
Current anti-copper therapies in management of Wilson disease
Introduction
Wilson Disease (WD) is an autosomal recessively inherited disorder of copper metabolism caused by mutations in the ATP7B gene (1,2), which codes for a transmembrane copper transporting ATPase (3,4). WD is a rare with an estimated prevalence of symptomatic disease of 1 in ~30,000 with a heterozygous ATP7B mutation carrier frequency of 1:90 (almost 1% of a population). Mutations in ATP7B result in impaired biliary copper excretion with consecutive copper overload primarily in the liver and later in the brain causing hepatic and neuro-psychiatric symptoms. All available therapies aim to restore a negative copper balance. Their use—or the choice of the treatment—is driven by different safety and efficacy consideration as well as by the clinical presentation of the patient and previous exposure to anti-copper drugs. Current guidelines (5,6) discriminate treatment regimens as initial (decoppering) or long-term (maintenance) therapies. After the initial, more potent treatment phase aiming for a negative copper balance, a reduced dose of the chelating agents might be sufficient for maintenance of copper homeostasis.
D-penicillamine (DPA) was introduced as the first oral copper chelator by Walshe in 1956 (7) and saved thousands of WD patients worldwide. Alternative anti-copper drugs with in improved safety profile followed with zinc salts (ZS) in the 1960s (8) and with trientine (TETA) in the 1980s (9).
Medical needs
Concerning patient compliance, certain phenotypes can be described, divided in three with a divergent mortality and morbidity: “the incompliant patient, the patient with fulminant hepatic failure and the symptomatic neurologic patient” (10).
Once the diagnosis is made, lifelong treatment and monitoring of adherence is necessary. Non-compliance and as a consequence uncontrolled copper balance are main risk factors for hepatic failure or neurological deterioration (11). In the light of studies suggesting a high rate of patients with problematic long-term adherence (12), measures to prevent incompliance and to improve adherence are essential. Thus, the ideal treatment regime scheme should be as simple as possible (10) and efficacy of the current anti-copper regimen should be re-evaluated in any case of disease progression (5,6).
Overall, the efficacy of chelating agents and/or zinc is satisfactory for hepatic disease manifestations, except in patients developing acute liver failure (formerly referred to as “fulminant Wilson disease”) in whom still liver transplantation might be the only lifesaving therapy. Validated scores can guide the decision whether an urgent liver transplantation is needed or not (13,14).
Still disappointing results—in regard to treatment response—are seen in a large proportion of patients with neurological symptoms. The optimal treatment of neurologic disease is—in these authors opinion—the most pressing medical need in WD. For sure, the disappointing neurologic response can in part be explained by the irreversibility of structural neurologic damage. But still, paradoxical neurological deterioration after the initiation of chelation therapy is an unexplained unfavorable course.
Choice of drug for initial treatment
In WD only few randomized controlled trials and thus the available medical treatment options are still not standardized. Treatment recommendations are largely based on clinical experience and cohort studies and driven by safety concerns. The clinical presentation of the patient might drive treatment decisions according to the following rationales:
- In asymptomatic patients or patients with only mild hepatic symptoms all available agents have the desired effect (11,15-21). The choice of the drug—chelators versus ZS—should primarily be driven by safety considerations (10). Concerning chelating agents this favors TETA over DPA (22,23).
- In patients with hepatic manifestation, the degree of liver damage determines the further clinical course. From a hepatologist’s perspective a liver cirrhosis is a liver cirrhosis—and comes with all the implications regarding monitoring and treatment of portal hypertension that in any other liver patient with a different etiology. In WD, chelators establish a negative copper balance faster than ZS (21,24,25). We have previously reported a hepatic improvement with DPA or TETA in more than 90% of symptomatic hepatic cases (23).
- In case of symptomatic neurologic patients, therapy is less successful with at least a third of patients not profiting by medication (23). Clinical response rates to chelation therapy are in same ranges as reported for zinc monotherapy with regard to symptomatic neurologic patients (16,26). This fact could be explained by the concept of an irreversible cell damage in the central nervous system, which is already established at time of diagnosis (10,27). Most troublesome however is the reported paradoxical worsening of the neurological symptomology in up to 20% of WD patients after initiation therapy (16,28-30). In up to half of the patients showing such deterioration, the neurologic disease progression might be even irreversible (31). Several reports suggest that this worsening might be associated with chelating agents [especially DPA (30)], but it seems to occur under zinc as well (31).
