
Use of an offset head center acetabular shell in difficult primary total hip arthroplasties
Introduction
A large number of young patients who develop hip arthritis possess a severe biomechanical abnormality of the joint. This can be the sequela of developmental dysplasia of the hip, osteonecrosis, or septic arthritis, among others (1,2). These etiologies may result in antero-lateral and/or superior bone deficiency which may compromise acetabular component stability and impair reliable fixation. In addition to the immediate fixation and stability of the implant, the mid- and long-term stability may be compromised. Several methods of improving acetabular component stability and coverage have been utilized including autograft bone and metal adjuncts, oval shaped shells, reinforcement with acetabular augments, and larger acetabular cups placed superiorly (jumbo cup) (3-6). However, the use of these treatment methods may require special instrumentation, different surgical techniques, and may increase operative times. Many studies have evaluated the use of jumbo cups in antero-lateral bone deficiency and demonstrated good survivorship of the cup (7-11). However, these implants are associated with elevated center of rotation (COR) of the hip which may lead to altered hip biomechanics (7-13), leg length discrepancies, and poor clinical outcomes (14-16).
Recently, a new acetabular shell has been developed with the goal of bringing down the hip center of rotation while achieving adequate fixation. This shell is hemispherical, possesses offset COR, dome screw holes, beveled anterior and superior rim with screw holes directed into the posterior column, and highly porous titanium coating (17,18). In addition, shell implantation is performed with a standard technique and instrumentation. It has been previously demonstrated that this shell produces less elevation of hip COR in two radiographic studies (17,19).
However, there is a paucity of studies concerning the use of this acetabular shell in difficult primary total hip arthroplasty cases. Therefore, the purpose of this case report series was to demonstrate the use of this newer offset COR acetabular shell design in several commonly encountered difficult primary total hip arthroplasty cases.
Case 1
History
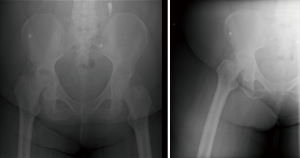
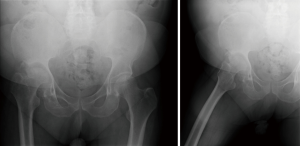
A 68-year-old female presented for an evaluation of a 3-year history of left hip pain localized to the groin. She had been using a walker to ambulate. Examination revealed very limited motion secondary to pain with flexion to 95˚, external rotation to 25˚, internal rotation to 10˚, and a flexion contracture of 15˚. Antero-posterior and frog-leg lateral radiographs demonstrated severe osteonecrosis with collapse of the femoral head and obliteration of the joint space (Figure 1). Given the advanced stage of her osteonecrosis, the patient was counseled and agreed to undergo a right total hip arthroplasty. A preoperative computerized tomography (CT) of the hip was performed.
Operative details
A posterior approach to the hip was performed using an extensile dissection due to morbid obesity. The adipose layer was dissected and elevated, the fascial layer was then split in line with the skin incision. The femoral head was found to be extremely small with marked collapse.
The patient was found to have a large superior defect and a very high hip center of rotation. A posterior intracapsular pin was placed in the ischium for orientation, as well as for retraction of the posterior capsule. The pre-operative plan demonstrated size 58 shell. The reamer was set to 40 degrees of abduction and 25 degrees of anteversion. The bone appeared to be of a good quality with circumferential bleeding, except for the superior ileum defect. Because of the superior defect, the surgeon decided that a Restoration Anatomic Shell (Stryker, Mahwah, New Jersey) would be of benefit in this case. A 60 mm shell was impacted in 40 degrees of abduction and 25 degrees of anteversion. A 40 mm dome screw was placed into the ilium with excellent purchase. Another dome screw was placed in the ischium followed by a rim screw.
A standard femoral stem was used with a +3 neck, which resulted in equal leg lengths. The patient had full passive flexion, internal rotation to 60 degrees, with no instability or impingement. The hip was reduced and leg lengths were again confirmed. The hip was irrigated and the wound closed.
Postoperative course
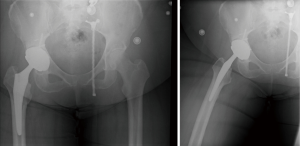
At 1 postoperative year, she had a non-antalgic gait without the use of any ambulatory aids. She had no complaints and reported no pain. She was able to extend her hip to 0˚, and flex to 125˚. The antero-posterior and frog-leg lateral radiographs demonstrated well-fixed acetabular and femoral components with no signs of loosening or osteolysis and restored COR of the hip (Figure 2).
