Personal factors influencing breast cancer patients’ perception of breast conservation surgery in West China
Introduction
In addition to the certain disease characteristics that determine eligibility for therapy, the National Institute of Health Consensus Conference acknowledged that patient’s preference and understanding of therapy were very important during treatment decision process (1). In Europe and the USA, the majority of patients who were more willing to choose breast conservation surgery (BCS) and satisfied with the therapeutic efficacy had better perception of BCS (2-4). In China, however, the proportion of patients choosing BCS is very low. A prospective multicenter case control study carried out by the Cancer Hospital, Chinese Academy of Medical Sciences (CAMS) and nine other hospitals across China concluded that, in 4,461 patients, BCS was only performed on 872 (19.5%) patients who were eligible for BCS, accounting for 9.0% of all surgical breast cancer patients during the same period (5). And another retrospective study including seven tertiary hospitals of respectively geographic regions have shown that, from 1999 to 2008, although the percentage of BCS increased from 1.3% to 11.8%, it was only about one-tenth of surgical patients (6).
This difference could be as a result of patient’s perception of BCS. Our previous study suggested that Chinese breast cancer patients (CBCP) lacked full understanding of BCS (7). There are no specialized studies that have sought to discover what Chinese patients with breast cancer knew about BCS, despite the fact that Chinese patients are among the largest ethnic groups in communities worldwide. The aims of our study were to evaluate CBCP’ perception of BCS and explore influencing factors.
Methods
Subjects
A cross-sectional study was conducted to investigate understanding of BCS among breast cancer patients in West China Hospital, the tertiary care hospital and the largest hospital in Asia, during the period from July 2013 to September 2017. To be eligible for the study, subjects were required to be female, to be 18 years or older, to have a pathological diagnosis, preoperative assessment showing stage I or stage II stage and to be well enough to fill out a questionnaire independently and communicate with the interviewer. Participants who did not complete their questionnaire were excluded.
Methodology
We constructed an open questionnaire based on published studies in combination with some unique aspects of this study. A pre-test was carried out in 127 patients, and the reliability and validity of the questionnaire were analyzed. We trained interviewer using a unified program. All participants were given enough information explaining the study and were asked not to share their information with others. Questionnaires were filled out by participants or with the help of the interviewer.
In the first section of the questionnaire, we collected information on age, religion, income, education and marital status. Next, participants answered further questions, such as whether surgery had been performed and their understanding of BCS. We used a four-point Likert scale (ranging from ‘never heard’ to ‘have clear understanding’). If patients had never heard of BCS, the investigation was closed, otherwise, they were asked to qualify their understanding of BCS. According to the responses, investigators rated the level of the patient’s understanding (patients who had only heard of BCS and did not have specific knowledge of it were classified as “skin-deep cognition”, understanding the costs and the postoperative treatment plan were classified as “penetrating cognition”, and understanding more than the therapeutic effects, surgical techniques and indications were classified as “more penetrating cognition”). The last section of the questionnaire obtained information on the patients’ knowledge-acquisition pathways. Four main pathways were included.
All the responses and other information obtained were inputted into a computer by an independent investigator. The study was approved by the ethical committee of Cancer Center of Sichuan University, China (ID of ethics approval: SCHX-2013-0625).
Statistical analysis
SPSS version 16.0 was used for statistical analysis. The Chi-square test was used to analyze the relevant factors influencing patient understanding of BCS. Binary logistic regression was used to calculate the odds ratios (OR) and 95% confidence intervals (CI). The level of statistical significance was set at P<0.05.
Results
Patients’ characteristics
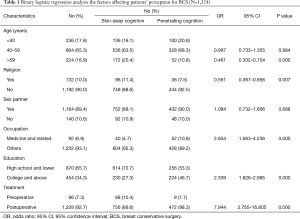
One thousand four hundred and ninety-six participants were contacted and 1,324 completed the questionnaire, effective response rate was 88.5%. Table 1 listed the characteristics of the participants. The patients were, on average, 49.1 years old (range 22–75) years, and 65.3% were 40–59 years of age. Of 1,324 patients, 89.4% were married or cohabiting, 34.3% were educated to college level and above, and 92.7% of patients were postoperative.
