
Successful treatment of complex coronary chronic total occlusions improves midterm outcomes
Introduction
Chronic coronary total occlusions (CTOs) are found in 15–25% of all patients referred for coronary angiography (1). Although percutaneous coronary intervention (PCI) is one of the more common treatment options for patients with coronary CTOs, the clinical benefits of CTO PCI have remained controversial given the conflicting findings from several studies. For instance, a newly-published European randomized controlled trial (RCT) showed that at 12-month follow-up, CTO recanalization led to a significant improvement of health status in patients with stable angina (2). Additionally, several large observational studies that compared the outcomes of CTO PCI with no revascularization suggested both the short-term and long-term survival benefit of successful PCI in CTO (3-10).
In contrast, there is evidence from several studies which challenges the consensus that CTO PCI is unconditionally advantageous. One recent example of this is a large RCT presented at the 2017 American College of Cardiology (ACC) meeting (11), which demonstrated CTO PCI plus optimal medical therapy (OMT) was not superior to OMT alone in reducing cardiovascular outcomes at 3-year follow-up. Similarly, a Dutch RCT involving patients with ST-elevation myocardial infarction (STEMI) with a concurrent CTO showed that CTO PCI was not associated with a reduction in long-term major adverse cardiac events (MACE) compared to CTO-No PCI (12). Furthermore, in a few observational studies, CTO PCI was not associated with reduction in mortality (13,14). However, it is essential to account for the discrepancy among included studies in regards to differences in patient population, different CTO grading, and various PCI approaches. Unfortunately, data detailing outcomes of PCI in patients with different difficulty grading lesions is limited. Therefore, we aimed to conduct a prospective study in order to evaluate clinical outcomes in patients with J-CTO (Multicenter CTO Registry in Japan) score ≥3 after CTO PCI.
Methods
Study population
A total of 145 consecutive patients treated with PCI were enrolled in our center from August 2016 to March 2017 for at least 1 CTO. Eligible patients were those who were at least 18 years of age and met the indication for PCI of CTO, which was based on the presence of anginal symptoms and/or evidence of reversible myocardial ischemia on perfusion imaging or on stress testing. Patients were not enrolled if they were more than 85 years of age, because such patients are at higher risk due to multiple comorbidities. Patients were also not enrolled if they met any exclusion criteria for implantation of drug-eluting stents (DES) (e.g., patients with severe hemorrhagic diseases or patients who cannot be on dual antiplatelet therapy). Baseline demographic, clinical, angiographic, and procedural data, along with in-hospital outcome data of the enrolled patients were entered into our clinical database. Patient follow-up was performed either by a clinical visit or by a telephone interview at 1 year after PCI. All information was collected by physicians through the revision of clinical source documentation. The study was performed in accordance with the Declaration of Helsinki, approved by the relevant authorities, and all patients provided written informed consent.
Definitions and study endpoints
Coronary CTOs were defined as angiographic evidence of total occlusions with Thrombolysis in Myocardial Infarction (TIMI) flow grade 0 and an estimated duration of at least 3 months (15). The estimates for the duration of occlusion were clinically based on the onset of symptoms or timing of myocardial infarction (MI) in the CTO related artery. The complexity of CTO lesion was assessed by J-CTO score (0= easy, 1= intermediate, 2= difficult, ≥3= very difficult) (16). Success of CTO PCI was defined as angiographic success (final residual stenosis <20% by visual estimation and TIMI flow grade 3 after CTO recanalization). Coronary perforation, collateral perforation, concurrent pericardial tamponade and stent thrombosis (ST) were recorded as procedural complications. In-hospital events were considered as death, periprocedural MI, urgent target vessel revascularization (TVR) [including coronary artery bypass grafting (CABG) or re-PCI] and proven periprocedural cerebrovascular events. At follow-up, MACE was defined as the composite of death from any cause, non-fatal MI, and need of TVR. Criteria for MI were taken from the Fourth Edition of the Universal Definition of Myocardial Infarction (17). ST was defined according to the Academic Research Council criteria (18). The primary endpoint was the frequency of MACE at 12 months. The secondary endpoint was rehospitalization for cardiovascular reasons (angina aggravation or heart failure).
