
Broncholithiasis: retrospect of 15 surgical treatment patients
Introduction
Broncholithiasis is defined as the presence of calcified material within a bronchus or within a cavity communicating with a bronchus (1). The majority of broncholiths are peribronchial lymph nodes that have undergone dystrophic calcification subsequent to an inflammatory process, most frequently histoplasmosis or tuberculosis (2).
The clinical presentation of broncholithiasis included cough, hemoptysis and chest pain. In some extreme cases, patients could suffer from life-threatening complications, such as massive hemoptysis or bronchoesophageal fistula. The aim of this study was to discuss the feasibility of surgical treatment and introduce our hospital experience in managing different patients.
Methods
From May 2008 to November 2014, 15 patients were diagnosed as broncholithiasis in Tongji University affiliated Shanghai Pulmonary Hospital, including 2 males and 13 females were focused with a median age of 54 years (range, 36 to 70 years). Three cases had calcification or stones in other organs including kidney, gallbladder and thyroid, 2 had smoking history and 4 had history of tuberculosis. All of these patients received surgical intervention. At the end of March 2015, patients who were completed follow-up are alive and their general condition are stable.
All patients provided written informed consent for the operation and for the inclusion of personal data in a scientific database.
Operative technique
The conventional surgical approaches could be performed to treat broncholithiasis involving lobectomy and/or segmentectomy, with or without bronchoplasty and/or reconstruction of the blood vessels including the pulmonary artery. As the patient had no symptom, we considered to perform segmentectomy only; if the patient had one or more symptoms, we performed lobectomy. On the other hand, if the calcification damaged bronchus, but the pulmonary function should be conserved, we performed lobectomy with bronchoplasty. If the calcification damaged artery and we could not stitch it or we could not decrease the tension of the vessel only by stitched it, we could perform the lobectomy combining with reconstruction of conduit.
Results
All of these 15 patients accepted surgical treatment, 14 of them accepted bronchoscopy before surgery. In order to prevent hemoptysis, fistula or other complications, removal of the broncholithiasis by flexible or rigid bronchoscopy was banned.
In these 15 cases, 12 patients (80%) who had abnormalities of their pulmonary lymph nodes. On the contrary, only 3 cases (20%) had calcification or stones in other organs including kidney, gallbladder, and thyroid, 2 (13.3%) had smoking history and 4 (26.7%) had history of tuberculosis. Therefore, potential connections were existed between broncholithiasis and the other organic calcification, tuberculous, and smoking.
The median age was 54 years among 2 male and 13 female patients (range, 36 to 70 years). Of all the patients, 14 patients had relevant symptoms: 6 patients suffered from cough, 5 suffered from hemoptysis combine with cough, 2 patients suffered from hemoptysis, single 1 patient suffered from hemoptysis combine with chest pain. Since conventional examination found lesions could not distinguish from malignancy, only 1 patient underwent surgical treatment with asymptomatic.
Computed tomography (CT) was performed in 15 patients. Six of them presented hilar or peribronchial calcifications, parenchymal mass could not distinguish from malignancy which was presented in 8 patients, 5 patients presented bronchial distortion, 4 patients presented bronchiectasis, and pulmonary atelectasis was presented in 4 patients.
Bronchoscopy was performed in 13 patients. Broncholiths was diagnosed in 12 patients (endobronchially in 7 and submucosally in 5). The remaining 1 patient had no obvious abnormalities. The abnormal bronchoscopic findings were on the right side in 7 patients (58.3%), on the left side in 5 (41.7%).
Surgical treatment
All patients received surgical treatment. Two patients (13.3%) merely had cough preoperatively, therefore, surgical resection (1 segmentectomy and 1 left lower lobe lobectomy combined with segmentectomy, respectively) was performed by video-assisted thoracic surgery (VATS). In the VATS group, only 1 patient relapsed into cough within 9 months after the initial segmentectomy by VATS. On the contrary, the other patient received VATS which had persistent cough postoperatively.
