
Prevalence of and factors related to microvascular complications in patients with type 2 diabetes mellitus in Tianjin, China: a cross-sectional study
Introduction
Type 2 diabetes mellitus (T2DM) is a progressive endocrine disease accompanied by a variety of metabolic disorders that manifests clinically as high blood glucose. T2DM has swiftly become an urgent health problem because of its associated complications. Since chronic hyperglycemia-related damage to small blood vessels results in complications, patients with T2DM with longer disease durations are more likely to develop microvascular complications, such as retinopathy, neuropathy and nephropathy, which will lead to the decline in patients’ quality of life, disability and even death (1). Diabetic retinopathy is one of the most common microvascular complications of diabetes and irreversible blindness-causing disease in the population. In particular, proliferative retinopathy is a unique complication of diabetes and is rarely associated with other diseases. Diabetic neuropathy can involve the central and peripheral nerves; the latter is more common. Diabetic neuropathy is related to the duration of diabetes, blood glucose levels and other factors. Patients with a diabetes duration of more than 10 years are prone to obvious clinical manifestations of neuropathy. In China, approximately 20~40% of patients with T2DM also suffer from diabetic nephropathy, which has become the main cause of chronic kidney disease (CKD) and end-stage nephropathy (2). Moreover, the cost of the treatment of microvascular complications accounts for the majority of diabetes-related costs, bringing a heavy economic burden to patients, families and society (3). Therefore, the detection and identification of risk factors for microvascular complications (retinopathy, neuropathy and nephropathy) is imperative and may prevent the progression towards blindness, diabetic foot ulcers and end-stage renal disease (4). Additionally, the investigation of the prevalence and the factors associated with diabetic microvascular complications can enhance the knowledge of diabetic patients and can provide beneficial information for practicable policies and strategies for the prevention and treatment of diabetic microvascular complications.
Above all, this study aimed to determine the prevalence of and risk factors for type 2 diabetic microvascular complications in Tianjin, China.
Methods
Subjects and data collection
This observational, cross-sectional study was conducted at 8 hospitals in urban and suburban regions of Tianjin, China; of the 8 hospitals, 6 were Grade A, 1 was Grade 2B, and the other was a private hospital. The study population was outpatients with T2DM who were consecutively recruited at each hospital from November 2015 to January 2016. The exclusion criteria were as follows: (I) patients with diagnosed T1DM; (II) patients younger than 18 years old; and (III) patients who were not willing to give prior informed consent.
The information collected from the subjects mainly included demographic characteristics and clinical information. The demographic information, including gender, family history of T2DM, duration of diabetes, smoking, alcohol consumption behavior and physical activity, was collected by trained interviewers through the completion of the questionnaire. The clinical information, regarding height, weight, physical examinations, laboratory examinations and biochemical indicators was extracted from field measurement and electronic medical records. The height and weight of the enrolled participants were measured using standardized techniques, and their body mass index (BMI) was calculated. The presence or absence of microvascular complications and microvascular complication types was identified in two ways: a medical history or physical and laboratory examinations. Physical examination included ankle reflex, pain sense, vibration sense, pressure sense and temperature sense, while the laboratory examinations included a routine blood examination, a routine urine examination and a renal function test. Notably, diabetic neuropathy includes central neuropathy and peripheral neuropathy, of which the latter is more common. Therefore, only peripheral neuropathy is considered in this study.