An approach to address safety issues—especially with regard to prevention of neurologic deterioration—might be a careful and systematic monitoring of biochemical markers [e.g., non-ceruloplasmin-bound copper (NCC), urinary copper, etc.] as well as a continuous monitoring of clinical symptoms using validated rating scales such as the unified WD rating scale (UWDRS) (10).
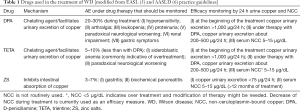
Available drugs for WD are listed in Table 1 [modified from (5) and (6)], that we will discuss drug by drug in the following paragraphs.
Full table
DPA
The major effect of DPA is to stimulate and extend the urinary excretion of copper. The recommended maintenance dose is 750–1,500 mg/day (20 mg/kg/day rounded off to the nearest available dose), administered in two or three divided doses (5).
DPA should be taken about one hour prior to meals, because gastrointestinal absorption is inhibited food. In case it is administered together with a meal, absorption can be decreased by about fifty percent (5). In addition, DPA interferes with pyridoxine metabolism why excess pyridoxine should be supplemented (25–50 mg/day).
Twenty-four-hour urinary copper excretion is recommended for treatment monitoring. Collection procedures vary among centers with some—especially European centers—supporting urinary copper excretion measurements after 2 days off chelating agents. However, especially in the initial treatment phase, urinary copper measurements on drug (without any interruption) might be more informative. Urinary copper per day is usually highest during initiation of treatment and should be three to eight µmol per twenty-four hours (equivalent to 200–500 µmol/24 h) (5). In long-term monitoring, the most important sign of efficacy are clinical and laboratory improvements. It is observed that serum ceruloplasmin may decrease after initiation of decoppering therapy.
Therapeutic efficiency is reached when urinary copper excretion reached a steady state, usually between 2–5 times upper limit of normal (UNL). This might correspond to measures less than 1.6 µmol per day after two days of chelator intermission. Additionally, NCC reveals normalization under effective treatment (32). Serum NCC under treatment should be 5–15 µg/dL (5,12,33).
DPA is rapidly absorbed from the gastrointestinal mucosa. The greatest amount of DPA is bound to plasma proteins such as albumin (about 80%). The free percentage of DPA becomes inactive by forming dimers or binds to other plasma proteins e.g., cysteine (6). Total bioavailability is estimated at 40–70%, depending also on correct administration (6). Major amount of DPA is discharged via the kidneys. The excretion half-life (t ½) of DPA is variating because of individual metabolism as well as of medication administration (t ½ =1.7–7 hours) (5,6).
The effectiveness of DPA as well tolerated treatment for WD has been proven in numerous clinical studies (16,30,34). In patients with symptomatic liver disease, recovery of liver function (quick, albumin, cholinesterase) and improvement in clinical signs (e.g., less fatigue) typically occurs during the first six to twelve months (5).
Nonadherence to therapy leads often to significant progression, inducing acute liver failure within few months. In symptomatic neurological patients, improvement of symptoms is observed to be slower and may be even awaited after some years (1–3 years) (5,35). Neurological deterioration is reported especially during initial phase of treatment in 10–30% of patients under DPA therapy (30).
When starting with gradual doses (between 150–300 mg/day) which can be increased slowly every week till the maximum dose is reached, tolerance can be exaggerated and undesirable side effects limited (5). Very fast dose escalations as well as re-administration after a longer therapy pause seem to be associated with potentially irreversible neurological deterioration (30,31).
DPA is associated with numerous side effects, which in approximately 30% of patients require discontinuation (34,36). These can be divided in early adverse events (AE) within the first three weeks and late AE’s, which might come up after years.
Early sensitivity reactions are marked by drug fever and cutaneous manifestations including generalized pruritus and rashes, lymphadenopathy or depression of blood cells (neutropenia, thrombocytopenia or total aplasia in case of bone marrow depression) (6). Even proteinuria might be detected by urinary status during the first weeks and is also recommended to be checked regularly under treatment as a monitoring instrument (5). Severe thrombocytopenia or total aplasia as well as newly diagnosed proteinuria require immediate discontinuation of DPA treatment (10). Mostly, this can be observed in cases of over dosing.
