Complete percutaneous laparoscopic cholecystectomy by employing the Percuvance Percutaneous Surgical System
Introduction
Laparoscopic cholecystectomy (LC) is currently, the gold standard in the treatment of gall bladder diseases. In the view of minimizing tissue trauma, wound complications, postoperative scarring, as well as improving cosmesis, minimally invasive surgery advances. Several novel techniques have been described as modifications of the standard procedure (1). Natural orifice transluminal endoscopic cholecystectomy, single incision LC and needlescopic cholecystectomy are some aspects (2).
Needlescopic surgery or mini-laparoscopy refers to the procedure which employs instruments of 3 mm in diameter or less (3). The aim of this paper is to document the first cases of complete needlescopic cholecystectomy with the Percuvance Percutaneous Surgical System (Teleflex, Wayne, PA, USA).
Methods
The study was approved by the Investigational Review Board of Aristotle University of Thessaloniki (IRB approval 30/2018). The revised declaration of Helsinki was applied. The exclusion criteria included the contraindications of laparoscopy.
From December 2016 to March 2018, fifteen patients consented to undergo LC using the Percuvance system. Patients were pre-operatively evaluated. Selection criteria included a normal body mass index (BMI) (18.5 to 24.9) or slight overweight (25 to 29.9), who reported no previous upper abdominal operations. The indications of cholecystectomy remain the same as the conventional. However, we choose patients that experienced mild galdbladder disease.
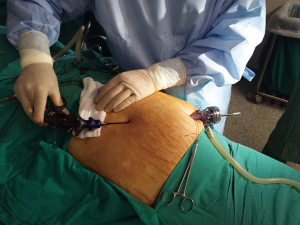
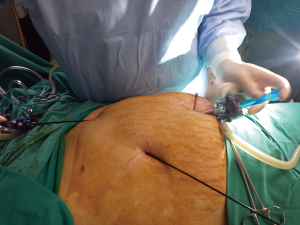
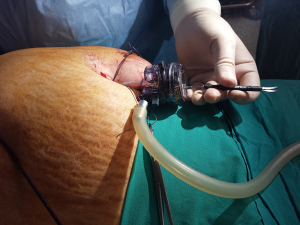
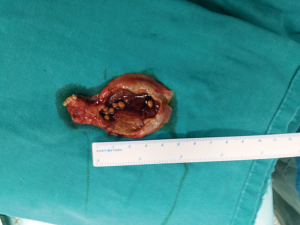
All procedures were performed by the same experienced surgeon. Entry into the abdomen was achieved under direct visualization. A 10 mm Hassontrocar was placed and pneumoperitoneum was created. The rest of the instruments of the Percuvance system were positioned. A small incision of the skin was performed at the level of the midline just below the xiphoid and a 2.9-mm disposable shaft with reusable, interchangeable effectors and a reusable handle was inserted into the abdomen under direct visualization with a Veress needle tip. The end was extra-corporealized through the 10 mm umbilical camera port. The introducer tip was unlocked and a 5 mm dissector tool was inserted. The same procedure was followed for the second shaft that was placed in the lateral right abdomen position and changed with an atraumatic grasper tip. This was applied to the fundus of the gallbladder to create enough traction so as to enable the visualization of Callots triangle. The instrument tips were exchanged with other tips (e.g., scissors, dissector) during cholecystectomy as many times as necessary, repeating the step of extra corporatization. The next steps are the same as the conventional LC. The gallbladder was retrieved through the 10 mm umbilical port.
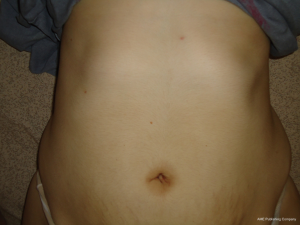
After procedures’ completion, the fascia was closed with 0-polyglactin 910 (VicrylTM), while the skin of the umbilicus was left to heal. The percutaneous access sites were closed with Steri-StripsTM only (Figures 1-7).
Patients were discharged after achieving adequate pain control management. All of them were followed-up 1 week and 3 months postoperatively (Figures 8-10). Data were collected prospectively.