Full table
Perception of BCS
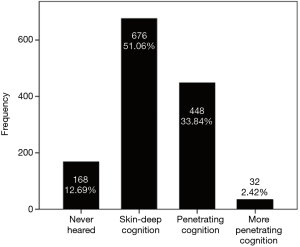
The results are shown in Figure 1. One hundred and sixty-eight of these 1,324 patients (12.69%) had never heard of BCS; 676 participants (51.06%) had skin-deep cognition; 448 patients (33.84%) had penetrating cognition; and 32 patients (2.42%) had more penetrating cognition. To avoid error bias caused by a few cases, patients’ perception was classified into two categories: one is skin-deep group including never heard and skin-deep cognition, and the another is penetrating group including penetrating and more penetrating cognition during statistical analysis.
Factors affecting patient understanding
Table 1 showed the factors such as patient’s age, religion, occupation, educational background and whether the patient was postoperative or not which were significantly associated with patient understanding of BCS (P<0.05). Compared with younger women, women aged 60 years or older were less likely to have better understanding of BCS (OR =0.461, 95% CI: 0.302–0.704). Patients with no a stated religion had better understanding than those with a stated religion (OR =0.561, 95% CI: 0.367–0.856). Patients in the medical or related profession had better understanding of BCS than those in other professions (OR =2.654; 95% CI: 1.633–4.236). Compared with less educated patients, those with a college education or above had better understanding of BCS (OR =2.339, 95% CI: 1.826–2.995). Moreover, postoperative patients had better understanding than pre-operative patients (OR =7.944, 95% CI: 3.755–16.805). No discernable patterns for knowledge were observed by studying the patients’ sexual histories.
How do patients obtain information?
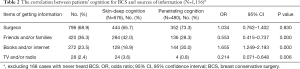
We asked patients to indicate their sources of information on BCS. As shown in Table 2, the most common source of information was doctors, as more than two-thirds of patients (68.9%) reported that they had consulted doctors. Relatives, friends and/or families (36.3%) were also frequently cited as a source of information. Furthermore, less than a quarter of patients (23.5%) reported that they had searched breast cancer treatment information on the internet or in books. As expected, patients mainly received information about breast cancer treatment from their surgeons. However, this was not a significant source of information (OR =1.034; 95% CI: 0.762–1.402). We examined patients’ knowledge across different categories of information sources whilst controlling for age, religion, educational background, occupation, sexual history, and whether they were postoperative. Table 2 showed that awareness of BCS could be better amongst patients who used books or the internet to obtain information (OR =1.665; 95% CI: 1.249–2.193). Information obtained from friends/families and from television and radio also affected patients’ awareness (P<0.01). However, patients who obtained information from these sources were inclined to be in the skin-deep cognition group (OR =0.553; 95% CI: 0.415–0.737; OR =0.214; 95% CI: 0.071–0.648).
Full table
Discussion
Over the past hundred years, there have been major changes in breast cancer surgery. In developed countries, the majority of patients had knowledge of recurrence and survival of BCS and mastectomy, and they participated in treatment decision-making and were more willing to choose BCS (2-4). In China, however, most patients preferred not to choose BCS (5-7). Studies have shown that patient’s preference and understanding of therapy were very important during the treatment decision process (1,8,9). The present study showed that in West China, only 2.42% of patients had greater perception of BCS, 12.69% had never heard of BCS, and 51.06% had only heard of BCS but did not have specific knowledge (Figure 1). In our previous study (7), we found that more than half of CBCP stated that the most appropriate treatment for them was mastectomy and they had a commonly expressed opinion that the mastectomy would “get rid of all the cancer”. A study of patients in Hong Kong by Chua et al. showed the same result (10).
Some studies showed that age, occupation, educational background and whether the patient was postoperative were factors influencing patients’ perception for BCS (4,11,12). The present study showed the same results (Table 1). Compared with younger women, women aged 60 years or older were less likely to have better understanding of BCS. Compared with patients who were not in the medical profession, those in the medical or related profession had better understanding of BCS. Compared with patients who were less well educated, women with a college education or above had better understanding of BCS, and patients who were postoperative had better understanding than pre-operative patients. The reason may be that patients with younger, working in the medical profession, and/or having knowledge are more eager to obtain knowledge and have better means of researching therapies. Moreover, our study found that patients without a stated religion had a better awareness of BCS than those with a stated religion. This suggested that faith could affect patients’ perception. No discernable patterns for knowledge were observed by studying patients’ sexual histories. There was some contradiction compared with previous research result (7).