Late onset side effects include progressive proteinuria or the seldom Goodpasture syndrome with fatal glomerulonephritis and intra-alveolar haemorrhage. These findings of nephrotoxicity should lead to discontinuation of DPA (16). Other long-term reactions span from mild symptoms, such as gastric symptoms, hair loss or hypogeusia to myasthenia- or lupus-like syndrome marked by hematuria, positive antinuclear antibody (4,6).
Dermatological toxicities are reported more frequently, including structural changes in the skin. Elastosis perforans serpiginosa, pemphigus or pemphigoid like lesions, lichen planus or aphthous stomatitis are the most frequent ones to name (6,37).
DPA should not be combined with agents of the following classes because of pharmacological interactions: myelosuppressive or cytostatic agents, antimalarials, oxyphenbutazone and phenylbutazone (4). It interacts also with other (heavy) metals, why administration should be timely separated from zinc and iron uptake.
TETA
In 1969, TETA was introduced as an alternative to DPA. TETA is also a chelator but its chemically structure is distinct from DPA lacking sulfhydryl groups. Like DPA, TETA increases urinary copper excretion.
In contrast to DPA, TETA gastrointestinal absorption is less efficient (5). The absorbed drug is metabolized and inactivated in relevant amounts (6): directly, about one percent of the administered TETA and about eight percent of the biotransformed metabolite (acetyltrien) are excreted via urine (6).
In comparison with TETA, its metabolite (acetyltrien) binds copper less effective (6). The mobilized copper is like DPA discharged via the kidneys. The discussion of whether TETA is a weaker chelator of copper than DPA is still controversial in recent studies (6,16,38). Nevertheless, both agents seem to target different pools copper (6,38).
TETA is accepted as an alternative drug to DPA with potential, especially in patients that suffer from side effects of DPA or have clinical features indicating prospective intolerance (6,9,29). In contrast to DPA, neurological worsening under TETA initiation phase has been detected less common (6). Moreover, a hepatic improvement with TETA is reported in some studies in more than ninety percent of patients with hepatic symptoms (23).
Treatment monitoring is analog to DPA by measuring twenty-four hours urinary copper excretion without treatment pause (see reference values above). The NCC may show normalization under effective treatment. NCC is a good parameter of dosing and adherence. In patients with nonadherence to therapy, NCC is usually enhanced (reference values: 15 to 150 µg/dL) (6). If NCC values are very low (5 to 50 µg/L), this might indicate overdosing (6).
Recommended dosages of TETA are between 900–2,700 mg/day during treatment initiation and between 900–1,500 mg/day (20 mg/kg/day) used for maintenance (5,6). Like DPA, doses should be divided into several portions. Guidelines recommend to take TETA one hour before or several hours after meals. TETA needs to be cooled if the tablet is exposed to high temperatures, because the active agent is not heat-resistant (6).
TETA has a few side effects, AE are four-fold less than in DPA. Severe hypersensitivity reactions have not been reported yet, except a fixed cutaneous drug reaction which was observed in one patient (6). A reversible sideroblastic anemia may be a consequence of overtreatment and resultant copper deficiency. Pancytopenia has been observed in some cases. Lupus-like syndrome has also been reported in some patients as well as hemorrhagic gastritis, loss of taste and rashes (6,39).
Zinc
The pharmacological mechanism of zinc is different from DPA and TETA: zinc competes with the uptake of copper in the gastrointestinal mucosa. Zinc induces metallothionein—a cysteine-rich protein—in the enterocyte, which functions as an endogenous chelator of metals.
Metallothionein binds copper with greater affinity than zinc and thus, preferentially binds copper. This indirectly stops copper uptake to the blood circulation (26). The copper is somehow trapped in the enterocyte and excreted into the fecal contents by normal cell turnover (26). Zinc treatment can generate a negative balance for copper (40,41). Zinc may also induce elevated levels of hepatocellular metallothionein, enhancing cellular copper storage capacity (42,43). Different zinc salts for example sulphate, acetate or gluconate are available, but pharmacodynamics data favors zinc acetate (5). The recommended dose is a maximum of 150 mg elemental zinc per day divided in two to three dosages before food uptake, because its food interferes significantly with its with its absorption (5,6,44).
