
Cardiac penetrating injury: a rare complication associated with the lung nodule localization by hookwire
Case presentation
A 48-year-old woman was firstly admitted 2 years ago because of multiple pulmonary nodules with two nodules in the left upper lobe, one ground-glass opacity (GGO) in the left lower lobe, and one in the right upper lobe. At that time, a left upper lobectomy and left lower wedge resection by video-assisted thoracoscopic surgery (VATS) were performed for the left three dominant nodules with pathological diagnosis being multiple primary lung adenocarcinoma, and the nodule in the right lung was managed with regular computed tomography (CT) follow-up because of its small size and lack of solid component. In the recent CT follow-up examination, nodule growth was detected for the remaining nodule in the right lung. Therefore, anterior lung segmentectomy of the right upper lobe by VATS was planned. Because the nodule was less than 2 cm and had a deep location, preoperative lung nodule localization with hookwire system was implemented to facilitate nodule recognition in the resected specimen. Written informed consent was obtained from the patient for publication of this case report and any accompanying images.
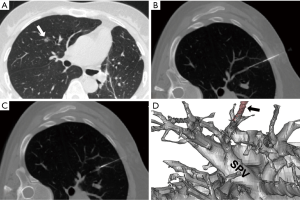
The CT-guided hookwire localization was performed with local anesthesia 2 hours before the operation in the CT department. Under the surveillance of CT scan, the hookwire (20-gauge, Pajunk, Germany) was inserted 3 cm deep into the lung surface, just adjacent to the lesion. There was no pneumothorax or intrapulmonary hemorrhage after this procedure (Figure 1). The patient was then wheeled into operation room. Anesthesia was performed with double lumen intubation, and a 3 cm incision was made on the anterior axillary line at the fourth intercostal space. At the time of entering thorax, the hookwire was visible and its tail was cut off to avoid hindering the operation.
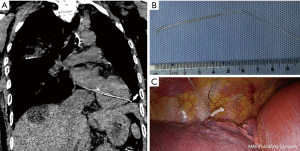
We successively dissected the horizontal fissure, anterior segmental artery, anterior segmental vein, and anterior segmental bronchi. After the anterior segmental pulmonary tissue was removed and the lung nodule was successfully identified in the resected lung specimen, we found that the hookwire mysteriously disappeared. At first it seemed that it had been left in a corner of the thoracic cavity. After searching at least 2 hours and extending the incision from 3 to 10 cm, the hookwire was not found. The imaging department was asked, and the chest X-ray, which was filmed in the operating room, showed the hook-wire was still situated in the left thoracic cavity. To pinpoint the location of the hookwire, we temporally sutured the incision and performed a CT scan in the radiography room with the help of a portable ventilator. As shown on the CT scan, the hookwire had horizontally penetrated the ventricular wall with the tip of hookwire in the pericardial sac (Figure 2A). The patient was then sent back to the operating room, and an 8-cm incision was made in the seventh intercostal space on the left side under the X-ray guidance. After opening the pericardium, the hookwire was seen and carefully extracted using thoracic forceps (Figure 2B). During the process of hookwire removal, the patient did not have any arrhythmias or endocardial hemorrhaging. The patient was eventually discharged seven days after the operation with an uneventful postoperative recovery. The pathological results indicated primary lung adenocarcinoma.
Discussion
CT-guided hook wire is currently the most commonly used methods for percutaneous lung nodule localization (1). Associated complications including preoperative localizer dislodgement, pneumothorax, intrapulmonary hemorrhaging, and air embolism have been reported (2,3). However, a penetrating cardiac injury, which is an extremely rare complication, has never been reported to date to our knowledge.
We speculated that because the hookwire was placed too close to the anterior segmental pulmonary vein, it was able to insert into the superior pulmonary vein and left ventricle under the influence of blood flow and lung manipulation. The hookwire cannot be forcefully reversed due to its hook-shaped tip. Fortunately, the hookwire had penetrated the myocardium and gone into pericardial cavity, and we were able to easily remove it after opening the pericardium without performing ventriculotomy.
In our opinion, several lessons can be learned from this case to avoid this complication in the future: (I) pulmonary vasculature should be avoided as far as possible during localization procedure; (II) because the superficial lung nodule can be easily identified after the pleura was marked, the hookwire should be pulled out from lung parenchyma at the beginning of the operation to avoid the risk of hookwire migration when the nodule is near the pleura; (III) the hookwire should be fixed by a device such a ham-lock to prevent it from sliding into the lung further if the nodule is deep into the lung (Figure 2C); (IV) most importantly, unnecessary mobilization and manipulation of the lung parenchyma should be avoided.
Acknowledgements
Funding: The study was funded by the grant 2016YFC0905403 and 2016YFC0905402 from National Key R&D Program of China and the grant 2014YQ03 from Shanghai Pulmonary Hospital.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this case report and any accompanying images.
References
- Park CH, Han K, Hur J, et al. Comparative Effectiveness and Safety of Preoperative Lung Localization for Pulmonary Nodules: A Systematic Review and Meta-analysis. Chest 2017;151:316-28. [Crossref] [PubMed]
- Mullan BF, Stanford W, Barnhart W, et al. Lung nodules: improved wire for CT-guided localization. Radiology 1999;211:561-5. [Crossref] [PubMed]
- Ichinose J, Kohno T, Fujimori S, Harano T, Suzuki S. Efficacy and complications of computed tomography-guided hook wire localization. Ann Thorac Surg 2013;96:1203-8. [Crossref] [PubMed]


