The effect of operative time on in-hospital length of stay in revision total knee arthroplasty
Introduction
Revision total knee arthroplasty (TKA) is associated with worse patient outcomes when compared to primaries, including increasing blood loss, bone loss, readmissions, prolonged lengths-of-stay (LOS), and increased operative time (1,2). Nichols et al. performed an analysis of 526,481 total joint arthroplasty (TJA) patients, including 25,354 revision TKAs, in order to determine differences in costs and complications in primary versus revision arthroplasty. Within this cohort, revision arthroplasty was associated with increased rates of readmissions, complications, longer LOS, discharges to nursing facility, and transfusions as well as higher 90-day costs (2). These results indicate that there is room for improvement in the treatment of revision arthroplasty patients. With the increasing need for revision surgeries, there is increasing importance in identifying modifiable variables for these patients.
Operative times have historically been identified as an important factor in postoperative outcomes for TKA. Increasing operative times are associated with worse outcomes, such as increased rates of infections, thromboemboli, neurologic deficits, revisions, and other complications (3-10). Young et al. analyzed 61,438 TKAs in the New Zealand Joint Registry over a 13-year period and found increasing revision rates with operative times longer than 120 minutes (P<0.01) (10). Duchman et al. studied 99,444 patients undergoing TJA and found older age, obesity, and ASA 3 or 4 predicted an operative time greater than 120 minutes. This cohort showed increasing complication rates (5.9%) with operative times greater than 120 minutes compared to those less than 120 minutes (4.6% to 4.8%, P<0.001) (3). In a study of 353 TKAs, including primary and revisions, Peersman et al. found that operative times for patients who developed infections after TKAs were 33 minutes longer than for those who did not develop SSIs (P<0.001) (9). Additionally, revisions, bilateral surgery, medical comorbidities, morbid obesity, and any prior open surgery were considered risk factors for longer operative time (9). Many of the studies identifying the association between operative time and complications investigate primary TKAs. However, revision surgeries have longer procedure times and higher innate infection rates, which potentially portend even greater risk.
Increasing LOS has also been associated with higher complication rates, readmissions, and decreased patient satisfaction (11-14). Williams et al. performed an analysis of Medicare TJA patients and found that patients readmitted within 90-day showed significantly longer initial postoperative LOS compared to those that were not readmitted (3.81 vs. 2.10 days, P<0.001) (14). Within this cohort, a LOS greater than 4 days was almost twice as likely to be readmitted (P=0.001) (14). LOS have also been found to be a major driver of cost in TJA, further emphasizing the need to identify factors associated with LOS (15). Several studies have attempted to identify predictors for prolonged LOS in an effort to uncover modifiable risk factors. These include patient age, day of surgery, illness severity scores, female sex, preoperative walking aids, blood transfusions, ASA scores, and in-hospital ambulation (11,16). The elucidation of these risk factors can be utilized to identify patients who may require further in-patient optimization and therapy in order to decrease LOS and improve outcomes.
Revision TKA is an increasingly common, complex problem for both the patient and the surgeon. Prolonged LOS is associated with is associated with higher complication and readmission rates, which can be devastating for these patients. While studies have found that increasing operative time is associated with adverse complications following TJA, the effect increasing operative time may have on LOS has not been fully elucidated. Identification of the association between operative time and LOS, as well as the factors that affect them, can allow for targeted interventions in an effort to improve outcomes. Therefore, the purpose of this study was to: (I) identify predictors of longer operative times; (II) identify predictors of longer LOS; and (III) evaluate the effect of operative time, treated as a continuous and an ordinal variable, on LOS after revision TKA.
Methods
Database
Revision TKA cases were extracted from the American College of Surgeons (ACS) National Surgical Quality Improvement Program (NSQIP) database. The database contains a number of patient and operation specific variables from millions of patients who were reviewed by a trained Surgical Clinical Reviewer are publicly available in the NSIQP database (1). This study was deemed exempt by the Institutional Review Board because the data is de-identified and available publicly.