In combination therapy with chelators different times of dosing have to be considered to avoid interaction (see paragraph TETA above).
Monitoring of treatment with zinc is follows clinical and biochemical improvement. Like monitoring of DPA or TETA, twenty-four hours urinary excretion of copper can be used. Values should be less than 1.6 µmol per day on stable treatment (<75 µg/24 h) (5,6). Additionally, NCC should drop with effective treatment >12 months (NCC 5–15 µg/dL). Urinary zinc amount can be occasionally quantified to check patient’s adherence (5).
Zinc has some side effects. Gastric irritation is common in about 30% of patients (5). Zinc may have immunosuppressant effects by reducing leukocytes and causing a bone marrow depression (8,40). Increased serum lipase/amylase might be measured, without any—clinical or radiologic—sign of pancreatitis (5,41). Neurological deterioration is not reported under zinc monotherapy (6,16,45).
Nevertheless, zinc as monotherapy during initial decoppering phase might be not as effective as a therapy with chelating agents (22), but seems to be equal for therapy maintenance. Moreover, it is recommended as first-line therapy for asymptomatic patients, better tolerated as e.g., DPA (5,6,41). While zinc monotherapy is safe in neurological and in asymptomatic patients, hepatic deterioration is reported in some cases of patients with hepatic manifestation (5,45). In a subpopulation of patients, zinc monotherapy is insufficient to control hepatic disease (46,47).
In summary, exclusive monotherapy with zinc in symptomatic Wilson liver disease requires monitoring for efficacy as well as for possible side effects.
Treatment sequences and maintenance therapy: consequences for long term monitoring
The overall goal of treatment monitoring is to ensure clinical and biochemical improvement, assess compliance and screen for AE necessitating modifications of the medical regime.
This includes the assessment of when the patients leave the decoppering phase and enter into maintenance therapy. In clinical practice this time point if surprisingly unclear, as there are no commonly accepted definitions of when a patient is “de-coppered”.
From a biochemical point of view for a copper overload disorder, a response guide therapy seems a logical consequence, taking into account the treatment related changes of measurable copper parameters (48,49). An analysis daily urinary copper excretion (under ongoing medication) reflects overall exchangeable copper and is helpful for monitoring as well as for compliance. Target ranges of 24-hour urinary copper excretion under DPA, TETA and zinc are already mentioned above. If values for urine copper are elevated, this might be indicative of poor adherence or underdosing. Low values for urine copper excretion under chelation treatment could also indicate overtreatment while NCC values are typically low (33).
Non-ceruloplasmin-bound copper (or “free copper”) can be calculated by subtracting ceruloplasmin-bound copper from the total serum copper concentration: NCC = [total serum copper (µmol/L) −0.049] × ceruloplasmin (mg/L) (5). The amount of copper associated with ceruloplasmin is approximately 3.15 µg of copper per milligram of ceruloplasmin. The usefulness of this calculation in WD has been subject of intensive discussions in the field. The value of ceruloplasmin levels determined by immunological methods has been questioned due to the high values measuring falsely high Cp values, as these tests do not discriminate between holo-ceruloplasmin and apo- ceruloplasmin (50,51). When using immunological tests, negative NCC values for NCC might be found up to 10 to 25% of WD patients (52-54). NCC is elevated above 25 µg/dL (250 µg/L) in most untreated patients (normal 15 µg/dL =150 µg/L) and should decline under anti-copper-therapy. NCC concentrations <5 µg/dL (<50 µg/L) could be a signal of systemic copper depletion which is possible in patients a prolonged treatment.
Long-term intake of subtherapeutic dosages may also present with low values for 24-hour urine copper excretion, while having elevated NCC values. Urine analysis as well as total blood count should be performed regularly to assure safety under chelation therapy to detect adverse proteinuria or anemia (33).