In the 13-patient group, the surgical approach of choice is thoracotomy, including 9 patients received lobectomy; 2 received lobectomy with bronchoplasty; and 2 received lobectomy combining with reconstruction of the pulmonary artery. No intraoperative complication occurred in these 13 cases (Table 1). Two of 13 patients occurred pyothorax postoperatively, one of them occurred in the left side within 5 days postoperatively. For the other one, pyothorax were occurred in the right side in the sixth day postoperatively, respectively.
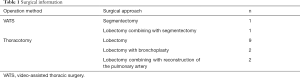
Full table
In process of surgery, we found that calculus often located in the place near bronchus and peripheral vessel. What is more, during the chronic inflammation and recurrent infection, the character of the wall of vessel and bronchus is weak. It made operation hard since it is easy to damage the vessel to bleeding and let the stump of bronchus cannot healing well to fistula. In case of these events in and post of surgery, we must resect the bronchus have enough distance away from lesion.
Surgical pathology
Lymph node dissection was performed combining with lobectomy or segmentectomy if surgeons found lymph nodes had calcification or any other abnormalities. The abnormalities usually were found on the station of paratracheal (station 2), tracheobronchial (station 4), aortopulmonary (station 5), subcarinal (station 7), pulmonary ligament (station 9), hilar (station 10) and interlobar (station 11). Twelve patients (80%) were found abnormalities with their pulmonary lymph nodes. Seven patients had lymphnoditis, the station 4, 5, 12 lymphnoditis had 1 patient; the station 7 and 9 had 2 patients; the station 10 had 5 and the station 11 had 6 patients. Five patients had serious lymph nodes calcification. The station 2 and 4 had 2 patients with lymph nodes calcification and the station 10 had 4 patients. Perhaps, the lymph nodes calcification might consider to be related to broncholithiasis (3).
Follow-up
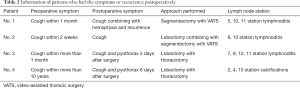
The follow-up was completed in 12 patients (80%) and ranged from 1 to 79 months (median, 44 months), all patients survive in this study. Eight patients (66.7%) were asymptomatic at the time of follow-up, however, the remaining 4 (33.3%) had some form of discomfort: 1 patient suffered from cough, 1 suffered from cough combined with hemoptysis, 2 suffered from lung pyothorax (Table 2). Recurrence of broncholithiasis occurred in the patient who received segmentectomy via VATS that have suffered from cough combined with hemoptysis after surgery. This patient has not received any treatment until now.
Full table
Discussion
Almost all broncholiths originate in the peribronchial lymph nodes, which calcify in response to an inflammatory process. Although the exact mechanism is not fully understood, the process of broncholith formation appears to be related to the precipitation of calcium salts in the alkaline tissue of lung and surrounding lymph nodes during the healing process (4). After calcification, constant respiratory or cardiac motion is believed to cause bronchial wall erosion, producing a broncholith (5). In these 15 patients, it was known that there were 12 patients (80%) who had abnormalities of their pulmonary lymph nodes.
The indications for surgical treatment of broncholithiasis have been well established. They are the complications of broncholithiasis: intractable cough, persistent or massive hemoptysis, suppurative lung disease, bronchiectasis or bronchial stenosis, bronchoesophageal or aortotracheal fistula, and uncertainty about the diagnosis (6). The methods of surgical treatment have been used in broncholithiasis included thoracotomy and VATS. Brantigan revealed that bronchoscopic broncholithectomy had high risk of massive hemoptysis (7). Trastek from Mayo Clinic concluded that thoracotomy is the preferred treatment (8). Surgical management should be chosen first in complicated cases such as obstructive pneumonitis, bronchiectasis, massive hemoptysis, and bronchoesophageal fistulas (9). According to these literatures, surgical treatment was performed but not used bronchoscopic broncholithectomy in these 15 cases.
