
A rare presentation of pleomorphic carcinoma of lung mimic empyema
Introduction
Pleomorphic carcinoma (PC) of lung is a relatively rare malignant tumor of lung which has been reported to have low incidence from 0.1% to 0.4% of all lung cancers (1,2). According to the classification from World Health Organization (WHO), PC was defined as poorly defined as poorly differentiated adenocarcinoma, squamous cell carcinoma, or large cell carcinoma containing sarcomatoid components of spindle or/and giant cell at 10% of the cells or a carcinoma comprised entirely of giant and spindle cells (3), as a subtype of sarcomatoid carcinomas. PC is considered to occur on male smokers at over 65 years of age usually in most of reports. The clinical presentations of PC are various and non-specific which may delay the diagnosis and management. In this study, we report a case of PC with a patient who has a non-classical background with unusual symptoms.
Case presentation
A 40-year-old female non-smoker without any past medical history initially presented with epigastric fullness and intermittent abdominal pain followed by nausea and dyspnea for three weeks. No chills, cough and chest pain were reported. A massive exudative pleural effusion in her right pleural cavity was detected by chest X-ray (CXR) and computed tomography (CT) after she was admitted at previous hospital. No obvious lung mass or nodule was detected by the CT scan. However, her symptoms had been not improved after a pigtail catheter was inserted for amount of pleural effusion drainage and cytology for one week. As a result, she was transferred to our hospital for further management.
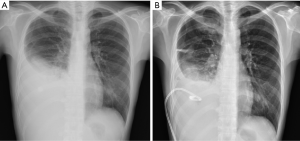
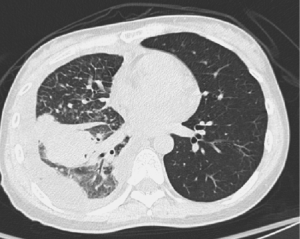
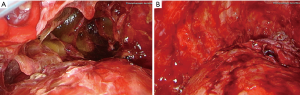
Fever and moderated dyspnea were developed when she was admitted to our hospital. A severe effusion at right hemithorax was detected again. The pleural effusion analysis showed highly elevated lactic dehydrogenase (LDH) (3,376 U/L) and reactive mesothelial cells and inflammatory cells rather than malignant cells were detected by cytological exam. Chest CT was performed again for excluding possible malignant lesion. The report of chest CT did not mention any mass or nodule although right lung cancer with massive right pleural effusion, cT4N2M1a (stage IV), was still considered as a differential diagnosis. According to her symptoms and the result of associated investigations, empyema at right pleural cavity was considered. Thus, she was required to admit. Empiric antibiotics and pigtail catheter insertion were provided as the appropriate management for empyema. The results of CXR and chest CT were demonstrated in Figures 1 and 2 respectively. Her symptoms, however, did not subside two days after treatment. For checking the cause and controlling her symptoms, pleural decortications via video-assisted thoracic surgery (VATS) was performed for diagnosis and mechanical pleurodesis. During VATS, massive red jelly-like pleura at right thoracic cavity was discovered. Red and sticky fluid was produced from the affect pleura. A pleural wall tissue biopsy was also delivered during VATS. The images of VATS were showed in Figure 3. Her symptoms were gradually improved after decortications. Other relevant investigations including abdominal sonography and bone scan were also provided for excluding other possible metastatic malignancy. Apart from mild elevation of tumor marker CA-125 (63.5 μ/mL), the rest of results were unremarkable. She was discharged 10 days after the procedure and treated as an outpatient.
Unfortunately, PC of right lower lobe of lung was diagnosed by pathological exam. She presented to our emergency department (ED) with severe chest pain and dyspnea four days after discharge. Her symptoms were deteriorated rapidly. Thus, she was admitted again for advanced medical control. However, her symptoms could not be controlled effectively. Palliative care was requested and this patient expired with severe pleural effusion at right thoracic cavity five days after this admission.
Discussion
The PC of lung is a rare lung cancer with extremely poor prognosis. According to studies, the survival rate of patients with advanced stage of PC is 22.8 months (4). Furthermore, the presentations of PC are various and unspecific. Common unspecific respiratory symptoms including dyspnea and cough for patient with PC were reported previously (5). More asymptotic patients with PC were detected by chest CT coincidently during general health-check (6). A patient with advanced stage of PC presented with symptoms like empyema initially was extremely rare.