“Skin-deep cognition” in CBCP may be due to multiple factors. First, it may be that patients lack access for information (13-15). Our study results support this opinion patients had not been exposed to a great variety of information sources for BCS. In fact, most patients (68.9%) recalled being told about BCS by their surgeons, but among these patients, the majority of understanding was “skin-deep” (Table 2). Only 23.5% of patients reported that they had “penetrating cognition”, they obtained information by accessing books or internet (Table 2). Second, according to our results, it may be that the cognitive barriers related to medical knowledge may inhibit understanding of risk-related information. There was compelling evidence that patients had difficulty understanding medical information about their diseases and treatments (16,17). In addition, during surgeon-patient communication, such terms were used that the patients did not truly comprehend the risks and benefits of BCS. And the most of participants have lower education level raising the difficulty to understand BCS.
It is possible that there were other explanations for patients’ “skin-deep cognition”. Firstly, some of the sources that patients consulted may have provided inaccurate information. In fact, friends and families/relations were the second most commonly used sources of information (Table 2), but they may have provided patients with anecdotal and/or erroneous information. This is an important consideration, as anecdotal information has been found to have an unfavorable influence on patients’ treatment decisions (18,19). Additionally, it is possible that the information given was incomplete and did not contain information regarding the ascendancy of BCS compared with mastectomy (20).
Secondly, patients may not have been aware of the benefits of BCS (21,22) and they did not consider conserving or resetting the breast when the surgery decision was made. They conventional have thought that mastectomy was the most appropriate treatment and did not consider the information about BCS.
Thirdly, it is possible that Chinese surgeons doubted the therapeutic effect of BCS and/or did not have enough self-confidence perform the surgery. They maybe have not provided enough information to their patients. There was evidence that many surgeons did not routinely perform BCS as the first and best treatment modality (23). However, a study showed that patient’s preference was different from their doctor’s recommendations (24). Fourthly, it is possible that when the patients were diagnosed with breast cancer, they felt so scared that they did not hear, remember or understand exactly the information given to them (25). In addition, there may be other factors to be considered by further study.
In summary, most CBCP only know that BCS exists and do not know how it compares to mastectomy as a treatment choice, so they do not state a preference for BCS more frequently. Our results could be interpreted to suggest that women need to be better informed before surgery to equip them to participate in surgery decision-making process and make the best decision. However, there were some limitations to the study. The questionnaire was not perfect and all the patients attended the same hospital and only represent the situation in west China. There are no information on care providers. Further and nationwide research is needed.
These findings are particularly noteworthy as they come after many years of efforts to improve the quality and quantity of information supplied to breast cancer patients and to promote patient participation in the surgical treatment decision process. We must find useful methods, either using decision aids and/or by improving patient–surgeon communication, for discussing the risks and benefits of BCS to breast cancer patients. Until patients obtain enough and necessary information about their own medical condition and right decision was making.
Acknowledgments
We thank Hong Zheng, Hongyu Zhuo, Yu Jiang and Jian-Jun He for collecting data.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study was approved by the ethical committee of Cancer Center of Sichuan University, China (ID of ethics approval: SCHX-2013-0625) and written informed consent was obtained from all patients. The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
References
- Consensus conference. Treatment of early stage breast cancer. National Institutes of Health. Conn Med 1991;55:101-7. [PubMed]
- Recio-Saucedo A, Gerty S, Foster C, et al. Information requirements of young women with breast cancer treated with mastectomy or breast conserving surgery: A systematic review. Breast 2016;25:1-13. [Crossref] [PubMed]