Conclusions
Improved diagnostic techniques and more systematic approaches in diagnosis offer an easier path to confirmation or exclusion of a diagnosis of WD and therefore an earlier treatment. Currently used ZS and chelators are mostly effective but have some limitations, chelating agents being associated with a deterioration of neurological symptoms. Future clinical trials should aim for better defining dosing, ideally offering comparative effectiveness of available medical therapies and standardization of definitions for treatment success and failure. The concept of different copper pools renders “control of free circulating copper” a primary monitoring readout. However, broad clinical evidence is lacking to allow general recommendation for dosage adjustments based on the Serum copper status alone. Currently NCC, urinary copper excretion as well as for other biochemical markers can only be seen as broad guidance, but not as read out parameters of a response guided therapy. All biochemical parameters (liver function) and clinical features (course of neurologic symptoms) should be taken into account regarding dosage decisions.
Acknowledgements
None.
Footnote
Conflicts of Interest: KH Weiss advises or received grant support from for GMP-O, Univar, Vivet therapeutics, Alexion. I Mohr has no conflicts of interest to declare.
References
- Walshe JM. History of Wilson's disease: 1912 to 2000. Mov Disord 2006;21:142-7. [Crossref] [PubMed]
- Walshe JM. History of Wilson disease: a personal account. Handb Clin Neurol 2017;142:1-5. [Crossref] [PubMed]
- Bandmann O, Weiss KH, Kaler SG. Wilson’s disease and other neurological copper disorders. Lancet Neurol 2015;14:103-13. [Crossref] [PubMed]
- Członkowska A, Litwin T, Dusek P, et al. Wilson disease. Nat Rev Dis Primers 2018;4:21. [Crossref] [PubMed]
- European Association for Study of L. EASL Clinical Practice Guidelines. Wilson’s disease. J Hepatol 2012;56:671-85. [PubMed]
- Roberts EA, Schilsky ML. American Association for Study of Liver D. Diagnosis and treatment of Wilson disease: an update. Hepatology 2008;47:2089-111. [Crossref] [PubMed]
- Walshe JM. Wilson’s disease; new oral therapy. Lancet 1956;270:25-6. [Crossref] [PubMed]
- Hoogenraad TU, Van Hattum J, Van den Hamer CJ. Management of Wilson's disease with zinc sulphate. Experience in a series of 27 patients. J Neurol Sci 1987;77:137-46. [Crossref] [PubMed]
- Walshe JM. Treatment of Wilson's disease with trientine (triethylene tetramine) dihydrochloride. Lancet 1982;1:643-7. [Crossref] [PubMed]
- Weiss KH, Stremmel W. Clinical considerations for an effective medical therapy in Wilson's disease. Ann N Y Acad Sci 2014;1315:81-5. [Crossref] [PubMed]
- Dzieżyc K, Karlinski M, Litwin T, et al. Compliant treatment with anti-copper agents prevents clinically overt Wilson's disease in pre-symptomatic patients. Eur J Neurol 2014;21:332-7. [PubMed]
- Masełbas W, Chabik G, Czlonkowska A. Persistence with treatment in patients with Wilson disease. Neurol Neurochir Pol 2010;44:260-3. [Crossref] [PubMed]
- Nazer H, Ede RJ, Mowat AP, et al. Wilson's disease: clinical presentation and use of prognostic index. Gut 1986;27:1377-81. [Crossref] [PubMed]
- Dhawan A, Taylor RM, Cheeseman P, et al. Wilson’s disease in children: 37-year experience and revised King's score for liver transplantation. Liver Transpl 2005;11:441-8. [Crossref] [PubMed]
- Merle U, Schaefer M, Ferenci P, et al. Clinical presentation, diagnosis and long-term outcome of Wilson's disease: a cohort study. Gut 2007;56:115-20. [Crossref] [PubMed]
