
Chin-down-plus-larynx-tightening maneuver improves choking cough after esophageal cancer surgery
Introduction
The recurrent laryngeal nerve (RLN) lymph node (LN) is considered a common metastatic site in esophageal cancer (1). RLN LNs are described as regional LNs in the Union for International Cancer Control (UICC) TNM Classification 7th edition. Dissection of these LNs is beneficial for determining the prognosis of esophageal cancer. RLN LN dissection causes RLN injuries and sectioning in 9–50% of cases (2-6). Hoarseness, choking cough, stridor, aspiration pneumonia, or even dyspnea may occur following RLN injuries. Some patients experience a post-operative choking cough while eating or drinking along with related dysphagia, even though the RLN does not innervate the muscles involved in swallowing (7).
Semi-liquid diets or soft foods are required for patients with a choking cough while eating or drinking after esophageal resection. Enteral nutrition via a naso-intestinal tube or feeding jejunostomy tube can be provided if necessary. The quality of life for patients is greatly impaired until oral feeding becomes possible.
Gould et al. found that RLN injuries produced kinematic changes in the tongue, epiglottis, larynx, posterior tongue ratio, and relative timing of various muscle complexes, leading to a choking cough (8); at some specific times, the choking cough disappeared.
Kumai et al. studied patients who had normal swallowing function after an esophagectomy and found that the chin-down maneuver significantly increased the pharyngeal constriction ratio, upper esophageal sphincter opening diameter, duration of upper esophageal sphincter opening, and duration of laryngeal vestibule closure (9). In addition, the chin-down maneuver increased glottal closure, epiglottis folding (10), epiglottis movement distance, and the angle between the mandible and posterior laryngeal wall, while decreasing liquid aspiration (11).
We hypothesized that changes in the head or body position might affect the phase of swallowing and improve swallowing abnormalities in patients with RLN injuries after an esophagectomy. In this study, we used the chin-down-plus-larynx-tightening maneuver and studied its effects in patients with a choking cough.
Methods
This was a prospective, one-arm, single-center study.
Patients
This study comprised 62 patients with thoracic esophageal squamous cell carcinoma treated at our hospital from April 2014 to May 2016. The study protocol was approved by the Ethics Committee of the Affiliated Cancer Hospital of Zhengzhou University (2014ys38), and written consent was obtained from each patient. All the clinical and pathological data were collected from the LinkDoc database. All the participants presented with at least 1 of the following 3 symptoms after the radical operation: choking cough, hoarseness, and vocal cord paralysis. Enhanced computed tomography (CT) scans of the chest and upper abdomen, ultrasound scans of the heart, abdomen and neck, routine blood tests, and liver and kidney function tests were performed pre-operatively. An open approach or minimally invasive esophagectomy (MIE) was conducted through a left or right thoracic approach. The left and right RLN and the subcarinal, upper, middle and lower para-esophageal, paracardial and left gastric artery LNs were thoroughly dissected (two-field lymphadenectomy). The tight RLN and upper para-esophageal LNs were preserved when a left thoracic approach was used. Three-field lymphadenectomy was not performed in these patients. Manual double-layer anastomosis was performed. We described this procedure in a previous publication (12).
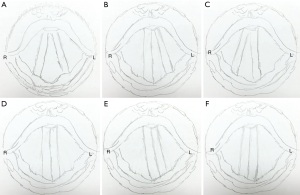
After March 13th, 2016, laryngoscopy was added to examine the vocal cord movements 1 day post-operatively. Complete compensation was defined as complete glottal closure following compensation by contralateral vocal cord movement after unilateral vocal cord fixation, and incomplete glottal closure was defined as incomplete compensation. Central fixation was confirmed when the vocal cords remained adductive, and abduction fixation was confirmed when the vocal cords remained abducent (Figure 1).
Definition of choking cough
We defined a choking cough as a cough that occurred immediately when patients began drinking.
Degree of relief
Degrees of relief were defined as follows: complete relief, numerous swallows with no choking cough after applying this maneuver; no relief, a choking cough during the first two swallows; partial relief, numerous swallows with occasional occurrence of a choking cough.