Case 2
History
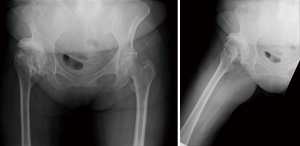
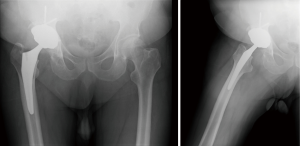
The patient is a 63-year-old female who presented for initial evaluation of severe, continuous right hip pain. Her pain had been present for about 40 years, but, until recently, had previously been intermittent. As a child, she was diagnosed with hip dysplasia, sustained multiple dislocations, but was treated non-operatively. Recently, the pain became worse, at times 10 out of 10. She was ambulating with a noticeable antalgic gait and had a marked leg-length discrepancy which was very bothersome for her. Examination revealed hip flexion to 80˚, external rotation of only 15˚, and internal rotation of only 5˚. She had pain with motion and crepitus, and her right leg is 2 cm shorter than the left. Radiographs demonstrated a severely dysplastic right hip with a large expansile acetabulum and proximal femoral dysplasia (Figure 3).
Operative details
An extensile posterior approach to the hip was utilized similarly to case #1. There was an extremely large and flattened out femoral head. A clear delineation between the lesser trochanter and the remainder of the neck was made by removing osteophytes, and the femoral neck cut was performed. The acetabular shell was shallow and flattened. The preoperative plan template was for a 62 mm shell. Therefore, the initial reaming was performed with a 54 mm reamer at 40˚ of abduction and 24˚ of anteversion. This was followed by 56, 58, and 60 mm reamers. The hip center was very high, and the surgeon decided to utilize an offset center-of-rotation acetabular shell. A 60 mm offset shell was impacted in 40˚ of abduction and 24˚ of anteversion and secured with two dome screws into ileum, one dome screw into the ischium, and one rim screw. A 38 mm dual mobility liner was impacted in place. A standard proximal femoral stem with standard offset, 132˚ neck angle, and neutral neck length was utilized.
Postoperative course
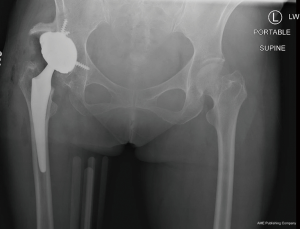
At her post-operative 1 year visit, she had a non-antalgic gait with a one-point cane and markedly improved overall gait. The range of motion was approximately 130˚ of flexion, 50˚ of external rotation, and 40˚ of internal rotation. She had good strength of her hip flexors and abductors. The antero-posterior radiograph demonstrated well maintained acetabular component with no signs of loosening or osteolysis (Figure 4).
Case 3
History
A 60-year-old man presented for an initial evaluation of a two-year history of right hip pain, which started after a native joint infection treated with a drain and intravenous antibiotics. Examination revealed limb-length discrepancy of approximately 2 to 3 cm, right hip flexion of only 95˚, limited extension, external rotation to 35˚, and internal rotation to 15˚. Radiographs revealed complete obliteration of his right hip, a very large expansile defect of the right acetabulum, and severe degeneration of his femoral head with multiple loose bodies (see Figure 5). He elected to undergo a right total hip arthroplasty. Prior to the surgery, a pre-operative infection work up, including aspiration and erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) evaluations, were performed, all tests came back negative.
Operative details
A similar surgical procedure to cases 1 and 2 was performed. After surgical exposure, synovial tissue biopsies were taken as well as biopsies of the femoral head, which were sent to pathology. This demonstrated no neutrophils under high power field from multiple sectors. The femoral neck was cut, and scar tissue was debrided inferiorly and circumferentially about the acetabulum. The acetabular shell was templated, and there was a large amount of superior migration of the femoral head and acetabular bone loss noted. Therefore, it was decided that offset center-of-rotation acetabular shell would be beneficial. Careful sequential reaming was performed and 64 mm offset shell was impacted at 40˚ of abduction and 25˚ of anteversion. Three screws were placed in the dome, and one in the rim. A size 6 high offset femoral stem with a -4 neck and ceramic head was used.
Postoperative course
At his latest postoperative visit, he had a non-antalgic gait with four-wheel walker. He had good range-of-motion and good strength of his hip flexors and hamstrings. The antero-posterior radiograph demonstrated well maintained acetabular component in good position (see Figure 6). The patient currently ambulates with no assistive devices, no limp, and no pain with the ability to walk greater than 2 miles.
Discussion
Several conditions may predispose patients to development of antero-lateral and superior acetabular bone deficiencies, including developmental dysplasia of the hip, osteonecrosis, or septic arthritis among others (1,2). This may compromise acetabular component stability and impair reliable fixation. In addition to the immediate fixation and stability of the implant, the mid- and long-term stability may be compromised. Several methods of improving acetabular component stability and coverage have been utilized. Recently, a new acetabular shell was developed with a goal of maintaining the native hip COR while achieving excellent fixation with a standard instrumentation and technique. Previous radiographic studies have demonstrated the efficacy of this shell in lowering hip COR (19). In this case series we demonstrate the use of this new shell in patients with difficult hip pathologies.
In a recently performed radiographic evaluation study (19), the authors analyzed 29 radiographs of patients with offset center-of-rotation cups and 58 jumbo cups. The group found the mean vertical COR in the offset COR cohort (3.5 mm; range, −12 to 15 mm; mean difference, −7.3 mm; 95% CI, −13.2 to −1.5) to be smaller than that for the jumbo cup cohort (10.5 mm; range, −4 to 50 mm; mean difference, 7.3 mm; 95% CI, −12.5 to −2.2; P=0.003). Faizan et al. (17) performed a computer simulation, in vitro study, assessing the center-of-rotation of the hip, and screw trajectories of the offset center of rotation acetabular shell also evaluated in this study. The newer shell had less of the vertical displacement when compared to jumbo cup for both large (4 vs. 8.8 mm) and small (2.1 vs. 2.2–5.3 mm) diameters. Furthermore, there were substantially, up to 300% more, fixation options for the new shell.