Definitions
(I) The diagnosis of T2DM was performed according to the following international standards (WHO 1999) (5): fasting plasma glucose (FPG) ≥7.0 mmol/L and/or 2-hour postprandial plasma glucose (PPG) or casual plasma glucose ≥11.1 mmol/L; (II) the diagnosis of diabetic retinopathy was performed according to the following relevant international clinical grading standards developed in 2002 (6): diabetic retinopathy was divided into proliferative stages and non-proliferative stages with a total of 6 stages: (i) the nonproliferation period of diabetic retinopathy (NP-DR), period I: micro-hemangioma and leakage of small blood vessels; period II: rapid seepage; and period III: cotton-wool spots; (ii) the proliferation period of diabetic retinopathy (PDR), period IV: the formation of new blood vessels and vitreous hemorrhage; period V: fibrous vascular proliferation and vitreous occurrence; and period VI: tractional retinal detachment and blindness; (III) the diagnosis of diabetic neuropathy was performed using the following criteria (7); the diagnosis of diabetes along with the occurrence of clinical neuropathy symptoms (pain, numbness, paresthesia, etc.) and abnormal results in at least 1 of the 5 examinations (ankle reflex, acupuncture pain, vibration, pressure, temperature). In the absence of clinical symptoms, at least 2 of the 5 examinations needed to be abnormal for diabetic peripheral neuropathy to be diagnosed; (IV) diabetic nephropathy was diagnosed using the following criteria (7): diabetic nephropathy is usually diagnosed based on an increased urine albumin/creatinine ratio (UACR) and a reduced estimated glomerular filtration rate (eGFR) with the exclusion of other CKDs: (i) a random UACR ≥30 mg/g indicated increased urinary albumin; (ii) eGFR <60 mL·min–1·(1.73 m2)–1 can be used to indicate GFR decline; (V) smoking was defined as smoking more than one cigarette per day for >1 year; (VI) alcohol consumption was defined by the following criteria: ethanol intake exceeding 20 g per day for more than 1 year. Ethanol content was calculated as follows: ethanol content = alcohol consumption * alcohol content * 0.8 (8); and (VII) regular exercise was defined as performing moderate-intensity physical activity at least 3 times per week.
Data management and statistical analysis
The data were double-entered and validated by EpiData 3.1 (EpiData Association, Odense, Denmark). Statistical analysis was carried out using SPSS version 22.0 (SPSS Inc., Chicago, IL, USA). For comparison, we divided all patients into four groups: (I) patients who did not have any diabetic microvascular complications, (II) patients with diabetic retinopathy, (III) patients with diabetic neuropathy, and (IV) patients with diabetic nephropathy. Patients with two or more complications were counted separately in the appropriate group. Continuous normally distributed variables are presented as the mean and standard deviation (SD), while data with a non-normal distribution are reported as the median with interquartile range; categorical variables are expressed as counts and percentages. Student’s t-test or the Mann-Whitney test were used to compare means for numerical data, and the Wilcoxon rank sum test was applied when variables were nonnormally distributed. Chi-square tests were used to analyze the differences in categorical between the 4 groups, and if one of the theoretical counts was less than 1 or one-fifth of the theoretical frequency was less than 5, Fisher’s exact probability test was performed.
Univariate and multivariate logistic regression were used to assess the association between the responses and independent variables. Odds ratios (ORs) with 95% confidence intervals (CIs) were calculated to assess the risk factors associated with microvascular complications. Associations were considered to be significant when a P value was less than 0.05.
Results
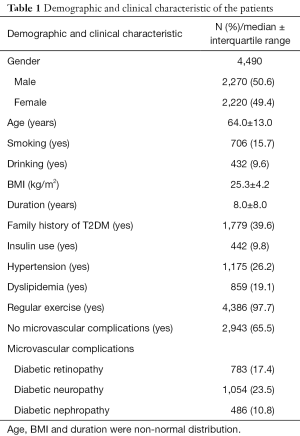
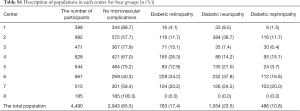
A total of 4,490 patients with T2DM, including 2,270 (50.6%) males, were recruited for the study. The median age was 64.0±13.0 years. The median BMI was 25.3±4.2 kg/cm2. The median diabetes duration was 8.0±8.0 years. The proportions of smokers and alcohol consumers were 15.7% and 9.6%, respectively. There were 1,779 (39.6%) patients with a family history of T2DM. Approximately 9.8% of the total subjects used only insulin treatment. Of all the study participants, 1,175 (26.2%) had hypertension and 859 (19.1%) had dyslipidemia. There are 2,943 of the 4,490 (65.5%) participants without microvascular complication. Diabetic neuropathy was the most frequent complication (23.5%), followed by diabetic retinopathy (17.4%) and diabetic nephropathy (10.8%) (Table 1). The prevalence of complications in each center was showed in the Table S1.