Study population
A total of 10,723 revision TKAs were identified from the NSQIP database using Current Procedural Terminology (CPT) code 27487 January 01, 2008 and December 31, 2016. Inclusion/exclusion criteria was set so that cases with operative times less than 30 and/or greater than 500 minutes (n=50), body mass indexes (BMIs) less than 15 or greater than 70 kg/m2 (n=66), and those with no reported LOS (n=3) were excluded (0.05%). After removing these cases, a total of 10,604 cases were included in the final analysis.
Study variables
Age, sex, and BMI, as well as operative times and LOS were extracted from each case and compared.
Predictors of operative times
Independent sample t-tests and one-way analysis of variance (ANOVA) were used to compare differences in mean operative times between patient demographics (age, sex, and BMI).
Predictors of LOS
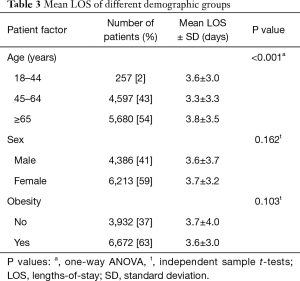
To identify predictors of LOS, mean LOS for were compared between different patient age, sex, and obesity classifications with one-way ANOVA.
Effect of operative times on LOS
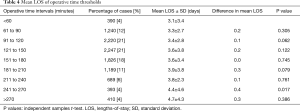
Univariate analyses with one-way ANOVA were performed in order to determine the associations between operative times and LOS. Operative times were separated into 30-minute time interval groups and treated as categorical variables. Mean LOS were determined for each operative time interval and were graphically evaluated to determine the relationship between operative time intervals and LOS.
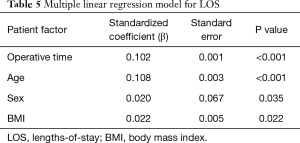
Multivariate analyses were also performed in order to better understand the relationship between operative times and LOS. Multicollinearity among predictors were assessed with variance inflation factors (VIF), with VIFs greater than 3 used to identify potential collinearities. Because no collinearities were identified, all study covariates were included in the multiple linear regression model. A multiple linear regression model was utilized to evaluate the association of LOS with operative times after adjusting for patient factors (i.e., age, sex, and BMI).
Data analysis
Statistical Package for the Social Sciences (SPSS) version 22 for Windows (International Business Machines Corporation, Armonk, NY, USA) was used for data analysis. The threshold for statistical significance was maintained at a P value of less than 0.05.
Results
Study population and study variables
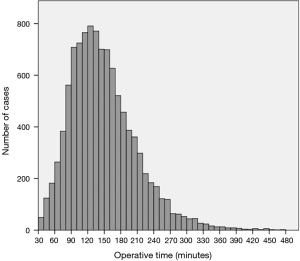
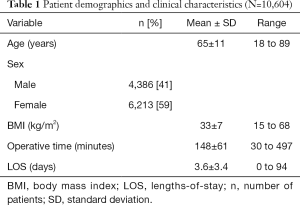
A total of 10,604 cases were included in the final analysis. Within these cases, the patient sample consisted of 6,213 women (59%) and 4,386 men (41%) with a mean age of 65±11 years and a mean BMI of 33±7 kg/m2 (Table 1). Overall, the mean operative time for the study group was 148±61 minutes. The distribution of operative times was positively skewed (Figure 1) with a median operative time of 139 minutes (interquartile range 105 to 181 minutes). The mean LOS was found to be 3.6±3.4 days overall (Table 1).
Full table
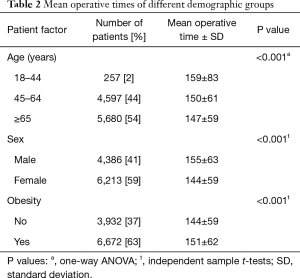
Predictors of operative times
Mean operative times were longer for younger, obese men. This applied to patients between the ages of 18 to 44 years (159±83 minutes), compared with ages 45 to 64 years (150±61 minutes), and 65 years and older (147±59 minutes). Obese patients (BMI >30 kg/m2) had longer mean operative times (151±62 minutes) compared to non-obese patients (BMI <30 kg/m2; 144±59 minutes; P<0.001). Lastly, men had longer mean operative times (155±63 minutes) than women (144±59 minutes; P<0.001) (Table 2).