Chin-down-plus-larynx-tightening maneuver
A previous clinical study described the chin-down posture (9), but the angle is smaller than that used in our study, so we refer to the maneuver in the present study as the “chin-down-plus-larynx-tightening maneuver”. In a chin-down position, the head is held, and the chin is moved as close as possible to the sternum; meanwhile, the larynx is tightened. When the chin is down as much as possible, all the muscles around the larynx are tightened toward the back (Figure 2, the direction of the white arrow).
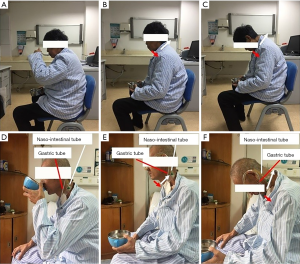
One day after the operation, each participant was directed to hold 1 mL of warm water in their mouth, move the chin as close to the sternum as possible, tighten the larynx, and then swallow the water (Figure 2). Individuals were allowed to drink more water and increase intake to the normal pre-operative level gradually if this novel maneuver completely relieved their choking cough. This maneuver was repeated for every swallow until the patients could swallow naturally.
Taniyama reported that the mean and median times of improvement of hoarseness were 103.5 and 92.5 days (5). Our study planned to advise patients to try natural position swallowing at 3 months; however, results in follow-up revealed that patients occasionally forgot the new maneuver. If choking occurred again, they would remember this maneuver. If no choking occurred after 1 “occasional forgetting”, they began natural position swallowing. The mean time taken to achieve natural swallowing was 58.6 [5–120] days. The chin-down-plus-larynx-tightening maneuver was terminated if the choking cough did not improve.
Statistical analysis
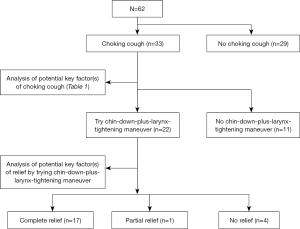
A chi-square test was used to analyze the correlation between having a choking cough and clinical factors. A chi-square test or Fisher’s exact test was used to analyze the correlation between the effectiveness of the chin-down-plus-larynx-tightening maneuver and clinical factors. Univariate regression analysis was used to analyze the effect of various factors on a choking cough, and factors with a value of P<0.2 were further analyzed by multivariate regression analysis. Because incomplete glottal closure is likely to cause a choking cough, we further analyzed vocal cord compensation using multivariate regression analysis. The flow chart is shown in Figure 3.

Full table
Results
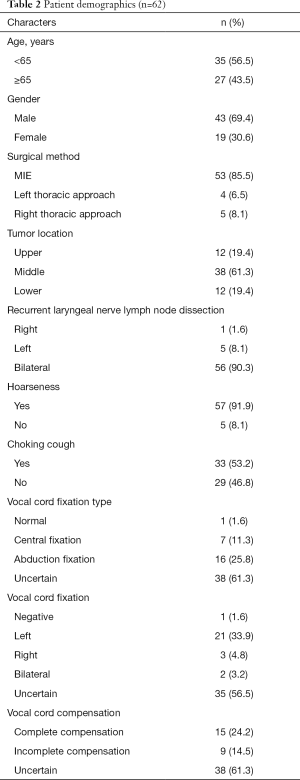
The study comprised 62 patients with resectable thoracic esophageal cancer who presented with a choking cough, hoarseness, or vocal cord paralysis after a radical operation. As shown in Table 2, 33 patients complained of a choking cough, 30 patients presented with choking cough and hoarseness, 27 patients presented with hoarseness but without choking cough, and 3 patients presented with choking cough but without hoarseness. Because laryngoscopy was added on March 13th, 2016, laryngoscopy was performed in only 27 patients.
Full table
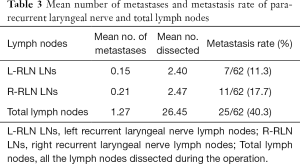
Seven patients exhibited left RLN LN metastasis (7/62, 11.3%), while the rate of right RLN LN metastasis was 11/62 (17.7%), and the total metastasis rate was 25/62 (40.3%). The mean number of metastases and mean number of LNs dissected were 0.15 and 0.21 for the left RLN respectively, and 2.4 and 2.47 for the right RLN respectively (Table 3).