- Czlonkowska A, Gajda J, Rodo M. Effects of long-term treatment in Wilson's disease with D-penicillamine and zinc sulphate. J Neurol 1996;243:269-73. [Crossref] [PubMed]
- Bruha R, Marecek Z, Pospisilova L, et al. Long-term follow-up of Wilson disease: natural history, treatment, mutations analysis and phenotypic correlation. Liver Int 2011;31:83-91. [Crossref] [PubMed]
- Beinhardt S, Leiss W, Stattermayer AF, et al. Long-term Outcomes of Patients With Wilson Disease in a Large Austrian Cohort. Clin Gastroenterol Hepatol 2014;12:683-9. [Crossref] [PubMed]
- Arnon R, Calderon JF, Schilsky M, et al. Wilson disease in children: serum aminotransferases and urinary copper on triethylene tetramine dihydrochloride (trientine) treatment. J Pediatr Gastroenterol Nutr 2007;44:596-602. [Crossref] [PubMed]
- Linn FH, Houwen RH, van Hattum J, et al. Long-term exclusive zinc monotherapy in symptomatic Wilson disease: experience in 17 patients. Hepatology 2009;50:1442-52. [Crossref] [PubMed]
- Brewer GJ, Hill G, Prasad A, et al. The treatment of Wilson’s disease with zinc. IV. Efficacy monitoring using urine and plasma copper. Proc Soc Exp Biol Med 1987;184:446-55. [Crossref] [PubMed]
- Weiss KH, Gotthardt DN, Klemm D, et al. Zinc monotherapy is not as effective as chelating agents in treatment of Wilson disease. Gastroenterology 2011;140:1189-98.e1. [Crossref] [PubMed]
- Weiss KH, Thurik F, Gotthardt DN, et al. Efficacy and safety of oral chelators in treatment of patients with Wilson disease. Clin Gastroenterol Hepatol 2013;11:1028-35.e1-2.
- Brewer GJ, Yuzbasiyan-Gurkan V, Johnson V, et al. Treatment of Wilson's disease with zinc XII: dose regimen requirements. Am J Med Sci 1993;305:199-202. [Crossref] [PubMed]
- Hill GM, Brewer GJ, Juni JE, et al. Treatment of Wilson's disease with zinc. II. Validation of oral 64copper with copper balance. Am J Med Sci 1986;292:344-9. [Crossref] [PubMed]
- Brewer GJ, Dick RD, Johnson VD, et al. Treatment of Wilson's disease with zinc: XV long-term follow-up studies. J Lab Clin Med 1998;132:264-78. [Crossref] [PubMed]
- Hölscher S, Leinweber B, Hefter H, et al. Evaluation of the symptomatic treatment of residual neurological symptoms in Wilson disease. Eur Neurol 2010;64:83-7. [Crossref] [PubMed]
- Brewer GJ, Askari F, Lorincz MT, et al. Treatment of Wilson disease with ammonium tetrathiomolybdate: IV. Comparison of tetrathiomolybdate and trientine in a double-blind study of treatment of the neurologic presentation of Wilson disease. Arch Neurol 2006;63:521-7. [Crossref] [PubMed]
- Scheinberg IH, Jaffe ME, Sternlieb I. The use of trientine in preventing the effects of interrupting penicillamine therapy in Wilson’s disease. N Engl J Med 1987;317:209-13. [Crossref] [PubMed]
- Brewer GJ, Terry CA, Aisen AM, et al. Worsening of neurologic syndrome in patients with Wilson’s disease with initial penicillamine therapy. Arch Neurol 1987;44:490-3. [Crossref] [PubMed]
- Litwin T, Dziezyc K, Karlinski M, et al. Early neurological worsening in patients with Wilson's disease. J Neurol Sci 2015;355:162-7. [Crossref] [PubMed]
- Brewer GJ, Yuzbasiyan-Gurkan V, Lee DY, et al. Treatment of Wilson’s disease with zinc. VI. Initial treatment studies. J Lab Clin Med 1989;114:633-8. [PubMed]
- Poujois A, Woimant F. Wilson’s disease: A 2017 update. Clin Res Hepatol Gastroenterol 2018;42:512-20. [Crossref] [PubMed]
- Walshe JM. Copper chelation in patients with Wilson's disease. A comparison of penicillamine and triethylene tetramine dihydrochloride. Q J Med 1973;42:441-52. [PubMed]