Full table
Full table
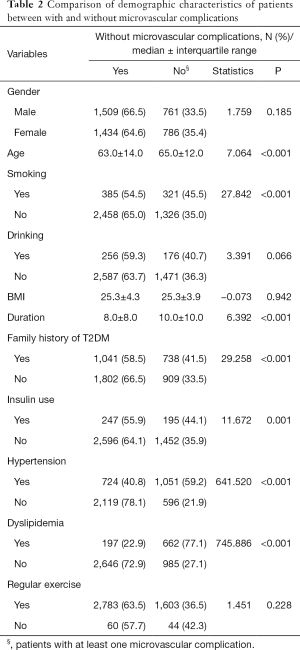
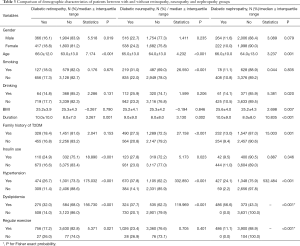
The results in Table 2 show that age, smoking, diabetes duration, family history of T2DM, insulin use, hypertension and dyslipidemia were significantly different between patients with and without microvascular complications. Table 3 illustrates that the females had a higher prevalence of retinopathy complications than males. The difference tests conducted on the four groups all illustrated that patients with microvascular complications were older and had a longer duration of diabetes (Tables 2,3). There was also a significant difference between smokers and nonsmokers and between alcohol consumers and non-alcohol consumers in neuropathy and nephropathy, respectively. Compared with patients who were treated with noninsulin treatments, the patients treated with insulin showed a significantly higher prevalence of retinopathy and neuropathy complications. The study also revealed that the prevalence of microvascular complications was higher in patients with hypertension and dyslipidemia than in those who had no hypertension or dyslipidemia (P<0.001). We observed that patients in the non-regular physical exercise group had a higher prevalence of retinopathy and nephropathy complications, and the difference was statistically significant.
Full table
Full table
The results of the univariate logistic regression are shown in Table 4. The risk factors for retinopathy were female sex, older age, longer duration of diabetes, insulin use, hypertension and dyslipidemia. The significant risk factors for neuropathy were older age, smoking, family history of diabetes, duration of diabetes, insulin use, hypertension, dyslipidemia and lack of regular physical exercise. Again, significant risk factors for nephropathy were older age, family history of T2DM, duration of diabetes, insulin use, hypertension, dyslipidemia and lack of regular physical exercise.
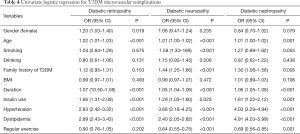
Full table
Table 5 shows the results of the multivariable logistic regression. The sex and age (continuous variable) of the subjects were not associated with any diabetic microvascular complications. A longer duration of diabetes, insulin use, and the presence of hypertension and dyslipidemia were found to be significantly associated with the presence of the three kinds of diabetic microvascular complications. Smoking was a significant risk factor for neuropathy (OR =1.7; 95% CI: 1.41–2.06, P<0.001). A significant association was also observed between neuropathy and family history of diabetes (OR =1.30; 95% CI: 1.12–1.51; P<0.001). Regular exercise was shown to be a protective factor against neuropathy (OR =0.68; 95% CI: 0.58–0.80, P<0.001) and nephropathy (OR =0.73; 95% CI: 0.58–0.90; P=0.005).
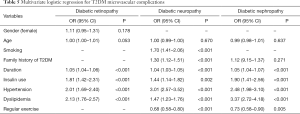
Full table
Discussion
China has become the country with the highest number of people with diabetes and will face major challenges associated with diabetic complications (9). Therefore, the prevention of complications is very important with regard to the general protection of diabetic patients (10). This study aimed to report the characteristics of various type 2 diabetic microvascular complications (retinopathy, neuropathy, nephropathy) and explore their possible risk factors.