Full table
Predictors of LOS
Significant relationships between age and LOS (P<0.001) were identified with one-way ANOVA. Patients between the ages of 45 and 64 years had shorter LOS (3.3±3.3 days) compared to patients between 18 and 44 years (3.6±3.0 days), and patients 65 years and older (3.8±3.5 days; Table 3). No significant correlations were found between LOS and sex or BMI.
Full table
Effect of operative times on LOS
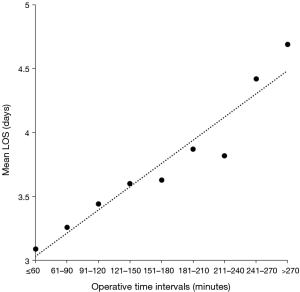
One way-ANOVA revealed relationships between operative time intervals and LOS. Progressively increasing operating time intervals showed progressively increasing differences in mean LOS (Table 4). The trend of increasing mean LOS with increasing operative time intervals was also observed in a line graph (Figure 2).
Full table
After accounting for potential confounding patient factors, a significant association was found between increased operative time and LOS (β=0.102, SE =0.001, P<0.001). Age was also shown to have a significant relationship with LOS (β=0.108, SE =0.003, P<0.001). Significant correlations were also found between LOS and sex (P=0.035) or BMI (P=0.022). These results show that an increase in LOS by 1 day corresponds with a 10-minute increase in operative time (Table 5).
Full table
Discussion
This study aimed to identify the association between operative times and LOS in revision TKA. By analyzing operative times in 30-minute intervals and as a continuous variable, we found significant associations between these two variables. Specifically, as operative times increase, the postoperative LOS increases as well. Additionally, middle-aged patients were found to have longer operative times. When controlling for age, BMI and sex, operative time continued to have the most significant association with LOS.
Identifying the associations between operative times and LOS, as well as the factors that influence them, can be used to target interventions and alter orthopaedic practice. Both longer procedures and increased lengths of surgical stays have been correlated with greater healthcare costs making them a key priority for cost reduction (17,18). Attarian et al. identified several inefficiencies contributing to delays in the operating room including inconsistent staffing, delayed starting time, and poor surgical team coordination. By improving upon these inefficiencies, they were able to decrease LOS and improve upon early discharges (19). These factors may be particularly important in revision arthroplasty, as these procedures tend to be more complex. Therefore, appropriate staffing, communication, and coordination are vital in these cases. Improvements in both surgical processes and patient optimization, may allow for decreased operative time and thus improved patient outcomes.
The findings in this study are similar to the results from several other studies. Keswani et al. also utilized the NSQIP database to analyze revision TJA. This study looked at 4,977 revision TKA and 5,135 revision THA to find factors associated with readmission and LOS >75th percentile. Operative time (OR 1.006, P=0.0001), procedure etiology, age, functional status, higher ASA, higher wound class, and comorbidities were found to be associated with an extended LOS. However, operative times were not found to be associated with readmission rates (20). While this study also used the NSQIP database, it utilized LOS as a categorical variable. Our study aimed to use LOS as a continuous variable and thus decipher its relationship to operative time. Inneh et al. examined 2,638 TKA patients and found that longer operating time (P<0.001), advanced age (P=0.02), and certain preoperative comorbidities were independently associated with a longer LOS, defined as greater than 3 days. Additionally, socio-demographic factors were found to work synergistically in their association with longer LOS (21).
Belmont et al. analyzed 15,321 TKA patients from the NSQIP database between 2006 and 2010 to determine risk factors for 30-day morbidity and mortality. The group identified that, along with morbid obesity (BMI ≥40), age >80 and, ASA ≥3, also, operative time >135 minutes was found to be the most significant predictor of major complications (OR: 1.54). Further analysis showed that prolonged operative time, along with age, ASA, sex, and comorbidities, were associated with a LOS greater than 4 days (OR 1.90) (22). A study by Bohl et al. identified the associations between operative times, stratified into 15-minute intervals, and adverse effects following 165,474 TJA cases (6). This study found that increasing operative time is an independent risk factor for anemia requiring transfusion, sepsis, surgical site infection, urinary tract infection, wound dehiscence, renal insufficiency, readmission, and hospital stay greater than 4 days. In fact, complications proportionally increased for each 15-minute increase in operative time. Risk of surgical site infection, and prolonged LOS each increased by 9% with 15-minute increases in surgical time (6).