Full table
Univariate and multivariate regression analyses found no independent risk factors associated with a choking cough (Table 1).
The choking cough was completely relieved in 17 of 22 (77.3%) patients, was partially relieved in 1 (4.5%) patient, and was not relieved in 4 (18.2%) patients. Fifteen of 19 (78.9%) patients who had both a choking cough and hoarseness, and 2 of 3 patients who only had a choking cough, reported complete choking cough relief.
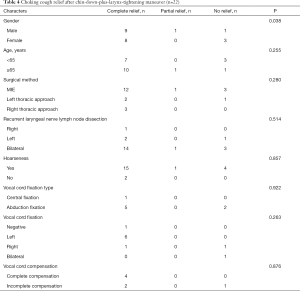
The chin-down-plus-larynx-tightening maneuver was more effective for males than for females in relieving a choking cough. No correlations were observed between the choking cough relief rate and age (P=0.255), surgical method (P=0.280), hoarseness (P=0.857), vocal cord fixation type (P=0.922), vocal cord fixation (P=0.263), or vocal cord compensation (P=0.876) (Table 4).
Full table
One important consideration is the length of time the patients had to use this position to eat or drink. Only 17 patients attempted this novel maneuver; therefore, only 17 datasets were collected by telephone. On average, the patients performed the maneuver for 58.6 [5–120] days before they were able to eat or drink in a natural position; the median time was 60 days. One patient recovered 5 days after his first attempt, while 1 recovered after 120 days.
Discussion
This study demonstrated that post-operative choking cough was not related to hoarseness or glottal closure in esophageal cancer patients who underwent esophagectomy. No independent risk factors were associated with a choking cough. The chin-down-plus-larynx-tightening maneuver significantly relieved the choking cough.
The LN metastasis rates of the left and right RLN LNs were 7/62 (11.3%) and 11/62 (17.7%), respectively, in our study. Thus, it is necessary for thoracic surgeons to dissect these LNs near the RLN. However, the drawback of this approach is that the risk of RLN injures is increased.
We found that 27 of 57 (47.3%) patients who were experiencing hoarseness did not have a choking cough, while 3 of 5 non-hoarse patients had a choking cough. No relationship was found between hoarseness and choking cough occurrence (P=0.752). A post-operative choking cough indicated the failure of airway protection or changes in the swallowing phases. Neurophysiological studies demonstrate that the RLN innervates most of the intrinsic muscles of the larynx (7); it is likely that the RLN does not directly regulate swallowing.
Our results showed no correlation between choking cough and glottal closure (P=0.876). After RLN injuries, the glottis was completely closed when the bilateral vocal cord was centrally fixed or the unilateral vocal cord was centrally fixed with contralateral vocal fold complete compensation. Among the 15 patients with complete vocal fold compensation, 5 patients presented with a choking cough. Clinical studies have revealed that RLN paralysis increases the risk of aspiration (2-4,6), suggesting that the RLN is involved in airway protection. Researchers have proposed that RLN injuries cause vocal cord paralysis, and then food or water enter the trachea because the glottis is open, leading to a choking cough (7). However, not all food or water in the superior glottis enters the trachea. Another study found that the aspiration rate 48 hours after RLN injuries was significantly higher than that immediately after RLN injuries. We observed that the status of the glottis may not explain the occurrence of aspiration. Therefore, opening and closing the glottis is not the only factor affecting the occurrence of a choking cough.
We conducted a multivariate regression analysis of choking coughs and found that gender, vocal cord fixation, and vocal cord compensation were not independent risk factors associated with having a choking cough, further suggesting that coughing is a complicated process that requires coordination of multiple structures.