PCI procedures
All patients received optimal dual antiplatelet therapy before and after PCI according to operators’ preference. Patients received an initial bolus of intravenous unfractioned heparin (150 IU/kg). The activated clotting time (ACT) was monitored every 30 minutes to determine if an additional bolus of unfractioned heparin was necessary to maintain an ACT of >300 seconds. J-CTO score incorporates 5 baseline clinical and angiographic CTO parameters into a 5-point scoring system to assess the difficulty of CTO crossing. One point is given for each of the following factors that were associated with a lower probability of successful guide wire crossing within 30 minutes: blunt stump, calcification, within lesion bending >45°, occlusion length ≥20 mm, and prior failed attempt to revascularize the CTO (8). Choice of CTO revascularization strategy via the anterograde or the retrograde approach, choice of guidewires, microcatheters, and CTO crossing equipment and techniques were at the discretion of the individual operators. Several guidewire techniques were used, including the parallel-wires technique, the intravascular ultrasound–guided wiring technique, subintimal tracking and re-entry (STAR) technique, and variations of retrograde wiring through collateral vessels, such as kissing wires, the knuckle technique, and the reverse controlled anterograde retrograde tracking (CART) techniques. Only newer-generation DES were implanted (everolimus or zotarolimus). In case of PCI failure, medical therapy was chosen according to the clinical need.
Statistical analysis
Clinical characteristics, angiographic features, and in-hospital and follow-up events were reported through standard descriptive analyses for large samples and were assumed to follow a normal distribution. Discrete variables were reported as counts (percentages) and continuous variables as mean ± SD. For discrete variables, depending on which test was appropriate, we tested differences between groups with either the χ2 test or the Fisher’s exact test. We used the two-tailed t-test to compare continuous variables. We assessed the difference in the incidence of MACE between the strata defined by success/failure of CTO and by J-CTO score <3 vs. J-CTO score ≥3, based on the log-rank statistic and a significance level of P=0.05. Cumulative MACE-free rates were calculated and graphically described according to the Kaplan-Meier method. We derived hazard ratios (HRs) with associated 95% confidence intervals (CIs) from the multivariable Cox proportional hazards model to determine the independent predictors of midterm MACE occurrence. Given the number of events available, variables for inclusion were carefully chosen to ensure parsimony of the final model. Baseline variables with P values <0.20 on univariate analysis or, that were judged to be of clinical importance from previous published research despite P values >0.20, were entered into the model. Two-tailed P values <0.05 were considered to indicate statistically significant differences for all analyses performed. All statistical analyses were performed using the SPSS software package, version 20.0 (SPSS Inc., Chicago, IL, USA).
Results
Baseline clinical and angiographic characteristics
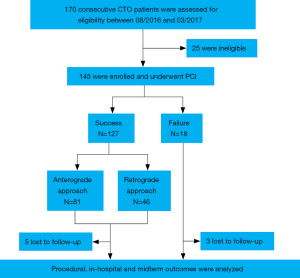
Between August 2016 and March 2017, a total of 170 consecutive patients at our center were screened, of whom 25 were excluded due to refusal for enrollment. A total of 145 patients fulfilled the inclusion criteria and underwent CTO PCI (Figure 1). Overall, the mean age was 61.9±9.6 years, and 91% were males. All baseline patient clinical characteristics (Table 1), organized according to procedural success or failure of PCI, were similar between the two groups. Baseline lesion characteristics are described in Table 1. Most CTOs were in the right coronary artery (54.5%), followed by the left anterior descending (28.3%) and circumflex arteries (15.9%). Lesion characteristics were similar between the groups except for a higher proportion of bending >45°, blunt proximal cap, and J-CTO score ≥3 lesions in the failure CTO PCI group. Furthermore, J-CTO scores were statistically higher in patients with failed CTO PCI (3.67±0.77 vs. 2.87±1.19; P=0.006).