Our study assessed the prevalence of microvascular complications in 4,490 outpatients from 8 hospitals in urban and suburban regions of Tianjin, China and found that 65.5% of subjects presented without microvascular complication. The overall prevalence in our study was lower than that reported in Australia, Colombia, and Iran (11-13) but was higher than that reported in a study from Ireland (14). Compared with the prevalence of microvascular complications identified in a cross-sectional hospital-based study carried out in four major cities of mainland China in 2007 (34.7%) (15), the prevalence in our study was similar (34.5%), which meant that although complications related to diabetes were well controlled in Tianjin, China, type 2 diabetic microvascular complications have still placed a very large burden on the healthcare system.
Multiple logistic regression analysis showed that the duration of T2DM, insulin use, hypertension and dyslipidemia were the factors responsible for the development of diabetic complications (nephropathy, neuropathy and nephropathy). Consistent with previous studies (16-18), the present study demonstrated that a longer duration of diabetes, hypertension and dyslipidemia were independently associated with all kinds of microvascular complications. A reasonable explanation is that hypertension hastens the development and progression of microvascular complications due to increased intracellular hyperglycemia (16). Dyslipidemia may cause or exacerbate diabetic complications by altering the coagulation-fibrinolytic system, changing membrane permeability, damaging endothelial cells and increasing atherosclerosis. Hyperlipidemia was also associated with a faster decrease in GFR and progression of albuminuria and nephropathy (19). The association between insulin use and the occurrence of microvascular complications has been reported in several studies (13,16), and our findings also showed a concurrent result. Insulin on its own does not seem to be associated with the development of complications. A common phenomenon in China is that the primary reason for starting insulin therapy in patients with T2DM is poor glycemic control despite taking oral hypoglycemic agents. This phenomenon indicates that insulin is used only when microvascular damage has already occurred, suggesting that poor glycemic control could be the reason for the association between insulin treatment and complications in this study.
The prevalence of diabetic neuropathy stood out at 23.5%, which was ranked as the most common diabetic microvascular complication. The prevalence of neuropathy was higher than that found in other studies in China (10.7%) and Colombia (14.5%) (13,15). In addition, the prevalence was lower than that found in studies performed in Iran (44.6%), Korea (33.5%), and India (26.8%) (12,20,21). Pradeepa et al. (22) also found a predominance of neuropathy in individuals with T2DM compared with the prevalence of the other microvascular complications. In addition to the common risk factors mentioned above, smoking, family of T2DM and lack of regular exercise also were risk factors of diabetic neuropathy. The harmful mechanism of smoking to diabetic neuropathy has not been clear. Tracey et al. (14) reported that smoking was identified as a risk factor for the development of the three types of microvascular complications, whereas others have reported that there was not a significant association between smoking and microvascular complications (23). Likewise, the association between diabetic microvascular complications and family history of diabetes has also been equivocal. Maghbooli et al. (24) found that family history was an independent risk factor for retinopathy, while our finding showed that family history was associated with neuropathy only. Further investigation is needed to provide more evidence for this relationship. Regular exercise is associated with numerous beneficial health effects. Regular exercise is considered important and can prevent diabetes-related complications. Many complications of diabetes mellitus seem to be attenuated by regular physical exercise (25) because regular physical exercise can increase energy expenditure. Therefore, it is an effective way to lower blood glucose levels.
In the present study, diabetic retinopathy ranked second in terms of frequency of occurrence (17.4%), which was similar to the findings of a study conducted in Hong Kong (26). A publication from the UK reported that in 10,709 patients with type 2 diabetes, the percentage of patients with retinopathy was 16.5%, which closely matched our findings. The figure in our study was much lower than those identified in Iran (35.7%), India (32.5%) and Pakistan (43%) (12,21,27). A meta-analysis of chronic complications that included 19 epidemiologic studies conducted from 1991 to 2012 in China indicated that the diabetic retinopathy prevalence was 23.0% (28).
Our study results showed that 10.8% of the subjects had diabetic nephropathy. In a study conducted in 4 cities in China from 1991 to 2000, the prevalence of nephropathy was observed to be higher than that in our study (39.7%) (26). A higher prevalence was also found in a study in Shanghai, China (33.2%) (29). Agrawal et al. (21) also found a high nephropathy prevalence in their study (30.2%). In addition, regular exercise also could prevent patients from developing nephropathy, of which the reason is the same as mentioned above.