Conversely, Liodakis et al. looked at the NSQIP database for aseptic revision arthroplasties between 2011 and 2012 to determine risk factors for complications and LOS greater than 7 days. Age greater than 75 years and hematocrit <35 were predictors of complications in revision TKA. Operative time >180 minutes was found to be a predictor of prolonged hospital stay in revision total hip arthroplasty (P<0.001), but not in revision TKA in univariate (P=0.061) or multivariate (P=0.196) analyses. This study identified only ASA >2, hematocrit <35, and COPD as predictors of LOS >7 days in revision TKA (23). The present study differed in that it used LOS as a continuous variable instead of a cutoff at 7 days, which is significantly longer than the mean LOS seen in our data. Additionally, Liodakis et al. only included aseptic TKAs, which excludes the most common cause of revision. Therefore, this may not reflect the entire scope of revision TKA operative time and LOS.
This study does have some limitations. The retrospective nature of the study meant that the analyzed data was limited to previously collected information. Furthermore, covariates that were taken into consideration only included age, BMI, and sex. Comorbidity scores, such as the Charlson comorbidity index, may also be useful in assessing factors affecting LOS and the inclusion of such variables should be the basis of future work. Nevertheless, this study provides comprehensive predictive and correlative analyses between operative times and LOS on over 10,000 revision TKAs.
Conclusions
Revision TKA is a complex procedure that is associated with higher complication rates and worse patient outcomes compared to primary TKA. Therefore, every effort should be made to identify and improve upon factors that can influence patient outcomes. This study found that operative time had a significant association with LOS and, in fact, has a greater effect than age, sex, and BMI. These results show that interventions to improve operative times may be a valuable target in the effort to reduce LOS as well as hospital costs. The results of this study further underscore the need for improved operating room efficiency and patient optimization in an effort to improve patient outcome, satisfaction, and to reduce overall cost.
Acknowledgements
None.
Footnote
Conflicts of Interest: MA Mont: AAOS, Cymedica, DJ Orthopaedics, Johnson & Johnson, Journal of Arthroplasty, Journal of Knee Surgery, Microport, National Institutes of Health (NIAMS & NICHD), Ongoing Care Solutions, Orthopedics, Orthosensor, Pacira, Peerwell, Performance Dynamics Inc., Sage, Stryker: IP royalties, Surgical Technologies International, Kolon TissueGene. The other authors have no conflicts of interest to declare.
References
- Bunn KJ, Isaacson MJ, Ismaily SK, et al. Quantifying and Predicting Surgeon Work Effort for Primary and Revision Total Knee Arthroplasty. J Arthroplasty 2016;31:59-62. [Crossref] [PubMed]
- Nichols CI, Vose JG. Clinical Outcomes and Costs Within 90 Days of Primary or Revision Total Joint Arthroplasty. J Arthroplasty 2016;31:1400-6.e3. [Crossref] [PubMed]
- Duchman KR, Pugely AJ, Martin CT, et al. Operative Time Affects Short-Term Complications in Total Joint Arthroplasty. J Arthroplasty 2017;32:1285-91. [Crossref] [PubMed]
- Naranje S, Lendway L, Mehle S, et al. Does operative time affect infection rate in primary total knee arthroplasty? Clin Orthop Relat Res 2015;473:64-9. [Crossref] [PubMed]
- Wills BW, Sheppard ED, Smith WR, et al. Impact of operative time on early joint infection and deep vein thrombosis in primary total hip arthroplasty. Orthop Traumatol Surg Res 2018;104:445-8. [Crossref] [PubMed]