Full table
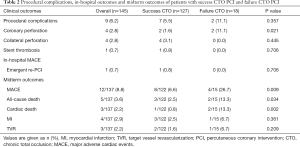
Procedural complications and in-hospital outcomes
Successful PCI of CTO was achieved in 127 (87.6%) patients. Table 2 reports procedural complications and in-hospital outcomes of patients with successful CTO PCI and failure CTO PCI. Overall, procedural complications occurred in 9 (6.2%) patients. Coronary perforation was significantly more common after failed recanalization of CTO than after successful recanalization (P=0.021). In-hospital events were infrequent in the CTO cohort. One patient who underwent successful PCI of a right coronary artery CTO developed ST-segment elevation MI the following day, and underwent an urgent PCI with favorable outcome. The retrograde approach was applied in 36.2% of successful procedures. All complications were managed in a timely manner, without periprocedural death.
Full table
Clinical events during 12 months
Among the study population, data on midterm follow-up were available in 137 patients (94.5%). Eight patients dropped-out at 6 months due to a loss of contact (phone number expired). The mean clinical follow-up period was 11.49±2.01 months. Overall, MACEs occurred in 12 patients (8.8%) (Table 2). During follow-up, 5 (3.6%) patients died; of these, 3, 1, and 1 patient died of cardiovascular cause, lung cancer, and traffic accident, respectively. The rate of further revascularization, either percutaneously or surgically, was 2.2%. In comparison with patients with failed CTO PCI, successfully revascularized patients showed lower rates of all-cause death (13.3% vs. 2.5%, respectively; P=0.034) and overall MACEs (26.7% vs. 6.6%, respectively; P=0.009) (Table 2). Furthermore, successful revascularization was associated with a significantly lower 1-year mortality rate than failed revascularization (HR: 0.485; 95% CI: 0.003–0.817; P=0.0357) (Figure 2A).
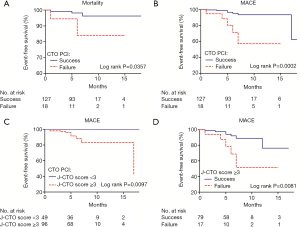
Recanalization and clinical outcomes
Successful revascularization was associated with a significantly lower 1-year MACE rate than failed revascularization (HR: 0.026; 95% CI: 0.004–0.176; P=0.0002) (Figure 2B).
J-CTO score and clinical outcomes
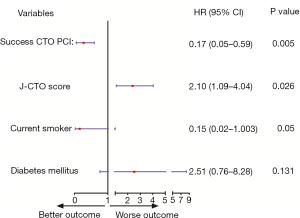
J-CTO score ≥3 was associated with a significantly higher 1-year MACE rate than J-CTO score <3 in patients undergoing PCI (HR: 4.819; 95% CI: 1.463–15.870, P=0.0097) (Figure 2C). Moreover, in patients with J-CTO score ≥3, success of CTO PCI was associated with a significantly lower 1-year MACE rate than failure of CTO PCI (HR: 0.114; 95% CI: 0.023–0.569; P=0.0081) (Figure 2D). Figure 3 summarizes the outcomes after adjustment for possible clinical confounders using the multivariate Cox regression model, which included the following clinical and angiographic variables: current smoker, diabetes mellitus, J-CTO score, and successful CTO PCI. This regression model identified J-CTO score (HR: 2.10; 95% CI: 1.09–4.04; P=0.026) and success of CTO PCI (HR: 0.17; 95% CI: 0.05–0.59; P=0.005) as significant independent predictors of MACEs.
Discussion
The main findings of the study
- Higher J-CTO score was independently associated with worse clinical outcomes in patients with CTOs;
- Successful recanalization of CTOs was associated with a reduction in midterm MACEs when compared to failed recanalization attempts;
- High procedural success and low complication rates of CTO PCI were observed among the dedicated CTO operators in our center.