Our study showed that the choking cough was completely relieved in 17 of 22 (77.3%) patients and partially relieved in 1 (4.5%) patient by the chin-down-plus-larynx-tightening maneuver. Thus, this posture change affected the post-operative choking cough. Rasley et al. found that the chin-down maneuver significantly reduced aspiration in 69% of patients (11). Ertekin also revealed that head and neck positions improved dysphagia in 50% of patients (13). The chin-down maneuver appears to change the relative motion between the laryngeal muscles that perform swallowing, and the timing of swallowing (8). In this study, we hypothesized that the chin-down-plus-larynx-tightening maneuver would change the states of the muscles that perform swallowing, replacing the post-operative timing with a new relative timing that leads to safe swallowing through the esophageal opening.
Interestingly, we found that the chin-down-plus-larynx-tightening maneuver was more effective for males than for females in relieving a choking cough (P=0.038). The different structure of the thyroid cartilage between males and females may be the anatomical factor accounting for this difference. This finding is also most likely a result of the stronger muscles in males that are more effective for muscle interaction and coordination, and the related compensation of those related muscles being more effective in males.
A previous study indicated that swallowing recovery in children after RLN injuries did not directly parallel the return of vocal fold mobility (14). Based on these results, we hypothesized that there is no relationship between a choking cough and hoarseness, and the relative phase of various muscle complexes is likely changed after RLN injuries.
A clinical study demonstrated that patients with stroke, acquired brain injuries, or intracranial hemorrhage had dysphagia, and the head-turn-plus-chin-down maneuver significantly reduced vallecular residue in these patients (15). Chin-down positioning also improved dysphagia in patients with Parkinson’s disease (16). Thus, it is possible that central nervous system disorders decrease neural control of swallowing and thereby change the phases of swallowing. In this sense, head-turn-plus-chin-down maneuver regulates swallow timing to achieve safe swallowing.
In our study, 9 patients were treated with an open approach, and 7 patients presented with a choking cough. This incidence rate seems very high, because we did not select all patients with esophageal cancer but only those who presented with at least 1 of the following 3 symptoms after radical surgery was included: choking cough, hoarseness, or vocal cord paralysis. The exact incidence of choking cough when using the open approach is unknown. In the MIE approach, surgeons can see the RLN clearly, and nerve injuries are decreased. This fact may account for the high incidence of choking cough to some degree.
One patient with hoarseness and a choking cough recovered at 5 days; her hoarseness may have been a sequela of orotracheal intubation. When the hoarseness disappeared, choking cough was not observed. Most likely, intubation is one of the factors that induces a choking cough or hoarseness; regardless, the novel maneuver could improve choking cough in these patients. This maneuver is meaningful and important for not only early oral feeding but also enhanced recovery after surgery (ERAS).
Based on the average day that normal swallowing occurred, we recommend that patients begin swallowing with a natural position 60 days after first using the novel maneuver.
There are some limitations of this study. First, the study was limited by the relatively small patient number; not all the participants underwent post-operative laryngoscopy. Second, laryngoscopy was not performed in patients whose choking cough was relieved spontaneously; thus, the relationship between vocal cord paralysis recovery and choking cough was not further investigated. Third, bronchoscopy or X-ray examinations were not conducted to determine whether penetration or aspiration that occurred after the choking cough were relieved. Further research is needed to investigate the mechanism by which posture changes affect post-operative choking cough. First, we will analyze pharyngeal constriction, the upper esophageal sphincter, and glottal closure and opening status in choking cough patients after using the chin-down-plus-larynx-tightening maneuver. Second, we will acquire pre-, intra-, and post-operative electroencephalograms to study the relationship of electroencephalogram parameters and the occurrence of a choking cough with the role of information integration of the central nervous system.
Conclusions
No correlations were found between a post-operative choking cough and hoarseness or glottal closure. The chin-down-plus-larynx-tightening maneuver significantly relieves choking cough and improves patient quality of life. The possible mechanism of this novel maneuver may be that it remodels the phases of muscles related to safe swallowing, while changes in the upper esophageal sphincter that accompany the chin-down posture provide favorable conditions for safe swallowing.
Acknowledgments
The authors would like to thank AME, for their language advice.
