Laparoscopic spleen retains the body and tail of the pancreas resection
Introduction
Pancreatic cystic neoplasms are estimated to be present in 2 to 45 percent of the general population, accounting for 1 to 2 percent of all pancreatic tumors (1). The histopathological features of these tumors are often divided into the mucinous cystic neoplasm (MCN) and serous cystic neoplasm (SCN) categories (2). Due to the low risk of malignant transformation of SCNs, estimated to be 0 to 1.2 percent (3), surgical resection should only be considered when the cysts are causing serious symptoms, or when it is not possible to differentiate from a MCN with concerning features.
Case report
A 46-year-old female presents for a follow-up after a physical examination found a tumor mass in the body and the tail of the pancreas two years ago. At the time, the tumor size was measured at 15 mm, and subsequently, pancreatic ultrasounds were performed intermittently to monitor growth. On this occasion, the patient reports a recent onset of left upper abdominal distension pain, and early satiety after a meal. There was no associated lower back pain, unaccompanied nausea, vomiting, dizziness, palpitation, clammy skin or other symptoms of low blood sugar. She has had a three-year history of hypertension, with irregular use of amlodipine that maintained systolic pressures between 140–170 mmHg.
Clinical examination was largely unremarkable and nonspecific, with normal hemodynamic parameters, and no jaundice or sclera icterus. There was non-specific tenderness over the whole abdomen, with no obvious foci nor distension. The rest of the examination was essentially normal.
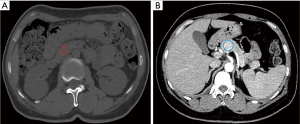
The routine investigations were within a normal range, except for slightly increased CA125 47.9 U/mL (normal 0–35.0 U/mL). All blood serology reports were negative. Upper abdomen computed tomography (CT) demonstrated a solid mass at the neck of the pancreas (Figure 1A), with features suggestive of a pancreatic neck partial leaf cystic mass. There was no abdominal lymph node enlargement, nor vascular invasion (Figure 1B). According to the above CT findings, and CA125 results, the diagnosis of pancreatic serous adenoma was deemed likely.
While the small sized benign pancreatic tumors usually require only routine follow-ups, the patient’s symptomatic presentation with distending pain, and left upper quadrant tenderness warranted surgical treatment, as European evidence-based guide of cystic neoplasms of the pancreas suggest surgical management for symptom control. In light of the patient’s age, and the non-malignancy of the tumor, pancreatectomy with spleen-preservation under a laparoscopy approach was elected, following discussion with the patient and her family. Informed consent, with risk, benefit and alternatives detailed, was provided.
Operative technique
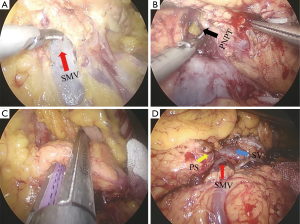
The patient was anesthetized with general anesthesia, and a sterile field established. Umbilicus puncture was used to establish a carbon dioxide pneumoperitoneum at 15 mmHg. A partial arc of five trocars were inserted in the abdominal wall surrounding the tumor. After routine exploration of the abdominal cavity failed to find any ascites or intraperitoneal tumor metastases, an ultrasound knife was used to open the gastric and colonic ligaments. Upon exploration of the pancreas, a 3 cm × 2 cm mass was identified in the neck of the pancreas. The upper and lower edges of the pancreas were carefully dissected, exposing the superior mesenteric vein (Figure 2A), and opened a tunnel behind the neck of the pancreas (Figure 2B), the neck of the pancreas is divided, usually with an ENDO-GIA (Figure 2C). Along the splenic artery and vein, a free body, and tail of the pancreas, there was a complete removal of the body tail of the pancreas (Figure 2D). A complete hemostasis of the wound, saline irrigation and a cleaning abdominal cavity was performed. Examination was done, to determine no pancreatic leakage and inactive bleeding, as well as determining abdominal drainage in the tube of the pancreas bed. The estimated amount of blood loss was 300 mL. The resected specimen was sent to the pathological laboratory (Figure 3).