There were several limitations to our study. First, a cross-sectional study does not allow inferences about the cause and effect relationship between microvascular complications and the factors that were explored. The study provided only partial evidence of causal associations. Second, several important values were not assessed at the time of observation, including blood pressure, plasma glucose, and HbA1c. Finally, although we have provided a unified definition of complications, the diagnosis of the disease is still subjective. Different doctors may combine their own experience to diagnose the disease, which will lead to the existence of confounders. This limitation is beyond our control.
Conclusions
This study mainly focused on microvascular complications because of their serious consequences. The prevalence of microvascular complications was high according to the present study. Longer diabetes duration, the presence of hypertension and dyslipidemia and insulin use were significantly associated with type 2 diabetic microvascular complications. Therefore, increasing the control of risk factors can reduce the occurrence of complications and improve the quality of life of patients. Nevertheless, this was only a cross-sectional study. Further cohort or trial studies should be carried out to confirm the causal relationship between risk factors, especially glycemic control-related risk factors, and diabetes microvascular complications.
Acknowledgments
The authors are grateful to 8 hospitals in Tianjin for providing data.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors state that the study had been approved by Medical ethics committee of Tianjin medical university. And the authors state that all the subjects had signed the information consent forms.
References
- Chawla A, Chawla R, Jaggi S. Microvasular and macrovascular complications in diabetes mellitus: Distinct or continuum? Indian J Endocrinol Metab 2016;20:546-51. [Crossref] [PubMed]
- Zhang L, Long J, Jiang W, et al. Trends in Chronic Kidney Disease in China. N Engl J Med 2016;375:905-6. [Crossref] [PubMed]
- Ayodele OE, Alebiosu CO, Salako BL. Diabetic nephropathy--a review of the natural history, burden, risk factors and treatment. J Natl Med Assoc 2004;96:1445-54. [PubMed]
- Margolis S. Diabetic microvascular complications: An overview. Advanced Studies in Medicine 2005;5:260-3.
- World Health Orgnization. Definition and diagnosis of diabetes mellitus and intermediate hyperglycemia: report of a WHO/IDF consultation, 2006. Geneva: WHO Document Production Services 2006.
- Wilkinson CP, Ferris FL, Klein RE, et al. Global Diabetic Retinopathy Project G: Proposed international clinical diabetic retinopathy and diabetic macular edema disease severity scales. Ophthalmology 2003;110:1677-82. [Crossref] [PubMed]
- Chinese Preventive Medicine Association. Guidelines for the prevention and treatment of type 2 diabetes in China (2017 edition). Chin J Pract Int Med 2018;38:292-344.
- Fatty Liver and Alcoholic Liver Disease Study Group of the Chinese Liver Disease Association. Guidelines for diagnosis and treatment of alcoholic liver disease. Zhonghua Gan Zang Bing Za Zhi 2006;14:164-6. [PubMed]
- Weng JP, Bi Y. Epidemiological Status of Chronic Diabetic Complications in China. Chin Med J (Engl) 2015;128:3267-9. [Crossref] [PubMed]
- Tuck M. Microvascular complications of diabetes: the role of angiotensin converting enzyme inhibitors Proceedings of a Round Table Meeting, June 1999, San Diego, USA. Available online: https://onlinelibrary.wiley.com/doi/pdf/10.1002/pdi.133
- Phillips P, Wilson D, Beilby J, et al. Diabetes complications and risk factors in an Australian population. How well are they managed? Int J Epidemiol 1998;27:853-9. [Crossref] [PubMed]