Funding: CAMS Innovation Fund for Medical Sciences (CIFMS), 2018-I2M-3-003.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study protocol was approved by the Ethics Committee of the Affiliated Cancer Hospital of Zhengzhou University (2014ys38), and written consent was obtained from each patient. The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
References
- Rice TW, Blackstone EH, Rusch VW. 7th edition of the AJCC Cancer Staging Manual: esophagus and esophagogastric junction. Ann Surg Oncol 2010;17:1721-4.
- Gockel I, Kneist W, Keilmann A, et al. Recurrent laryngeal nerve paralysis (RLNP) following esophagectomy for carcinoma. Eur J Surg Oncol 2005;31:277-81. [Crossref] [PubMed]
- Hulscher JB, van Sandick JW, Devriese PP, et al. Vocal cord paralysis after subtotal oesophagectomy. Br J Surg 1999;86:1583-7. [Crossref] [PubMed]
- Baba M, Natsugoe S, Shimada M, et al. Does hoarseness of voice from recurrent nerve paralysis after esophagectomy for carcinoma influence patient quality of life? J Am Coll Surg 1999;188:231-6. [Crossref] [PubMed]
- Taniyama Y, Miyata G, Kamei T, et al. Complications following recurrent laryngeal nerve lymph node dissection in oesophageal cancer surgery. Interact Cardiovasc Thorac Surg 2015;20:41-6. [Crossref] [PubMed]
- Pertl L, Zacherl J, Mancusi G, et al. High risk of unilateral recurrent laryngeal nerve paralysis after esophagectomy using cervical anastomosis. Eur Arch Otorhinolaryngol 2011;268:1605-10. [Crossref] [PubMed]
- Gould FD, Lammers AR, Ohlemacher J, et al. The Physiologic Impact of Unilateral Recurrent Laryngeal Nerve (RLN) Lesion on Infant Oropharyngeal and Esophageal Performance. Dysphagia 2015;30:714-22. [Crossref] [PubMed]
- Gould FD, Ohlemacher J, Lammers AR, et al. Central nervous system integration of sensorimotor signals in oral and pharyngeal structures: oropharyngeal kinematics response to recurrent laryngeal nerve lesion. J Appl Physiol (1985) 2016;120:495-502. [Crossref] [PubMed]
- Kumai Y, Yoshida N, Kamenosono Y, et al. Effects of chin-down maneuver on the parameters of swallowing function following esophagectomy with three-field lymphadenectomy examined by videofluoroscopy. Arch Phys Med Rehabil 2017;98:1174-9. [Crossref] [PubMed]
- Ekberg O. Posture of the head and pharyngeal swallowing. Acta Radiol Diagn (Stockh) 1986;27:691-6. [Crossref] [PubMed]
- Rasley A, Logemann JA, Kahrilas PJ, et al. Prevention of barium aspiration during video fluoroscopic swallowing studies: value of change in posture. AJR Am J Roentgenol 1993;160:1005-9. [Crossref] [PubMed]
- Zheng Y, Li Y, Wang Z, et al. A video demonstration of the Li's anastomosis-the key part of the "non-tube no fasting" fast track program for resectable esophageal carcinoma. J Thorac Dis 2015;7:1264-8. [PubMed]
- Ertekin C, Keskin A, Kiylioglu N, et al. The effect of head and neck positions on oropharyngeal swallowing: a clinical and electrophysiologic study. Arch Phys Med Rehabil 2001;82:1255-60. [Crossref] [PubMed]
- Tibbetts KM, Wu D, Hsu JV, et al. Etiology and long-term functional swallow outcomes in pediatric unilateral vocal fold immobility. Int J Pediatr Otorhinolaryngol 2016;88:179-83. [Crossref] [PubMed]
- Nagy A, Peladeau-Pigeon M, Valenzano TJ, et al. The effectiveness of the head-turn-plus-chin-down maneuver for eliminating vallecular residue. Codas 2016;28:113-7. [Crossref] [PubMed]
- Ayres A, Jotz GP, Rieder CR, et al. Benefit from the Chin-Down Maneuver in the Swallowing Performance and Self-Perception of Parkinson's Disease Patients. Parkinsons Dis 2017;2017:7460343. [Crossref] [PubMed]


