
Discharge to the skilled nursing facility: patient risk factors and perioperative outcomes after total knee arthroplasty
Introduction
The setting of physical therapy after total knee arthroplasty (TKA) varies, ranging from inpatient rehabilitation facility, skilled nursing facility (SNF), or home care (1,2). Those patients who fail to meet either the criteria for outpatient physical therapy or an inpatient rehabilitation facility are often discharged to SNFs. To date, several predictors are common to patients being discharged to acute rehabilitation facilities following TKA, namely living status, age, pre-operative systemic health and medical insurance, in addition to the functional testing outcomes, length of hospital stay, and pain management (3-5).
SNFs have historically provided both long-term residential care and short-term post-acute rehabilitation visits, but have increasingly shifted focus to cater to post-operative, post-acute rehabilitation needs (2,6,7). In a recent 2014 Medicare survey on SNF usage, 65% of residents in nursing homes were over the age of 75 years, with more than 60% with impairments of four or more activities of daily living (ADLs) (6,8). When compared to inpatient rehabilitation, patients in SNFs may not receive the continuous benefits of a dedicated postoperative rehabilitation program (7). In addition, many primary lower extremity total joint arthroplasty studies identified post-acute care as a focal point to improve outcomes and reduce cost of care (9-12). As a result, understanding the risk factors and predictors resulting in non-home discharges is important for clinicians to optimize post-operative outcomes and reduce costs (2,5,11,13).
As more patients are being discharged to SNFs, which may provide variable and unpredictable post-operative rehabilitation, it is important to understand the factors that result in this disposition status. In order to better characterize the patients predisposed to a SNF discharge post-TKA and quantify the peri-operative risks incurred, we used a nationwide TKA database to compare who were and were not discharged to SNFs with respect to: (I) patient and hospital characteristics; (II) comorbidities; (III) lengths of stay (LOS); and (IV) inpatient complications.
Methods
Patient selection
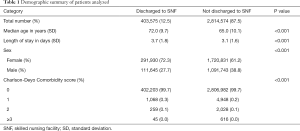
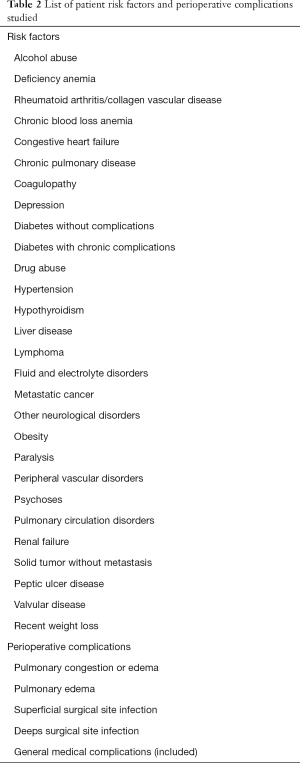
The National Inpatient Sample (NIS) database was queried for all individuals who received a primary TKA using the International Classification of Disease, Ninth Revision, Clinical Modification (ICD-9-CM) 81.54 between the years 2009 and 2013. The NIS database is developed and maintained through private-government partnership and is a valid representation of all non-federal in-patient hospitalizations in the United States during their respective years (14,15). Our query for primary TKA yielded 3,218,419 patients. The patient demographics and pre-operative factors that were recorded for each patient included: sex, age, race, region, hospital bed size, teaching status, and hospital control/ownership. See Table 1 for demographics. The comorbidities and risk factors, as well as perioperative complications studied, can be found in Table 2. Length-of-stay for each in-patient admission was also recorded. The relevant regions for the NIS database are obtained from the AHA Annual Survey of Hospitals, with the Census region is defined by the U.S. Census Bureau, namely the Northeast, Midwest, South, and West. All noted comorbidities, including psychoses, peripheral vascular disorders, and neurological disorders were based off of the Agency for Healthcare Research and Quality (AHRQ) comorbidity classification available in NIS disease severity measures files.
Full table
Full table
Data analysis
Charlson-Deyo comorbidity score was calculated to assess patient comorbidity status. Continous and categorical variables were assessed via independent samples t-test and chi-square analysis respectively. Mann-Whiney U test was used for non-parametric continuous data with the median value reported. A multi-level logistic regression analysis was conducted using patient and hospital specific factors as predictor variables in order to generate odd ratios. A two-tailed P value of 0.05 was set as the threshold for statistical significance.
