
Stereoacuity measurement using an auto-stereoscopic smartphone
Introduction
Measuring stereoacuity is a standard ophthalmic examination in the clinic, and a variety of instruments is used to evaluate it; however, most of them are printed. Commonly used clinically include the Frisby stereotest (Stereotest Ltd, Sheffield, UK), which conduct in real space (1,2); TNO stereo test (Lameris Ootech BV, Ede, Netherlands) (3,4), which should wearing red-green glasses to separate binocular; Titmus stereo test (Stereo Optical Company, Inc. Illinois, USA) (5,6), a pair of polarizing glasses is needed to separate two eyes; Lang stereotest (Lang-Stereotest AG, Kusnacht, Switzerland) (7), using a naked eye 3D technique, applied as a screen tool. With the development of information technology, 3D expression in the video domain becomes more and more mature. Watching a 3D movie, which usually uses the polarizing technique, or playing a 3D video game, which usually uses the shuttle glasses technique, is an ordinary form of entertainment. Theoretically, a successful 3D express mode can also be used to evaluate stereopsis because of the fundamentals of a 3D display or that stereopsis measurement is all based on disparity. Some researchers have done studies in this field (8,9). The size of a minimum display unit of the modern monitor, e.g., liquid crystal display (LCD), is a limitation comparing to traditional printed technique. However, the test distance is sometimes set at a relatively distant place to offset the deficiency. For a standard 17.3" 16:9 full HD (1920×1080 pixels) 3D laptop, the display density of the screen is 130 PPI (pixels per inch). At a routine checking distance of 40 cm, a pixel disparity approximately equal to 100 arc second (arcsec,”). The accuracy may only act as a coarse screen tool. The situation has been improved with the springing up of high-resolution smartphones, especially with the progression of naked eye 3D technology. For the naked eye 3D glasses-free mobile phone equipped with a 6 inch 2K (2560×1440 pixels) screen, display density is 490 PPI. A pixel disparity approximately equal to 27” at 40cm. Limited by the parallax barrier technology of auto-stereoscopic display, the minimum disparity would be twice of the physical pixels of the screen. Therefore, the test threshold was 54” at 40 cm. The threshold of the value is better than some measurement tools used in the clinic, such as Lang stereotest (threshold value 200”), PASS Test 3 (Vision Assessment Corporation, Illinois, USA, threshold value 60”), TNO stereo Test (19 edition, threshold value 60”), When prolonged the checking distance to 54 mm, the test threshold value of the 3D smartphone would reach 40”, which meet the standard of Titmus stereo test (threshold value 40”) or Dinosaur Stereoacuity Test (Bernell, a Division of Vision Training Products, inc. Indiana, USA; threshold value 40”).
Whether it is possible to make a naked eye 3D smartphone acting as an evaluation tool to measure stereopsis? After all, there are apparent advantages of a smartphone, such as glasses-free, portable, capaciousness, etc., to be a checking instrument. We imitated two quantitative measurements [Random Dot Stereo Acuity Test (Vision Assessment Corporation, Illinois, USA), representing contour based test symbol; Random Dot 3 Stereo Acuity Test (Vision Assessment Corporation, Illinois, USA), representing random dot based test symbol] with a naked eye 3D smartphone to explore the possibility.
Methods
Subjects
A total of 60 subjects, aged 20 to 35 years, whose stereoacuity was at least 160” as evaluated by the Fly Stereo Acuity test, were enrolled. The study was conducted at the Second Hospital of Jilin University in China. The research protocol followed the tenets of the Declaration of Helsinki and was approved by the ethics committee of the Second Hospital of Jilin University (No. 2017-89).
Smartphone and comparison tests
A naked eye 3D glasses-free PPTV King7s mobile phone (Shanghai Gallop Entertainment Media Technology Co., Ltd. China) is equipped with a 6 inch IPS screen which the display resolution is 2560×1440 pixels. The display density of the screen is 490 PPI. At a routine checking distance of 40 cm, 2-pixel disparity approximately equal to 54”. When changing checking distance, the testing threshold would be changed.
Page 2 (Section B) of Random Dot Stereo Acuity Test, which including 12 levels of disparity, was chosen as comparison with contour based stereo test; Page 2 (Section A) of Random Dot 3 Stereo Acuity Test, which including 10 levels of disparity, was chosen as comparison with random dot based stereo test.