- Bohl DD, Ondeck NT, Darrith B, et al. Impact of Operative Time on Adverse Events Following Primary Total Joint Arthroplasty. J Arthroplasty 2018;33:2256-62.e4. [Crossref] [PubMed]
- Ricciardi BF, Oi KK, Daines SB, et al. Patient and Perioperative Variables Affecting 30-Day Readmission for Surgical Complications After Hip and Knee Arthroplasties: A Matched Cohort Study. J Arthroplasty 2017;32:1074-9. [Crossref] [PubMed]
- Ong KL, Lau E, Manley M, et al. Effect of procedure duration on total hip arthroplasty and total knee arthroplasty survivorship in the United States Medicare population. J Arthroplasty 2008;23:127-32. [Crossref] [PubMed]
- Peersman G, Laskin R, Davis J, et al. Prolonged operative time correlates with increased infection rate after total knee arthroplasty. HSS J 2006;2:70-2. [Crossref] [PubMed]
- Young SW, Mutu-Grigg J, Frampton CM, et al. Does speed matter? Revision rates and functional outcomes in TKA in relation to duration of surgery. J Arthroplasty 2014;29:1473-7.e1. [Crossref] [PubMed]
- Husted H, Holm G, Jacobsen S. Predictors of length of stay and patient satisfaction after hip and knee replacement surgery: fast-track experience in 712 patients. Acta Orthop 2008;79:168-73. [Crossref] [PubMed]
- Otero JE, Gholson JJ, Pugely AJ, et al. Length of Hospitalization After Joint Arthroplasty: Does Early Discharge Affect Complications and Readmission Rates? J Arthroplasty 2016;31:2714-25. [Crossref] [PubMed]
- Sutton JC 3rd, Antoniou J, Epure LM, et al. Hospital Discharge within 2 Days Following Total Hip or Knee Arthroplasty Does Not Increase Major-Complication and Readmission Rates. J Bone Joint Surg Am 2016;98:1419-28. [Crossref] [PubMed]
- Williams J, Kester BS, Bosco JA, et al. The Association Between Hospital Length of Stay and 90-Day Readmission Risk Within a Total Joint Arthroplasty Bundled Payment Initiative. J Arthroplasty 2017;32:714-8. [Crossref] [PubMed]
- Rana AJ, Iorio R, Healy WL. Hospital economics of primary THA decreasing reimbursement and increasing cost, 1990 to 2008. Clin Orthop Relat Res 2011;469:355-61. [Crossref] [PubMed]
- Newman JM, Szubski CR, Barsoum WK, et al. Day of Surgery Affects Length of Stay and Charges in Primary Total Hip and Knee Arthroplasty. J Arthroplasty 2017;32:11-5. [Crossref] [PubMed]
- Meyers SJ, Reuben JD, Cox DD, et al. Inpatient cost of primary total joint arthroplasty. J Arthroplasty 1996;11:281-5. [Crossref] [PubMed]
- Moore B, Levit K, Elixhauser A. Costs for Hospital Stays in the United States, 2012: Statistical Brief #181. Healthcare Cost and Utilization Project (HCUP) Statistical Briefs. Rockville (MD) 2006.
- Attarian DE, Wahl JE, Wellman SS, et al. Developing a high-efficiency operating room for total joint arthroplasty in an academic setting. Clin Orthop Relat Res 2013;471:1832-6. [Crossref] [PubMed]
- Keswani A, Lovy AJ, Robinson J, et al. Risk Factors Predict Increased Length of Stay and Readmission Rates in Revision Joint Arthroplasty. J Arthroplasty 2016;31:603-8. [Crossref] [PubMed]
- Inneh IA. The Combined Influence of Sociodemographic, Preoperative Comorbid and Intraoperative Factors on Longer Length of Stay After Elective Primary Total Knee Arthroplasty. J Arthroplasty 2015;30:1883-6. [Crossref] [PubMed]
- Belmont PJ Jr, Goodman GP, Waterman BR, et al. Thirty-day postoperative complications and mortality following total knee arthroplasty: incidence and risk factors among a national sample of 15,321 patients. J Bone Joint Surg Am 2014;96:20-6. [Crossref] [PubMed]
- Liodakis E, Bergeron SG, Zukor DJ, et al. Perioperative Complications and Length of Stay After Revision Total Hip and Knee Arthroplasties: An Analysis of the NSQIP Database. J Arthroplasty 2015;30:1868-71. [Crossref] [PubMed]