. Furthermore, these patients have also experienced a steady increase in mobility over the 10 years with this orthosis treatment. Additionally, over the past 10 years, there have been no reports of serious injury, and a trend towards a reduced number of complaints can also be noted. These results are of particular importance, since no other study reports prospective data on thousands of patients showing that a bracing system substantially reduces pain and stiffness These data indicate that not only are these braces effective in improving functional ROM with high rate of success and no significant complications, but this bracing system has a significant effect on improving pain and stiffness. Therefore, based on the results from this prospective study of nearly 170,000 patients, patients suffering from upper or lower extremity joint pathology can expect excellent clinical outcomes using any of the analyzed ROM therapy braces.
Acknowledgements
None.
Footnote
Conflicts of Interest: MA Mont—AAOS, Cymedica, DJ Orthopaedics, Johnson & Johnson, Journal of Arthroplasty, Journal of Knee Surgery, Microport, National Institutes of Health (NIAMS & NICHD), Ongoing Care Solutions, Orthopedics, Orthosensor, Pacira, Peerwell, Performance Dynamics Inc., Sage, Stryker—IP royalties, Surgical Technologies International, Kolon TissueGene. The other authors have no conflicts of interest to declare.
Ethical Statement: Study approval and patient consent was obtained.
References
- Nandi S, Maschke S, Evans PJ, et al. The stiff elbow. Hand (N Y) 2009;4:368-79. [Crossref] [PubMed]
- Doornberg JN, Ring D, Jupiter JB. Static progressive splinting for posttraumatic elbow stiffness. J Orthop Trauma 2006;20:400-4. [Crossref] [PubMed]
- Gelinas JJ, Faber KJ, Patterson SD, et al. The effectiveness of turnbuckle splinting for elbow contractures. J Bone Joint Surg Br 2000;82:74-8. [Crossref] [PubMed]
- Costa CR, McElroy MJ, Johnson AJ, et al. Use of a static progressive stretch orthosis to treat post-traumatic ankle stiffness. BMC Res Notes 2012;5:348. [Crossref] [PubMed]
- Pierce TP, Cherian JJ, Mont MA. Static and Dynamic Bracing for Loss of Motion Following Total Knee Arthroplasty. J Long Term Eff Med Implants 2015;25:337-43. [Crossref] [PubMed]
- Morrey BF, Askew LJ, Chao EY. A biomechanical study of normal functional elbow motion. J Bone Joint Surg Am 1981;63:872-7. [Crossref] [PubMed]
- Namdari S, Yagnik G, Ebaugh DD, et al. Defining functional shoulder range of motion for activities of daily living. J Shoulder Elbow Surg 2012;21:1177-83. [Crossref] [PubMed]
- Gates DH, Walters LS, Cowley J, et al. Range of Motion Requirements for Upper-Limb Activities of Daily Living. Am J Occup Ther 2016;70:7001350010p1-7001350010p10.
- Rowe PJ, Myles CM, Walker C, et al. Knee joint kinematics in gait and other functional activities measured using flexible electrogoniometry: how much knee motion is sufficient for normal daily life? Gait Posture 2000;12:143-55. [Crossref] [PubMed]
- Hyodo K, Masuda T, Aizawa J, et al. Hip, knee, and ankle kinematics during activities of daily living: a cross-sectional study. Braz J Phys Ther 2017;21:159-66. [Crossref] [PubMed]
- Sodhi N, Khlopas A, Vaughn MD, et al. Manufactured Brace Modalities for Elbow Stiffness. Orthopedics 2018;41:e127-35. [Crossref] [PubMed]
- Veltman ES, Doornberg JN, Eygendaal D, et al. Static progressive versus dynamic splinting for posttraumatic elbow stiffness: a systematic review of 232 patients. Arch Orthop Trauma Surg 2015;135:613-7. [Crossref] [PubMed]
- Sodhi N, Yao B, Khlopas A, et al. A Case for the Brace: A Critical, Comprehensive, and Up-To-Date Review of Static Progressive Stretch, Dynamic, and Turnbuckle Braces for the Management of Elbow, Knee, and Shoulder Pathology. Surg Technol Int 2017;31:303-18. [PubMed]
- Lucado AM, Li Z. Static progressive splinting to improve wrist stiffness after distal radius fracture: a prospective, case series study. Physiother Theory Pract 2009;25:297-309. [Crossref] [PubMed]
- McGrath MS, Ulrich SD, Bonutti PM, et al. Static progressive splinting for restoration of rotational motion of the forearm. J Hand Ther 2009;22:3-8. [Crossref] [PubMed]