Outcomes after CTO recanalization
We found a statistically significant MACE-free benefit of successful CTO PCI in comparison with unsuccessful recanalization of CTOs at 1-year follow-up. Our findings are consistent with several studies suggesting that successful CTO PCIs are associated with better outcomes than failed CTO revascularization procedures (3,4,7,19). Tomasello et al. (3) showed, using a cohort of 1,777 consecutive patients from the Italian CTO Registry, that successful CTO revascularization may significantly improve the survival and decrease MACE occurrence at 1-year follow-up. In agreement with our findings, Jang et al. (7) reported that CTO revascularization may reduce the risk of cardiac mortality and MACE during a median follow-up duration of 42 months. Furthermore, a meta-analysis of 25 observational studies, over a mean follow-up of 3 years, found that compared with unsuccessful CTO PCI, successful CTO PCI was associated with a lower risk of death [odds ratio (OR): 0.52; 95% CI: 0.43–0.63] (20), although no RCT was included in this meta-analysis. One interpretation of this result is that the higher complication rates related to CTO failure may lead to increase in major adverse events. Mortality advantage was also reflected in our study showing lower death rates in successful CTO when compared to failed CTO intervention (HR: 0.05; 95% CI: 0.003–0.82; P=0.0325).
Based on results from a small cohort of patients undergoing PCI in our center, our study adds weight to the growing body of evidence indicating that successful CTO PCI improves midterm clinical benefit. Nevertheless, two prior registries are not consistent with this view (14,21). Both the Korean multicenter registry (14) and the CREDO-Kyoto registry from Japan (21) suggested that successful CTO PCI was not associated with a lower risk of long-term MACEs but associated rather with significantly lesser risk of subsequent CABG. We speculate that this discrepancy with our study may be explained by differences in the rate of revascularization. To elaborate, in the study by Lee et al. (14) and Yamamoto et al. (21), the rates of TVR were 20.9% and 19.6%, respectively, after failed PCI of CTO. As a result, there were higher rates of TVR in CTO PCI failure, than in our study (3.7%). Subsequent TVR in patients with unsuccessful CTO PCIs might have mitigated the detrimental effects of failed recanalization of CTOs, but less so in our current study. Furthermore, the differences in mortality rates may be related to the selection of patients for CTO PCI. Also, the success rate of CTO PCI was 78% in the study by Yamamoto et al. (21), which was slightly higher in our study (86.8%). Notably, 46.1% received first-generation DES and 53.9% received newer-generation DES between March 2003 and May 2014 in the study by Lee et al. (14), while in our study all patients were treated with newer-generation DES (43% of DESs were everolimus and 57% were zotarolimus), which could have contributed to the lower TVR.
J-CTO score and clinical outcomes
In accordance with the previous studies, we confirmed that independent predictors of MACEs were J-CTO score (22) and successful PCI of CTO (23,24) as demonstrated by our multivariable Cox model. Furthermore, we found that high J-CTO score was independently associated with unfavorable clinical outcomes, which shows that differences in lesion complexity might significantly account for the differences in the overall clinical outcomes. However, no relevant data were mentioned in the study by Lee et al. (14) and Yamamoto et al. (21), which might also account for the difference in findings compared to our study.
Procedural success rate and safety of CTO PCI
A large part of the higher success rate (87.6%) can be attributed to the use of recently innovated devices such as tapered wires or microcatheters, and advances in interventional techniques as evidenced by the fact that 36.2% of the procedures used the retrograde approach. Similar results were obtained in several large multicenter registries in the United States, Japan and Europe, with success rates of 86%, 88%, and 89%, respectively (4-6). A possible explanation for the slightly lower success rates in our study compared with the Japanese and European registries could be ascribed to the selection of patients with slightly higher average J-CTO scores in the current study.
In this study, the periprocedural complication rate was acceptable (6.2%), as compared to the 7%, 0.53%, and 2.6% rate, found in the registries in the United States, Japan and Europe, respectively (4-6). The complication that occurred was a non-lethal clinical perforation during the procedure, which was treated quickly and successfully by coil sealing, cover stenting and emergency pericardiocentesis when cardiac tamponade occurred.