Results
Patient and hospital characteristics
There were statistically significant differences found between patients discharged to SNFs and patients discharged to home with respect to age, sex, Charlson-Deyo Comorbidity scores, race, hospital size, teaching setting, and hospital ownership. See Table 3 for patient and hospital characteristics. From a demographic perspective, patients discharged to a SNF post-TKA were older (OR 1.07, P<0.001), more likely to be female (OR 1.74, P<0.001), and had a slightly lower Charlson-Deyo Comorbidity scores. Patients discharged to SNFs were more likely to be black (OR 1.246, P<0.001), from the South (OR 1.856, P<0.001), from medium- (OR 1.153, P<0.001) and large-size hospitals (OR 1.354, P<0.001), and be based in rural and community teaching settings (OR 1.083, P<0.001) that are privately owned (OR 1.196, P<0.001).

Full table
Comorbidities
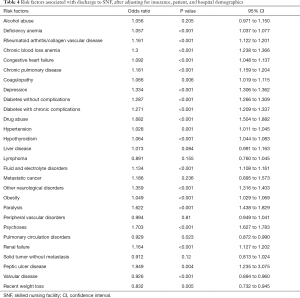
Patients discharged to SNFs were more likely to have comorbidities including: deficiency anemia (OR 1.057, P<0.001), rheumatoid arthritis/collagen vascular disease (OR 1.161, P<0.001), chronic blood loss anemia (OR 1.3, P<0.001), preexisting psychoses (OR 1.703, P<0.001), history of drug abuse (OR 1.682, P<0.001), neurological disorders (OR 1.359, P<0.001), and depression (OR 1.334, P<0.001). Patients discharged to non-SNFs were more likely to have pulmonary circulation disorders, valvular disease, and have recently lost weight. A full summary of pre-operative comorbidities and statistical significance can be found in Table 4.
Full table
Length of stay
Post-operatively, our analysis found that the TKA patients discharged to SNFs had 17% longer mean LOSs (P<0.001) when compared to those who were discharged home.
Inpatient complications
There was statistically significant difference found between patients discharged to SNFs and patients discharged to their home with respect to overall inpatient medical complications related to COPD (OR 1.181, P<0.001), chronic blood loss with anemia (OR 1.3, P<0.001), and diabetes-related complications (OR 1.271, P<0.001). Notably, there was no statistically significant difference found between patients discharged to an SNF and patients discharged to their home with respect to superficial surgical site infection and deep surgical site infection. A full summary of intra-operative complications can be found in Table 5.

Full table
Discussion
Many primary lower extremity total joint arthroplasty studies identified post-acute care as a focal point to improve outcomes and reduce cost of care (11,12). Indeed, patient discharge disposition following TKA plays a crucial role in determining the total costs, with nearly $2 billion being spent annually on post-operative stays at rehabilitation facilities (16). In addition, when compared to inpatient rehabilitation, patients in SNFs may not receive the continuous benefits of a dedicated postoperative rehabilitation program (7). As a result, understanding the risk factors and predictors resulting in non-home discharges is important for clinicians to optimize post-operative outcomes and decrease costs (2,11,13). To date, several predictors are common to patients being discharged to acute rehabilitation facilities following TKA, namely living status, age, pre-operative systemic health and medical insurance, in addition to the functional testing outcomes, length of hospital stay, and pain management (3,4). This study demonstrated that patients discharged to SNF were more likely to be black, from the South, and from large-size hospitals in community settings. While inpatient, these patients discharged to SNF had more frequent inpatient medical complications. Knowledge of these risk factors may be critical from the perspective of the newly value-based orthopaedic surgeon to intervene early, medically optimize, and preemptively plan with case management care after TKA.
Our study has limitations, consistent with those inherent to many large administrative database studies. The NIS database in particular may not be fully reflective of all national hospital patient discharges as it captures 20% of community hospitals (14). In addition, this database captures data specific to inpatient admission to discharge and is not linked to the past or future encounters of a particular patient. As a result, it does not contain information regarding post-discharge complications and mortality, among other outcomes. However, investigators consider this database to be an appropriate representation of hospital admissions, procedures, diagnoses, and discharges in the United States.
Our findings are largely consistent with other outlined findings. Neuman et al. reported that patients discharged to SNFs after acute-care hospitalization, when risk-adjusted, were not statistically different in terms of performance measures, death, and readmission rates (7). Multiple studies have demonstrated that increased age, female sex, Medicare insurance, living alone, obesity, longer LOS, and persisting postoperative pain are associated with increased risk of non-home discharge after TKA (2,11). The findings that SNF patients had a greater inpatient LOS is in concordance with the report by Sibia et al. (17). As several studies have evaluated drivers for longer LOS in non-home discharge settings for TKA patients, none to our knowledge have evaluated factors implicated in SNF disposition for TKA at a national level. Multiple studies have focused on increased age, female sex, Medicare insurance, living alone, obesity, longer LOS, and persisting postoperative pain to be associated with increased risk of non-home discharge (2,7,17).