Results
Patients characteristics are summarized in Table 1. Ten females and 5 males, with mean age of 42.44 years were included. Mean BMI was 24.2 kg/m2. None of them reported a previous surgical history. ASA score was under 2. Mean operative time was 74.5±18.3 minutes and hospital stay was 1 day. No drainages were inserted and no additional trocars were introduced in the surgical field in 14 PLC. None of the PLC was converted to open cholecystectomy However, a conversion to convention all laparoscopic cholocystectomy was recorded in order to control bleeding and to place a drainage. For the rest of the cases and when needed, a suction pipe was placed parallel to the umbilical trocar so as to avoid the insertion of another trocar. Postoperatively, no wound-related complications were observed while scarring was minimal.
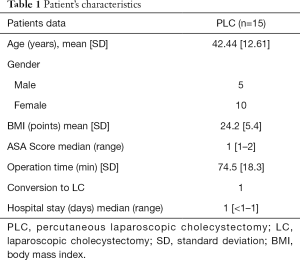
Full table
Discussion
Recent trends tend to develop the most minimally invasive approach for cholecystectomy. Needlescopic instruments and techniques seem to represent a promising candidate for several laparoscopic surgeries, including cholecystectomy, appendectomy, Nissen fundoplication, and video-assisted thoracoscopic surgery (2,4).
In general, the smaller the size of laparoscopic instruments the fewer the port-related injury occurs (4). As a consequence, activation of the sympathetic nervous is decreased system and so, less postoperative analgesic medication is required (5). Furthermore, wound infection rates are lower, decreasing the risk of future herniation and improving cosmesis (4,5). Kimura et al. (6) reported that the scars become significantly smaller as the size of the trocar decreases, not only immediately after the operation but also at 6-month follow-up. In this report, patients were evaluated postoperatively. On years interval scars seemed to be minimal.
However, flaws exist and may prolong the operation time (3), increase the risk of perioperative complications, or impose stress on surgeons (4). These results from the small size of the instruments and laparoscopes (7). Several of the available instruments reach the length of 2.9 cm or less, while instrument tips are smaller compared with 5-mm instruments, which can complicate dissection, especially in cases of inflammation. Such instruments bend easily and are prone to mishandling (2,5). As far as the 3-mm laparoscopes is concerned, they seem to have restricted visual field, poor resolution, and clarity (4). In our study, this was out reached by the placement of a 10-mm Hasson trocar, while extra-corporealizing the 2.9-mm shafts through a separate 10-mm trocar, without the loss of pneumoperitoneum, was technically simple. Fluency can, obviously, be achieved when completing the learning curve. Careful preoperative evaluation should be highlighted, while the choice of conversion remains the solution when the procedure is complicated.
Percutaneous LC with the Percuvance System seems to be a viable option in the era of minimally laparoscopic procedures.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study was approved by the Investigational Review Board of Aristotle University of Thessaloniki (IRB approval 30/2018).
References
- Rossitto C, Gueli Alletti S, Costantini B, et al. Total Laparoscopic Hysterectomy With Percutaneous (Percuvance) Instruments: New Frontier of Minimally Invasive Gynecological Surgery. J Minim Invasive Gynecol 2016;23:14-5. [Crossref] [PubMed]
- Krpata DM, Ponsky TA. Needlescopic surgery: what's in the toolbox? Surg Endosc 2013;27:1040-4. [Crossref] [PubMed]
- Gagner M, Garcia-Ruiz A. Technical aspects of minimally invasive abdominal surgery performed with needlescopic instruments. Surg Laparosc Endosc 1998;8:171-9. [Crossref] [PubMed]
- Tagaya N, Kubota K. Reevaluation of needlescopic surgery. Surg Endosc 2012;26:137-43. [Crossref] [PubMed]
- Chang J, Boules M, Rodriguez J, et al. Minilaparoscopy with Interchangeable, Full 5-mm End Effectors: First Human Use of a New Minimally Invasive Operating Platform. J Laparoendosc Adv Surg Tech A 2016;26:1-5. [Crossref] [PubMed]
- Kimura T, Yamauchi K, Ihara Y, et al. Single-site laparoscopic herniorrhaphy using needle instruments for inguinal hernias in children: a novel technique. Surg Today 2012;42:100-3. [Crossref] [PubMed]
- Markar SR, Karthikesalingam A, Thrumurthy S, et al. Single-incision laparoscopic surgery (SILS) vs. conventional multiport cholecystectomy: systematic review and meta-analysis. Surg Endosc 2012;26:1205-13. [Crossref] [PubMed]