- Durand MA, Yen RW, O'Malley AJ, et al. What matters most: protocol for a randomized controlled trial of breast cancer surgery encounter decision aids across socioeconomic strata. BMC Public Health 2018;18:241. [Crossref] [PubMed]
- Temple WJ, Russell ML, Parsons LL, et al. Conservation surgery for breast cancer as the preferred choice: a prospective analysis. J Clin Oncol 2006;24:3367-73. [Crossref] [PubMed]
- Zhang BN, Shao ZM, Qiao XM, et al. A prospective multicenter clinical trial of breast conserving therapy for early breast cancer in China. Zhonghua Zhong Liu Za Zhi 2005;27:680-4. [PubMed]
- Zhang BL, Sivasubramaniam PG, Zhang Q, et al. Trends in Radical Surgical Treatment Methods for Breast Malignancies in China: A Multicenter 10-Year Retrospective Study. Oncologist 2015;20:1036-43. [Crossref] [PubMed]
- Zhang L, Jiang M, Zhou Y, et al. Survey on breast cancer patients in China toward breast-conserving surgery. Psychooncology 2012;21:488-95. [Crossref] [PubMed]
- Mac Bride MB, Neal L, Dilaveri CA, et al. Factors associated with surgical decision making in women with early-stage breast cancer: a literature review. J Womens Health (Larchmt) 2013;22:236-42. [Crossref] [PubMed]
- Zikmund-Fisher BJ, Windschitl PD, Exe N, et al. “I'll do what they did”: social norm information and cancer treatment decisions. Patient Educ Couns 2011;85:225-9. [Crossref] [PubMed]
- Chua MS, Mok TS, Kwan WH, et al. Knowledge, perceptions, and attitudes of Hong Kong Chinese women on screening mammography and early breast cancer management. Breast J 2005;11:52-6. [Crossref] [PubMed]
- Livaudais JC, Franco R, Fei K, et al. Breast cancer treatment decision-making: are we asking too much of patients? J Gen Intern Med 2013;28:630-6. [Crossref] [PubMed]
- Bleicher RJ, Abrahamse P, Hawley ST, et al. The influence of age on the breast surgery decision-making process. Ann Surg Oncol 2008;15:854-62. [Crossref] [PubMed]
- Janz NK, Mujahid MS, Hawley ST, et al. Racial/ethnic differences in adequacy of information and support for women with breast cancer. Cancer 2008;113:1058-67. [Crossref] [PubMed]
- Freedman RA, Kouri EM, West DW, et al. Association of Breast Cancer Knowledge With Receipt of Guideline-Recommended Breast Cancer Treatment. J Oncol Pract 2016;12:e613-25. [Crossref] [PubMed]
- Qiu WL, Lin PJ, Ruan FQ, et al. Requests for health education from Chinese cancer patients during their recovery period: a cross-sectional study. J Cancer Educ 2013;28:428-34. [Crossref] [PubMed]
- Lillie SE, Brewer NT, O'Neill SC, et al. Retention and use of breast cancer recurrence risk information from genomic tests: The role of health literacy. Cancer Epidemiol Biomarkers Prev 2007;16:249-55. [Crossref] [PubMed]
- Mancuso CA, Rincon M. Asthma patients' assessments of health care and medical decision making: The role of health literacy. J Asthma 2006;43:41-4. [Crossref] [PubMed]
- Fagerlin A, Wang C, Ubel P. Reducing the influence of anecdotal reasoning on people's health care decisions: is a picture worth a thousand statistics? Med Decis Making 2005;25:398-405. [Crossref] [PubMed]
- Carey M, Herrmann A, Hall A, et al. Exploring health literacy and preferences for risk communication among medical oncology patients. PLoS One 2018;13:e0203988. [Crossref] [PubMed]
- Frongillo M, Feibelmann S, Belkora J, et al. Is there shared decision making when the provider makes a recommendation? Patient Educ Couns 2013;90:69-73. [Crossref] [PubMed]
- Arndt V, Stegmaier C, Ziegler H, et al. Quality of life over 5 years in women with breast cancer after breast-conserving therapy versus mastectomy: a population-based study. J Cancer Res Clin Oncol 2008;134:1311-8. [Crossref] [PubMed]
- Maly RC, Stein JA, Umezawa Y, et al. Racial/ethnic differences in breast cancer outcomes among older patients: effects of physician communication and patient empowerment. Health Psychol 2008;27:728-36. [Crossref] [PubMed]
- Sattaratnamai A, Samankatiwat N, Lohsiriwat V. Surgeons’ Recommendation is the Factor in Determining the Breast Cancer Surgery Procedures: an Experience from Rural Hospital in Thailand. Asian Pac J Cancer Prev 2018;19:1189-93. [PubMed]
- Caldon LJ, Collins KA, Wilde DJ, et al. Why do hospital mastectomy rates vary? Differences in the decision-making experiences of women with breast cancer. Br J Cancer 2011;104:1551-7. [Crossref] [PubMed]
- Rönnlund M, Sundström A, Sörman DE, et al. Effects of perceived long-term stress on subjective and objective aspects of memory and cognitive functioning in a middle-aged population-based sample. J Genet Psychol 2013;174:25-41. [Crossref] [PubMed]