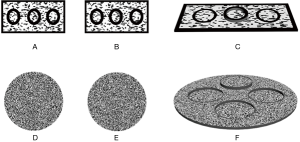
A device equipped with slide-rail was used to hold the test materials (Figure 1). For Random Dot Stereo Acuity Test and Random Dot 3 Stereo Acuity Test, the test page was fixed at 40 cm. For naked eye 3D smartphone tests, three test pages were set to imitate Random Dot Stereo Acuity Test (page 1: 400”, 160” and 40”; page 2: 200”, 100” and 50”; page 3: 63” and 32”) and Random Dot 3 Stereo Acuity Test (page 1: 160” and 40” ; page 2: 100” and 50”; page 3: (63” and 32”) respectively. The checking distance of page 1 was set at 54 cm, at which 20 pixels disparities equivalent to 400”, 8 pixels equivalent to 160” and 2 pixels equivalent to 40”; the checking distance of page 2 was set at 43 cm, at which 8 pixels equivalent to 200”, 4 pixels equivalent to 100” and 2 pixels equivalent to 50” ; the checking distance of page 3 was set at 67 cm, at which 4 pixels equivalent to 63”, and 2 pixels equivalent to 32” A program was written using C# to generate all random-dot stereograms (Figure 2).
Tests procedures
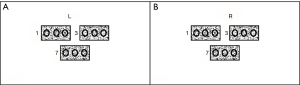
Sixty participants were divided into two groups equally. Thirty people were tested with Random Dot Stereo Acuity Test, and another 30 people were tested with Random Dot 3 Stereo Acuity Test. For naked eye 3D smartphone test, the examination began with page 1 at 54 cm, and then page 2 at 43 cm, and then page 3 at 67 cm. At the beginning of the test, the head position of the subject, or the position of the smartphone should be calibrated. Letter “R” and “L” were displayed on the screen, which could not be seen by a single eye at the same time (Figure 3). That is if the right eye can see “R”, “L” cannot be seen; if the left eye can see “L”, “R” cannot be seen. Before the formal test started, the subject should close the left eye and open the right eye. “R” shown on the screen should be seen on the screen, otherwise, adjust the position of the smartphone slightly and “R” could be seen. Hold the position and open both eyes during the test procedure, and crossed disparity was appeared in all test graphs.
For routine Random Dot Stereo Acuity Test and Random Dot 3 Stereo Acuity Test, the test terminal point was set at 32” in order to correspond to an auto-stereoscopic smartphone.
Statistical analysis
MedCalc Statistical Software (version 17.6, MedCalc Software bvba, Ostend, Belgium) was used to process all data. The Wilcoxon signed rank test was used to test the difference between the groups. Stereoacuity values were transformed to log arcsec for analysis. The Bland-Altman method was used to evaluate the agreement between the two tests.
Results
Random Dot Stereo Acuity Test vs. auto-stereoscopic smartphone: No significant difference was found between Random Dot Stereo Acuity Test and auto-stereoscopic smartphone (Wilcoxon test, paired samples: P=0.156). The mean stereoacuity measured by Random Dot Stereo Acuity Test was 1.61±0.19 log arcsec, compared with 1.60±0.17 log arcsec measured using an auto-stereoscopic smartphone. The 95% LoA was −0.09 to 0.12 log arcsec. The maximum allowed difference between methods was −0.12 to 0.15 log arcsec (Figure 4A).
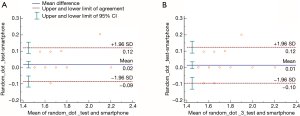
Random Dot 3 Stereo Acuity Test vs. auto-stereoscopic smartphone: No significant difference was found between Random Dot Stereo Acuity Test and auto-stereoscopic smartphone (Wilcoxon test, paired samples: P=0.219). The mean stereoacuity measured by Random Dot 3 Stereo Acuity Test was 1.61±0.18 log arcsec, compared with 1.60±0.17 log arcsec measured using an auto-stereoscopic smartphone. The 95% LoA was −0.10 to 0.12 log arcsec. The maximum allowed difference between methods was −0.13 to 0.16 log arcsec (Figure 4B).