Other reports, including that by Keswani et al., identified infection, functional status, history of smoking, diabetes, pulmonary disease, among other risk factors as independent predictors of non-home discharges (12). However, this report is the first to provide the evidence behind particular factors such as depression, deficiency anemia, rheumatoid arthritis, and neurological disorders specifically linked to TKA. Furthermore, it is the first study to specifically evaluate the likelihood of SNF discharge post-TKA specifically.
Conclusions
Our study serves to identify patient demographics and risk factors associated with discharge to SNFs, elucidate medical comorbidities resulting in inpatient complications, and highlight the increased LOS in order to potentially implement early case management planning. Patients discharged to SNF had common demographics and risk factors, increased LOS, more frequent inpatient medical complications, and greater hospital costs. Knowledge of these risk factors may be critical from the perspective of the newly value-based orthopaedic surgeon to intervene early and appropriately select the patient likely and capable of completing the rigorous postoperative TKA rehabilitation.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Meier W, Mizner RL, Marcus RL, et al. Total knee arthroplasty: muscle impairments, functional limitations, and recommended rehabilitation approaches. J Orthop Sports Phys Ther 2008;38:246-56. [Crossref] [PubMed]
- Dejong G, Horn SD, Smout RJ, et al. Joint replacement rehabilitation outcomes on discharge from skilled nursing facilities and inpatient rehabilitation facilities. Arch Phys Med Rehabil 2009;90:1284-96. [Crossref] [PubMed]
- Scott CE, Bugler KE, Clement ND, et al. Patient expectations of arthroplasty of the hip and knee. J Bone Joint Surg Br 2012;94:974-81. [Crossref] [PubMed]
- Belmont PJ Jr, Goodman GP, Waterman BR, et al. Thirty-day postoperative complications and mortality following total knee arthroplasty: incidence and risk factors among a national sample of 15,321 patients. J Bone Joint Surg Am 2014;96:20-6. [Crossref] [PubMed]
- Fry DE, Pine M, Locke D, et al. Prediction models of Medicare 90-day postdischarge deaths, readmissions, and costs in bowel operations. Am J Surg 2015;209:509-14. [Crossref] [PubMed]
- Rahman M, Norton EC, Grabowski DC. Do hospital-owned skilled nursing facilities provide better post-acute care quality? J Health Econ 2016;50:36-46. [Crossref] [PubMed]
- Neuman MD, Wirtalla C, Werner RM. Association between skilled nursing facility quality indicators and hospital readmissions. JAMA 2014;312:1542-51. [Crossref] [PubMed]
- Levine JM, Zulkowski KM. Secondary analysis of office of inspector general's pressure ulcer data: incidence, avoidability, and level of harm. Adv Skin Wound Care 2015;28:420-8. [Crossref] [PubMed]
- Nichols CI, Vose JG. Clinical Outcomes and Costs Within 90 Days of Primary or Revision Total Joint Arthroplasty. J Arthroplasty 2016;31:1400-6.e3. [Crossref] [PubMed]
- Vincent KR, Vincent HK. A multicenter examination of the Center for Medicare Services eligibility criteria in total-joint arthroplasty. Am J Phys Med Rehabil 2008;87:573-84. [Crossref] [PubMed]
- Doran JP, Zabinski SJ. Bundled payment initiatives for Medicare and non-Medicare total joint arthroplasty patients at a community hospital: bundles in the real world. J Arthroplasty 2015;30:353-5. [Crossref] [PubMed]
- Yao DH, Keswani A, Shah CK, et al. Home Discharge After Primary Elective Total Joint Arthroplasty: Postdischarge Complication Timing and Risk Factor Analysis. J Arthroplasty 2017;32:375-80. [Crossref] [PubMed]
- Sharareh B, Le NB, Hoang MT, et al. Factors determining discharge destination for patients undergoing total joint arthroplasty. J Arthroplasty 2014;29:1355-8.e1. [Crossref] [PubMed]
- NIS Database Documentation. Available online: https://www.hcup-us.ahrq.gov/db/nation/nis/nisdbdocumentation.jsp. Accessed November 30, 2017.
- Gwam CU, Mistry JB, Mohamed NS, et al. Current Epidemiology of Revision Total Hip Arthroplasty in the United States: National Inpatient Sample 2009 to 2013. J Arthroplasty 2017;32:2088-92. [Crossref] [PubMed]
- Mallinson TR, Bateman J, Tseng HY, et al. A comparison of discharge functional status after rehabilitation in skilled nursing, home health, and medical rehabilitation settings for patients after lower-extremity joint replacement surgery. Arch Phys Med Rehabil 2011;92:712-20. [Crossref] [PubMed]
- Sibia US, Turcotte JJ, MacDonald JH, et al. The Cost of Unnecessary Hospital Days for Medicare Joint Arthroplasty Patients Discharging to Skilled Nursing Facilities. J Arthroplasty 2017;32:2655-7. [Crossref] [PubMed]


