
Electronic health records, physician workflows and system change: defining a pathway to better healthcare
Introduction
The current patient care workflow for physicians and healthcare providers includes multi-level communication structures (i.e., doctor-patient communication; doctor-nurse communication, etc.) and a wide variety of data management systems (1). When seeking to understand how to advocate for system changes that might improve workflow, a primary requirement is to first establish a definition and standard description of workflow components. It is also important to review the history behind current workflow structures and acknowledge current system successes as new implementations can disrupt what is already working. A functional and historical review can help to frame current needs and strategies for developing and implementing system changes to improve workflow and patient care.
Physician workflow
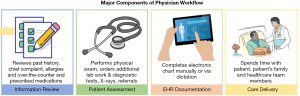
Receiving and reviewing patient related information is a major, early component of the physician workflow (Figure 1). In this process, sources of information include the patient, a colleague or the medical record. The amount of information and the time it takes to review the information is dependent on the circumstances by which the patient sought care and patient location (i.e., ED, ICU, floor, outside hospital, etc.). From a workflow perspective, the efficiency of the information review process is heavily dependent on access and physician experience with the system and the patient’s disease process. The second major component of the physician workflow is patient assessment and examination. Verbal communication with patients is a time-honored tradition and information-rich endeavor. Several research articles cite this part of the physician’s workflow as the one area that has suffered the most with the infiltration of technology into the workflow (2). Specifically, it is estimated that physicians now spend more time on a computer in the review and documentation of patient findings than they spend with the patient. Scribes have been introduced as a systems change that allows physicians to spend more time with their patients (3). Documentation of care as well as diagnostic strategies and treatments appear to be the areas where most physicians spend a significant amount of time. Even with Scribes and dictation capabilities, physicians also use the electronic health record (EHR) for billing and scheduling purposes as well as care coordination once the patient has left the hospital. The delivery of care is also a major component of physician workflow. Making rounds, prescribing medications, performing bedside procedures and major surgical operations are some of the direct care processes that physicians engage in during the practice of patient care. This is also a time-honored, traditional aspect of patient care and is critical to the doctor-patient relationship as well as patient outcomes. These four major components of patient care: (I) information review; (II) patient assessment; (III) EHR documentation and (IV) care delivery are all areas within the physician workflow that can benefit from targeted and strategic system changes. To ensure success, proposed healthcare system changes should be broad, innovative and far reaching to include technology-based innovations as well as innovations in the social-cultural foundations of medicine and communication strategies. The use of Scribes is one example of a foundational, far reaching change that would have had no place in medicine 20 years ago but is now being held as the savior of physician burnout and doctor-patient communication.
Revisiting the history of EHRs and physician workflows
EHRs grew out of an ever-emerging vast array of independent computer systems and software that stored internal hospital processes including billings, pharmacy, laboratory, scheduling, admissions, claims, and visit history. Many of these systems were built to address a specific problem and the thought of interoperability was virtually non-existent during the development process. Physician workflows and the ability to access information from these siloed, independent systems during the process of care was not taken into account. Moreover, there were no avenues that could enable a physician to unify the data they had and the data they needed.
As a result, physicians have a hard time leveraging the information they need to improve patient care. While EHRs were developed to replace paper-based charts and unite some of the previously existing hospital computer systems, current implementation has not met the intended needs. Despite the immense data amounts of stored in EHRs, this electronic system has become a major hindrance to the doctor-patient relationship and information exchange across team members and health systems, which brings the conversation back to physician workflows. There is a critical need to define and quantify workflows for all healthcare providers. Quantification of workflows will help bring to light where the real bottlenecks and inefficiencies exist in the process of care. In defense of the companies that develop and support EHRs, they may have built the best systems possible based on the information and needs expressed at the time of development. Moreover, at inception, implementation of EHRs solved numerous problems relating to efficiency and information access. Twenty years ago, a physician’s workflow included walking to the lab to gather lab values, walking to X-ray to check out radiographs using a library loan model and then documenting care on a paper chart with potentially questionable hand writing. Only now, as healthcare providers have heightened expectations for efficiency and functionality, is the EHR under fire. Overall, you can’t fix what you can’t measure and quantification of physician workflows has risen to the top of the list of critical necessities when planning any new development intended to improve healthcare.
The path to improvement?
With the rapid and continuous insertion of new technologies into the workplace, one thing is clear: Physician’s will always have to take the lead on managing care reporting and documentation while navigating various platforms to coordinate care. This being the case, it is imperative that healthcare providers partner with industry when new technologies are being developed. Having an advocate on the front lines may help to mitigate the downstream effects of technologies that increase disruptions in the workflow without exponential benefits to the patient and providers. When discussing solutions to physician burnout, one group of researchers noted that having the opportunity to be part of something meaningful within the healthcare organization was essential. As such, it is past time for physicians and healthcare providers’ workflows to be seen as part of the solution to improving care.
Acknowledgements
None.
Footnote
Conflicts of Interest: The author has no conflicts of interest to declare.
References
- Carayon P, Schoofs Hundt A, Karsh BT, et al. Work system design for patient safety: the SEIPS model. Qual Saf Health Care 2006;15 Suppl 1:i50-8. [Crossref] [PubMed]
- Carayon P, Wetterneck TB, Alyousef B, et al. Impact of electronic health record technology on the work and workflow of physicians in the intensive care unit. Int J Med Inform 2015;84:578-94. [Crossref] [PubMed]
- Mishra P, Kiang JC, Grant RW. Association of Medical Scribes in Primary Care With Physician Workflow and Patient Experience. JAMA Intern Med 2018;178:1467-72. [Crossref] [PubMed]