- Członkowska A, Litwin T, Dziezyc K, et al. Characteristics of a newly diagnosed Polish cohort of patients with neurological manifestations of Wilson disease evaluated with the Unified Wilson's Disease Rating Scale. BMC Neurol 2018;18:34. [Crossref] [PubMed]
- Medici V, Trevisan CP, D'Inca R, et al. Diagnosis and management of Wilson’s disease: results of a single center experience. J Clin Gastroenterol 2006;40:936-41. [Crossref] [PubMed]
- Bécuwe C, Dalle S, Ronger-Savle S, et al. Elastosis perforans serpiginosa associated with pseudo-pseudoxanthoma elasticum during treatment of Wilson’s disease with penicillamine. Dermatology 2005;210:60-3. [Crossref] [PubMed]
- Sarkar B, Sass-Kortsak A, Clarke R, et al. A comparative study of in vitro and in vivo interaction of D-penicillamine and triethylenetetramine with copper. Proc R Soc Med 1977;70 Suppl 3:13-8. [PubMed]
- Epstein O, Sherlock S. Triethylene tetramine dihydrochloride toxicity in primary biliary cirrhosis. Gastroenterology 1980;78:1442-5. [PubMed]
- Brewer GJ, Hill GM, Prasad AS, et al. Oral zinc therapy for Wilson's disease. Ann Intern Med 1983;99:314-9. [Crossref] [PubMed]
- Hoogenraad TU. Zinc treatment of Wilson’s disease. J Lab Clin Med 1998;132:240-1. [Crossref] [PubMed]
- Schilsky ML, Blank RR, Czaja MJ, et al. Hepatocellular copper toxicity and its attenuation by zinc. J Clin Invest 1989;84:1562-8. [Crossref] [PubMed]
- Cousins RJ. Absorption, transport, and hepatic metabolism of copper and zinc: special reference to metallothionein and ceruloplasmin. Physiol Rev 1985;65:238-309. [Crossref] [PubMed]
- Pécoud A, Donzel P, Schelling JL. Effect of foodstuffs on the absorption of zinc sulfate. Clin Pharmacol Ther 1975;17:469-74. [Crossref] [PubMed]
- Walshe JM, Munro NA. Zinc-induced deterioration in Wilson's disease aborted by treatment with penicillamine, dimercaprol, and a novel zero copper diet. Arch Neurol 1995;52:10-1. [Crossref] [PubMed]
- Steindl P, Ferenci P, Dienes HP, et al. Wilson’s disease in patients presenting with liver disease: a diagnostic challenge. Gastroenterology 1997;113:212-8. [Crossref] [PubMed]
- Członkowska A, Gromadzka G, Buttner J, et al. Clinical features of hemolysis, elevated liver enzymes, and low platelet count syndrome in undiagnosed Wilson disease: report of two cases. Arch Gynecol Obstet 2010;281:129-34. [Crossref] [PubMed]
- Weiss KH, Stremmel W. Evolving perspectives in Wilson disease: diagnosis, treatment and monitoring. Curr Gastroenterol Rep 2012;14:1-7. [Crossref] [PubMed]
- Weiss KH, Stremmel W. Clinical considerations for an effective medical therapy in Wilson's disease. Ann N Y Acad Sci 2014;1315:81-5. [Crossref] [PubMed]
- Twomey PJ, Viljoen A, Reynolds TM, et al. Non-ceruloplasmin-bound copper in routine clinical practice in different laboratories. J Trace Elem Med Biol 2008;22:50-3. [Crossref] [PubMed]
- Poujois A, Trocello JM, Djebrani-Oussedik N, et al. Exchangeable copper: a reflection of the neurological severity in Wilson's disease. Eur J Neurol 2017;24:154-60. [Crossref] [PubMed]
- Twomey PJ, Viljoen A, House IM, et al. Relationship between serum copper, ceruloplasmin, and non-ceruloplasmin-bound copper in routine clinical practice. Clin Chem 2005;51:1558-9. [Crossref] [PubMed]
- Gnanou JV, Thykadavil VG, Thuppil V. Pros and cons of immunochemical and enzymatic method in the diagnosis of Wilson's disease. Indian J Med Sci 2006;60:371-5. [Crossref] [PubMed]
- McMillin GA, Travis JJ, Hunt JW. Direct measurement of free copper in serum or plasma ultrafiltrate. Am J Clin Pathol 2009;131:160-5. [Crossref] [PubMed]