Conclusions
Based on this case series, we have presented how this new offset acetabular shell may help bring down the center-of-rotation of the hip in difficult primary cases, which may otherwise be quite challenging utilizing conventional techniques. With a more normal center-of-rotation, one can potentially expect better abductor tensioning with more normal hip mechanics resulting in better short- and long-term outcomes.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patients for publication of this manuscript and any accompanying images.
References
- Issa K, Pivec R, Kapadia BH, et al. Osteonecrosis of the femoral head: the total hip replacement solution. Bone Joint J 2013;95-B:46-50. [Crossref] [PubMed]
- Dudkiewicz I, Salai M, Chechik A, et al. Total hip arthroplasty after childhood septic hip in patients younger than 25 years of age. J Pediatr Orthop 2000;20:585-7. [Crossref] [PubMed]
- Guan M, Zhou G, Li X. A simple technique to strengthen the initial and mid-term to long-term stability of the cup during total hip arthroplasty in developmental dysplasia of the hip. Saudi Med J 2018;39:342-6. [Crossref] [PubMed]
- Iwase T, Morita D, Ito T, et al. Favorable Results of Primary Total Hip Arthroplasty With Acetabular Impaction Bone Grafting for Large Segmental Bone Defects in Dysplastic Hips. J Arthroplasty 2016;31:2221-6. [Crossref] [PubMed]
- Mont MA, McGrath MS, Bonutti PM, et al. Anatomic and physiologic rationale for various technologies for primary total hip arthroplasty. Expert Rev Med Devices 2009;6:169-86. [Crossref] [PubMed]
- Chen WM, Engh C, Hopper RH, et al. Acetabular revision with use of a bilobed component inserted without cement in patients who have acetabular bone-stock deficiency. J Bone Joint Surg Am 2000;82:197-206. [Crossref] [PubMed]
- Dearborn JT, Harris WH. Acetabular revision arthroplasty using so-called jumbo cementless components: an average 7-year follow-up study. J Arthroplasty 2000;15:8-15. [Crossref] [PubMed]
- Fan CY, Chen WM, Lee OK, et al. Acetabular revision arthroplasty using jumbo cups: An experience in Asia. Arch Orthop Trauma Surg 2008;128:809-13. [Crossref] [PubMed]
- Gustke KA. Jumbo Cup or High Hip Center Is Bigger Better 2004;19:120-3.
- Nwankwo CD, Ries MD. Do jumbo cups cause hip center elevation in revision THA? A radiographic evaluation. Clin Orthop Relat Res 2014;472:2793-8. [Crossref] [PubMed]
- Nwankwo C, Dong NN, Heffernan CD, et al. Do Jumbo Cups Cause Hip Center Elevation in Revision THA? A Computer Simulation. Clin Orthop Relat Res 2014;472:572-6. [Crossref] [PubMed]
- Zhang Z, Wu P, Huang Z, et al. Cementless acetabular component with or without upward placement in dysplasia hip: Early results from a prospective, randomised study. J Orthop 2017;14:370-6. [Crossref] [PubMed]
- Chen M, Luo ZL, Wu KR, et al. Cementless Total Hip Arthroplasty With a High Hip Center for Hartofilakidis Type B Developmental Dysplasia of the Hip: Results of Midterm Follow-Up. J Arthroplasty 2016;31:1027-34. [Crossref] [PubMed]
- Jauregui JJ, Banerjee S, Elmallah RK, et al. Radiographic Evaluation of Hip Dislocations Necessitating Revision Total Hip Arthroplasty. Orthopedics 2016;39:e1011-8. [Crossref] [PubMed]
- Dargel J, Oppermann J, Bruggemann GP, et al. Dislocation following total hip replacement. Dtsch Arztebl Int 2014;111:884-90. [PubMed]
- Brooks PJ. Dislocation following total hip replacement: causes and cures. Bone Joint J 2013;95-B:67-9. [Crossref] [PubMed]
- Faizan A, Black BJ, Fay BD, et al. Comparison of Head Center Position and Screw Fixation Options Between a Jumbo Cup and an Offset Center of Rotation Cup in Revision Total Hip Arthroplasty: A Computer Simulation Study. J Arthroplasty 2016;31:307-11. [Crossref] [PubMed]
- Ries MD. The jumbo cup: Curtain calls and caveats. Semin Arthroplasty 2014;25:151-5. [Crossref]
- Khlopas A, Chughtai M, Elmallah RK, et al. Novel Acetabular Cup for Revision THA Improves Hip Center of Rotation: A Radiographic Evaluation. Clin Orthop Relat Res 2018;476:315-22. [Crossref] [PubMed]