Clinical outcome
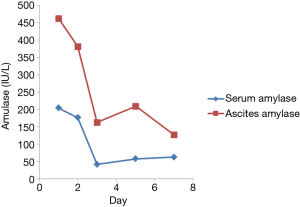
The patient recovered uneventfully, with no postoperative bleeding, pancreatic leakage (Figure 4), intra-abdominal infection, gastric emptying disorders, intestinal root obstruction or any other complications. The gastrointestinal decompression tube, indwelling catheter, and abdominal drainage tube was removed on postoperative day 2, day 7, and day 9, respectively. Pathologically, the tumor was confirmed to be a serous cystic neoplasm.
Discussion
Pancreatic serous cystic neoplasm is a benign tumor of the pancreas, with 44% of the lesions located in the neck, head, or uncinate process of the pancreas, while the remaining are in the body or tail region (5). The typical endosonographic features of SCN include aggregates of several small (3 to 5 mm each) cysts separated by thin septa, creating a honeycombing appearance. The aggregation of very small cystic lesions might be mistaken for a solid mass on CT scan. In this patient, the CT plain scan was also identified as a solid lesion, but in view of the patient's long-term follow-up history, a benign tumor was considered more likely, and the later an enhanced CT showed a characteristic SCN features.
Excision of the benign tumor of the pancreas was done as far as possible to reduce the organ damage to the tissue and adjacent organs. Surgery is still the goal, but over the years, because the tail of the pancreas and the spleen have blood vessel anatomies that are closely related to the pancreatic body and tail of a large tumor. Therefore, splenectomy may be performed though the tumors on the tail of the pancreas are benign. In recent years new developments have given the medical community a better understanding of the physiological function of the spleen. Experts have proposed preserving the non-malignant pancreatic tail tumors so as to preserve the spleen. In 1996, Kimura et al. (6) first reported a spleen-preserving distal pancreatectomy. At the present, the evidence shows that splenic-preserving distal pancreatectomy has been demonstrated to be safe and effective. Combined with the rapid development of laparoscopy techniques and popularization, spleen preserving laparoscopy with distal pancreatectomy is considered a first choice operation for symptomatic benign, or small malignant lesions located at the body or tail of the pancreas (7).
In the case, it was more beneficial for the patient to receive a minimal, non-invasive spleen-preserving operation so as to avoid a lifetime of immune system deficiency and thrombocytosis. The potential advantages are obvious, and include decreased risk of infection or sepsis, while the necessity for long-term anticoagulant treatment, (antiplatelet drugs) and chemoprophylaxis is minimized. The advantages of spleen-preservation laparoscopy, and distal pancreas resection include shorter hospitalization, and recovery time, reduced postoperative pain, reduced adhesions, and better cosmesis.
In conclusion, it is safe and feasible to perform laparoscopic spleen operation that retains the body and tail of the pancreas resection, and it is worth considering for patients with benign, or low-malignancy tumors of the tail of the pancreas.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- European Study Group on Cystic Tumors of the Pancreas. European evidence-based guidelines on pancreatic cystic neoplasms. Gut 2018;67:789-804. [Crossref] [PubMed]
- Nuzhat Z, Palma C, Rice GE, et al. Exosomes in pancreatic juice as valuable source of biomarkers for early diagnosis of pancreatic cancer. Transl Cancer Res 2017;6:S1339-51. [Crossref]
- Lennon AM. Cystic Neoplasms of the Pancreas. J Gastrointest Surg 2013;17:645-53. [Crossref] [PubMed]
- Zheng Z, Shi Y, Wen T, et al. Laparoscopic spleen retains the body and tail of the pancreas resection. Asvide 2018;5:762. Available online: http://www.asvide.com/article/view/27370
- Mohamadnejad M, Eloubeidi MA. Cystsic lesions of the pancreas. Arch Iran Med 2013;16:233-9. [PubMed]
- Kimura W, Inoue T, Futakawa N, et al. Spleen-preserving distal pancreatectomy with conservation of the splenic artery and vein. Surgery 1996;120:885-90. [Crossref] [PubMed]
- de Rooij T, Klompmaker S, Hilal MA, et al. Laparoscopic pancreatic surgery for benign and malignant disease. Nat Rev Gastroenterol Hepatol 2016;13:227-38. [Crossref] [PubMed]
(English Language Editor: Jeremy Dean Chapnick, AME Publishing Company)