The goals of treatment should be removal of all calcification and irreversibly damaged bronchi or lung, along with the conservation of as much normal pulmonary parenchyma as possible (10). Bagheri and his colleagues concluded that simple broncholithectomy without pulmonary resection is insufficient, and is accompanied with late complications leading to reoperation (11). The only 1 case who had recurrence was performed segmentectomy with VATS. It would reflect the phenomenon that comparing with VATS, thoracotomy has less risk and it is a sufficient procedure. As the experience we have, the primary surgical approach that aim to treat broncholithiasis is lobectomy. Comparing this surgical method with the same method to treat lung cancer, we concluded that using this method to treat broncholithiasis is more difficult than the same method that is applied to treat lung cancer. The reason is that lobectomy is performed on treating broncholithiasis, which consider the location of calcification of lymph node could corrode bronchus and/or vessels that probably cause some postoperative complications, including hemoptysis, cough, and fistula. In addition, according to patients’ intraoperative characteristics, surgeons would prepare the reconstruction of conduit timely during the initial operation. Since lobectomy via thoracotomy has its advantage to perform the supplementary surgeries, involving reconstruction of vessels and/or bronchus during the operation. Therefore, VATS is not recommended to apply to treat this disease to reduce the risk of surgery and decrease the complications happening. Thoracotomy is the method that would be accepted to cure the patients who suffer from broncholithiasis need to perform surgery first. What is more, according to the curative effect, lobectomy has its advantage since it could reduce the rate of recurrence than segmentectomy. Therefore, surgeries of these 15 patients were performed in lobectomy or lobectomy combining with segmentectomy, not used simple broncholithectomy or segmentectomy. In case of bleeding, any other complications or broncholithiasis recurrence appears in or after surgery, the view of this paper suggests that lobectomy via thoracotomy should be considered as a standard therapy if patients need to receive surgical treatment.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: This work is a retrospective analysis in our single center. The information was revived in the database in our hospital. All patients provided written informed consent for the operation and for the inclusion of personal data in a scientific database. In this phenomenon, we believe that ethics approval is unnecessary.
References
- Dixon GF, Donnerberg RL, Schonfeld SA, et al. Advances in the diagnosis and treatment of broncholithiasis. Am Rev Respir Dis 1984;129:1028-30. [PubMed]
- Bhagavan BS, Rao DR, Weinberg T. Histoplasmosis producing broncholithiasis. Arch Pathol 1971;91:577-9. [PubMed]
- Deslauriers J, Meyerson SL, Patterson A, et al. Pearson’s thoracic & esophageal surgery. 3rd edition. Philadelphia: Churchill Livingstone 2008:532-3.
- Craig K, Keeler T, Buckley P. Broncholithiasis: a case report. J Emerg Med 2002;23:359-63. [Crossref] [PubMed]
- Nollet AS, Vansteenkiste JF, Demedts MG. Broncholithiasis: rare but still present. Respir Med 1998;92:963-5. [Crossref] [PubMed]
- Potaris K, Miller DL, Trastek VF, et al. Role of surgical resection in broncholithiasis. Ann Thorac Surg 2000;70:248-51; discussion 251-2. [Crossref] [PubMed]
- Brantigan CO. Endoscopy for broncholith. JAMA 1978;240:1483. [Crossref] [PubMed]
- Trastek VF, Pairolero PC, Ceithaml EL, et al. Surgical management of broncholithiasis. J Thorac Cardiovasc Surg 1985;90:842-8. [PubMed]
- Menivale F, Deslee G, Vallerand H, et al. Therapeutic management of broncholithiasis. Ann Thorac Surg 2005;79:1774-6. [Crossref] [PubMed]
- Chujo M, Yamashita S, Kawano Y, et al. Left sleeve Basal segmentectomy for broncholithiasis. Ann Thorac Cardiovasc Surg 2008;14:101-4. [PubMed]
- Reza B, Ziaollah H. Surgical management of tuberculous broncholithiasis with hemoptysis: experience with 5 operated cases. Ann Thorac Cardiovasc Surg 2007;13:185-90. [PubMed]