In our case, this middle-age and healthy female patient without smoking history presented with unspecific symptoms initially and her image also demonstrated the characteristics of empyema. Empyema was commonly considered as first impression. Moreover, the advanced PC diagnosed on this patient with unspecific symptoms was not common in the early presentation. Regarding associated investigations, there is not a highly sensitive test for PC apart from pathological exam via biopsy although several antibodies are available to detect pulmonary epithelial tumor (5). According to Poe and Khan et al. (7,8), the sensitivity of the cytology of pleural effusion for diagnosing lung cancer was about 65% and the sensitivity of pleural biopsy via thoracoscopy was about 85%. As a result, it was relatively difficult to detect this problem on her before the VATS was performed.
Although the treatments of lung cancer including PC are various such as surgical recession, chemotherapy, target therapy radiotherapy and immunotherapy based on the stage of cancer (9), no one was considered as an effective way to approach PC. The survival rate of PC after treatment is still poor. The median survival time for patients with advanced PC receiving surgical resection or chemotherapy was few months as Chang et al. reported (10). Fishback and Rossi et al. also mentioned disappointed results in their studies (2,11). The extremely poor prognosis occurred in our case. She expired two months after she had developed these empyema-like symptoms initially. In conclusion, pleomorphic carcinoma is a rare lung cancer with various signs and symptoms. It may occur in female non-smokers with middle age although the typical candidate of PC is in the group of old male smokers. PC can present like empyema with massive pleural effusion initially. As a result, PC should be considered as one of differential diagnoses if patients’ symptoms did not subside after pleural effusion drainage and appropriate antibiotics had been given.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Ishida T, Tateishi M, Kaneko S, et al. Carcinosarcoma and spindle cell carcinoma of the lung: Clinicopathologic and immunohistochemical studies. J Thorac Cardiovasc Surg 1990;100:844-52. [PubMed]
- Fishback NF, Travis WD, Moran CA, et al. Pleomorphic (spindle/giant cell) carcinoma of the lung. A clinicopathologic correlation of 78 cases. Cancer 1994;73:2936-45. [Crossref] [PubMed]
- Travis WD, Brambilla E, Muller-Hermelink HK, et al. eds. World Health Organization Classification of Tumors: Pathology and Genetics of Tumours of the Lung, Pleura, Thymus and Heart. Lyon: IARC Press; 2004:53-8.
- Ito K, Oizumi S, Fukumoto S, et al. Clinical characteristics of pleomorphic carcinoma of the lung. Lung Cancer 2010;68:204-10. [Crossref] [PubMed]
- Zhang X, Wang Y, Zhao L, et al. Pulmonary pleomorphic carcinoma: A case report and review of the literature. Medicine (Baltimore) 2017;96:e7465. [Crossref] [PubMed]
- Kato D, Chihara Y, Shirase T, et al. Successful treatment of two consecutive cases of pulmonary pleomorphic carcinoma with platinum chemotherapy. Oncol Lett 2015;10:3040-42. [Crossref] [PubMed]
- Poe RH, Israel RH, Utell MJ, et al. Sensitivity, Specificity, and Predictive Values of Closed Pleural Biopsy. Arch Intern Med 1984;144:325-8. [Crossref] [PubMed]
- Khan SL, Haris M, Munavvar M, et al. Diagnostic accuracy of pleural fluid cytology compared to pleural biopsy histology obtained via thoracoscopy. Eur Respir J 2014;44:2775.
- Zappa C, Mousa SA. Non-small cell lung cancer: current treatment and future advances. Transl Lung Cancer Res 2016;5:288-300. [Crossref] [PubMed]
- Chang YL, Lee YC, Shih JY, et al. Pulmonary pleomorphic (spindle) cell carcinoma: peculiar clinicopathologic manifestations different from ordinary non-small cell carcinoma. Lung Cancer 2001;34:91-7. [Crossref] [PubMed]
- Rossi G, Cavazza A, Sturn N, et al. Pulmonary Carcinomas With Pleomorphic, Sarcomatoid, or Sarcomatous Elements: A Clinicopathologic and immunohistochemical study of 75 cases. Am J Surg Pathol 2003;27:311-24. [Crossref] [PubMed]