- Hosseini MS, Rostami Z, Saadat A, et al. Anemia and microvascular complications in patients with type 2 diabetes mellitus. Nephrourol Mon 2014;6:e19976. [Crossref] [PubMed]
- Santos AL, Cecílio HP, Teston EF, et al. Microvascular complications in type 2 diabetes and associated factors: a telephone survey of self-reported morbidity. Cien Saude Colet 2015;20:761-70. [Crossref] [PubMed]
- Tracey ML, McHugh SM, Fitzgerald AP, et al. Risk Factors for Macro- and Microvascular Complications among Older Adults with Diagnosed Type 2 Diabetes: Findings from The Irish Longitudinal Study on Ageing. J Diabetes Res 2016;2016:5975903. [Crossref] [PubMed]
- Liu Z, Fu C, Wang W, et al. Prevalence of chronic complications of type 2 diabetes mellitus in outpatients - a cross-sectional hospital based survey in urban China. Health Qual Life Outcomes 2010;8:62. [Crossref] [PubMed]
- Hurst C, Thinkhamrop B, Tran HT. The Association between Hypertension Comorbidity and Microvascular Complications in Type 2 Diabetes Patients: A Nationwide Cross-Sectional Study in Thailand. Diabetes Metab J 2015;39:395-404. [Crossref] [PubMed]
- Zhang B, Xiang HD, Mao WB, et al. Epidemiological analysis of chronic diabetic complications and related macrovascular diseases in hospitalized patients with type 2 diabetes in Beijing, Shanghai, Tianjin and Chongqing. Chin Med Sci J 2002;24:452-6.
- Khanam PA, Hoque S, Begum T, et al. Microvascular complications and their associated risk factors in type 2 diabetes mellitus. Diabetes Metab Syndr 2017;11 Suppl 2:S577-S581. [Crossref]
- Misra A, Kumar S, Kishore Vikram N, et al. The role of lipids in the development of diabetic microvascular complications: implications for therapy. Am J Cardiovasc Drugs 2003;3:325-38. [Crossref] [PubMed]
- Won JC, Kwon HS, Kim CH, et al. Prevalence and clinical characteristics of diabetic peripheral neuropathy in hospital patients with Type 2 diabetes in Korea. Diabet Med 2012;29:e290-6. [Crossref] [PubMed]
- Agrawal RP, Ola V, Bishnoi P, et al. Prevalence of micro and macrovascular complications and their risk factors in type-2 diabetes mellitus. J Assoc Physicians India 2014;62:504-8. [PubMed]
- Pradeepa R, Anjana RM, Unnikrishnan R, et al. Risk factors for microvascular complications of diabetes among South Indian subjects with type 2 diabetes--the Chennai Urban Rural Epidemiology Study (CURES) Eye Study-5. Diabetes Technol Ther 2010;12:755-61. [Crossref] [PubMed]
- Bansal D, Gudala K, Esam HP, et al. Microvascular Complications and Their Associated Risk Factors in Newly Diagnosed Type 2 Diabetes Mellitus Patients. Int J Chronic Dis 2014;2014:201423. [Crossref] [PubMed]
- Maghbooli Z, Pasalar P, Keshtkar A, et al. Predictive factors of diabetic complications: a possible link between family history of diabetes and diabetic retinopathy. J Diabetes Metab Disord 2014;13:55. [Crossref] [PubMed]
- Nakhanakhup C, Moungmee P, Appell HJ, et al. Regular physical exercise in patients with type II diabetes mellitus. Eur Rev Aging Phys Act 2006;3:10-19. [Crossref]
- Kung K, Chow KM, Hui EM, et al. Prevalence of complications among Chinese diabetic patients in urban primary care clinics: a cross-sectional study. BMC Fam Pract 2014;15:8. [Crossref] [PubMed]
- Shera AS, Jawad F, Maqsood A, et al. Prevalence of chronic complications and associated factors in type 2 diabetes. J Pak Med Assoc 2004;54:54-9. [PubMed]
- Liu L, Wu X, Liu L, et al. Prevalence of diabetic retinopathy in mainland China: a meta-analysis. PLoS One 2012;7:e45264. [Crossref] [PubMed]
- Yang H, Young D, Gao J, et al. Are blood lipids associated with microvascular complications among type 2 diabetes mellitus patients? A cross-sectional study in Shanghai, China. Lipids Health Dis 2019;18:18. [Crossref] [PubMed]