Limitations
First, this study is a single-center prospective study, in which unmeasured variables and selection bias on the part of operators toward cases may have influenced the results; thus, a lack of randomization needs to be considered as a limitation of our study. Additionally, it is probable that patients with high CTO score had more complex angiographic characteristics and more comorbidities which could have adversely affected subsequent outcomes. As a result, the true benefits of PCI for CTO revascularization remain to be assessed by dedicated RCTs. Furthermore, procedures were performed by several highly experienced operators in our center, which limits the aptness of extrapolation of the study results to less experienced centers and operators. In addition, the number of patients, particularly in the failed CTO PCI group (n=18 and 3 lost to follow-up) was relatively small. Finally, although long-term follow-up was not performed, the study will be continued for 36 months to assess the long-term outcomes of PCI for CTOs.
Conclusions
Our study shows that among patients with CTOs, high J-CTO score was independently associated with worse clinical outcomes. Moreover, successful PCI was associated with a lower risk of midterm MACE compared to failed revascularization of CTOs. Further well-designed research will be needed to explore the exact benefits and optimal therapies in this specific population with CTO.
Acknowledgements
Funding: The study was supported by the Science and Technology Planning Project of Guangdong Province, China (Grant No: 2016A020216022).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study protocol was approved by the Research Ethics Committee of Guangdong General Hospital, Guangdong Academy of Medical Sciences [No. GDREC2017196H(R1)], with written informed consent was obtained for all participants.
References
- Fefer P, Knudtson M, Cheema A, et al. Current perspectives on coronary chronic total occlusions: the Canadian Multicenter Chronic Total Occlusions Registry. J Am Coll Cardiol 2012;59:991-7. [Crossref] [PubMed]
- Werner GS, Martin-Yuste V, Hildick-Smith D, et al. A randomized multicentre trial to compare revascularization with optimal medical therapy for the treatment of chronic total coronary occlusions. Eur Heart J 2018;39:2484-93. [Crossref] [PubMed]
- Tomasello SD, Boukhris M, Giubilato S, et al. Management strategies in patients affected by chronic total occlusions: results from the Italian Registry of Chronic Total Occlusions. Eur Heart J 2015;36:3189-98. [Crossref] [PubMed]
- Sapontis J, Salisbury A, Yeh R, et al. Early Procedural and Health Status Outcomes After Chronic Total Occlusion Angioplasty: A Report From the OPEN-CTO Registry (Outcomes, Patient Health Status, and Efficiency in Chronic Total Occlusion Hybrid Procedures). JACC Cardiovasc Interv 2017;10:1523-34. [Crossref] [PubMed]
- Habara M, Tsuchikane E, Muramatsu T, et al. Comparison of percutaneous coronary intervention for chronic total occlusion outcome according to operator experience from the Japanese retrograde summit registry. Catheter Cardiovasc Interv 2016;87:1027-35. [Crossref] [PubMed]
- Maeremans J, Walsh S, Knaapen P, et al. The Hybrid Algorithm for Treating Chronic Total Occlusions in Europe: The RECHARGE Registry. J Am Coll Cardiol 2016;68:1958-70. [Crossref] [PubMed]
- Jang WJ, Yang JH, Choi SH, et al. Long-term survival benefit of revascularization compared with medical therapy in patients with coronary chronic total occlusion and well-developed collateral circulation. JACC Cardiovasc Interv 2015;8:271-9. [Crossref] [PubMed]
- Christopoulos G, Karmpaliotis D, Alaswad K, et al. Application and outcomes of a hybrid approach to chronic total occlusion percutaneous coronary intervention in a contemporary multicenter US registry. Int J Cardiol 2015;198:222-8. [Crossref] [PubMed]
- Wilson WM, Walsh S, Yan A, et al. Hybrid approach improves success of chronic total occlusion angioplasty. Heart 2016;102:1486-93. [Crossref] [PubMed]
- Akinseye OA, Haji SA, Koshy SKG, et al. Outcomes of Percutaneous Antegrade Intraluminal Coronary Intervention of Chronic Total Occlusion With Remote Surgical Backup. Curr Probl Cardiol 2018. [Epub ahead of print]. [Crossref] [PubMed]
- Park SJ. Optimal Medical Therapy With or Without Stenting for Coronary Chronic Total Occlusion: DECISION-CTO. (ClinicalTrials.gov Identifier: NCT01078051). Paper presented at: American College Cardiology Congress; March 18,2017; Washington, DC. Available online: https://www.acc.org/Latest-in-Cardiology/Clinical-Trials/2017/03/17/08/40/DECISION-CTO. Accessed August 28, 2018.
- Elias J, van Dongen IM, Råmunddal T, et al. Long-term impact of chronic total occlusion recanalisation in patients with ST-elevation myocardial infarction. Heart 2018;104:1432-8. [Crossref] [PubMed]
- Kim BS, Yang JH, Jang WJ, et al. Clinical outcomes of multiple chronic total occlusions in coronary arteries according to three therapeutic strategies: Bypass surgery, percutaneous intervention and medication. Int J Cardiol 2015;197:2-7. [Crossref] [PubMed]
- Lee PH, Lee SW, Park HS, et al. Successful Recanalization of Native Coronary Chronic Total Occlusion Is Not Associated With Improved Long-Term Survival. JACC Cardiovasc Interv 2016;9:530-8. [Crossref] [PubMed]
- Sianos G, Werner G, Galassi A, et al. Recanalisation of chronic total coronary occlusions: 2012 consensus document from the EuroCTO club. EuroIntervention 2012;8:139-45. [Crossref] [PubMed]
- Morino Y, Abe M, Morimoto T, et al. Predicting successful guidewire crossing through chronic total occlusion of native coronary lesions within 30 minutes: the J-CTO (Multicenter CTO Registry in Japan) score as a difficulty grading and time assessment tool. JACC Cardiovasc Interv 2011;4:213-21. [Crossref] [PubMed]
- Alpert JS. The Fourth Edition of the Universal Definition of Myocardial Infarction. Am J Med 2018;131:1265-6.
- Cutlip DE, Windecker S, Mehran R, et al. Clinical end points in coronary stent trials: a case for standardized definitions. Circulation 2007;115:2344-51. [Crossref] [PubMed]
- George S, Cockburn J, Clayton TC, et al. Long-term follow-up of elective chronic total coronary occlusion angioplasty: analysis from the U.K. Central Cardiac Audit Database. J Am Coll Cardiol 2014;64:235-43. [Crossref] [PubMed]
- Christakopoulos GE, Christopoulos G, Carlino M, et al. Meta-analysis of clinical outcomes of patients who underwent percutaneous coronary interventions for chronic total occlusions. Am J Cardiol 2015;115:1367-75. [Crossref] [PubMed]
- Yamamoto E, Natsuaki M, Morimoto T, et al. Long-term outcomes after percutaneous coronary intervention for chronic total occlusion (from the CREDO-Kyoto registry cohort-2). Am J Cardiol 2013;112:767-74. [Crossref] [PubMed]
- Galassi AR, Sianos G, Werner GS, et al. Retrograde Recanalization of Chronic Total Occlusions in Europe: Procedural, In-Hospital, and Long-Term Outcomes From the Multicenter ERCTO Registry. J Am Coll Cardiol 2015;65:2388-400. [Crossref] [PubMed]
- Mehran R, Claessen BE, Godino C, et al. Long-term outcome of percutaneous coronary intervention for chronic total occlusions. JACC Cardiovasc Interv 2011;4:952-61. [Crossref] [PubMed]
- Niccoli G, De Felice F, Belloni F, et al. Late (3 years) follow-up of successful versus unsuccessful revascularization in chronic total coronary occlusions treated by drug eluting stent. Am J Cardiol 2012;110:948-53. [Crossref] [PubMed]