Discussion
Traditional methods to evaluate stereopsis in the clinic are almost printed. Most of the method should divide two eyes first and then checking, except Frisby stereotest which conducted in real space. Polarizing glasses are most often used to separate binocular, such as Titmus stereo test, PASS Test 3, Randot Stereotests, Random Dot E Stereotest (Vision Assessment Corporation, Illinois, USA), Random Dot Stereo Acuity Test, et al. Red-green glasses can separate binocular, and TNO stereo test using this technique. Naked eye 3D technique can also be used to divide images, such as Lang stereotest and Dinosaur Stereoacuity Test. Although Lang stereotest and Frisby stereotest are all tested without the help of special glasses, the principle of them is different. Naked eye 3D technique should divide two eyes first, which means that the right eye sees cannot be seen by the left eye and vice versa, and the disparity setting is transversal. Frisby stereotest need not divided eyes, and the disparity setting is lengthwise.
To achieve glasses-free 3D expression, light barrier technology, cylindrical lens technology, or point light source technology usually could be utilized in a stereoscopic display. The naked eye 3D glasses-free PPTV King7s mobile phone used in this experiment adopts a light barrier, that is, parallax barrier technology (10). Optical parallax barrier technology is realized by using a switched liquid crystal screen to produce a series of vertical fringes with a direction of 90 degrees. These ultrathin vertical grating pattern, called parallax barrier, help to divide images into different eyes. In stereoscopic display mode, when the image that should be viewed by the left eye is displayed on the LCD screen, the opaque stripes will occlude the right eye. Similarly, when the image that should be seen by the right eye is displayed on the LCD screen, the opaque stripes will occlude the left eye. However, there still a problem that the display itself could achieve transfer different images to different eyes, but could not sure which image to which eye. In other words, crossed disparity or uncrossed disparity could not be determined by smartphone. To solve the issue, close one eye and make sure the suitable picture to send to the right eye at the beginning of the test is essential. Also, the head of the subject should maintain still during the whole test procedure. Another problem is that the horizontal resolution reduces by half because of the display principle of parallax barrier technology, which means 2-pixel disparity is the smallest unit of this test circumstance.
Whatever in contour based test or random dot based test, the test result of the auto-stereoscopic smartphone showed a high-level agreement with traditional test methods. Comparing with Random Dot Stereo Acuity Test, the 95% LoA was ±1.29 arcsec, and the maximum allowed difference between methods was ±1.36 arcsec. Comparing with Random Dot 3 Stereo Acuity Test, the 95% LoA was ±1.29 arcsec, and the maximum allowed the difference between methods was ±1.40 arcsec. The stereopsis value is far lower than the minimum test interval in the clinical test.
A high-resolution auto-stereoscopic smartphone can change to a useful tool to evaluate stereopsis qualitatively or quantitatively. A large number of people encountered refractive error should not wear other glasses upon their one. The researchers or doctors can create more personalized symbols, more flexible test step range, more complicated test environment, et. al. Moreover, the test instrument is portable for it just a smartphone with a standard size.
Conclusions
The auto-stereoscopic smartphone can be used as a useful quantitative tool for evaluating deficiency in stereopsis.
Acknowledgments
Funding: Jilin Provincial Science & Technology Department, China (No. 20170519004JH, No. 20190303150SF).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The research protocol followed the tenets of the Declaration of Helsinki and was approved by the ethics committee of the Second Hospital of Jilin University (No. 2017-89). The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
References
- Bohr I, Read JC. Stereoacuity with Frisby and revised FD2 stereo tests. PLoS One 2013;8:e82999. [Crossref] [PubMed]
- Costa MF, Moreira SM, Hamer RD, et al. Effects of age and optical blur on real depth stereoacuity. Ophthalmic Physiol Opt 2010;30:660-6. [Crossref] [PubMed]
- Lee JY, Seo JY, Baek SU. The effects of glasses for anisometropia on stereopsis. Am J Ophthalmol 2013;156:1261-6. [Crossref] [PubMed]
- van Doorn LL, Evans BJ, Edgar DF, et al. Manufacturer changes lead to clinically important differences between two editions of the TNOstereotest. Ophthalmic Physiol Opt 2014;34:243-9. [Crossref] [PubMed]
- Tejedor J, Ogallar C. Comparative efficacy of penalization methods in moderate to mild amblyopia. Am J Ophthalmol 2008;145:562-9. [Crossref] [PubMed]
- Arnoldi K, Frenkel A. Modification of the titmus fly test to improve accuracy. Am Orthopt J 2014;64:64-70. [Crossref] [PubMed]
- Budai A, Czigler A, Mikó-Baráth E, et al. Validation of dynamic random dot stereotests in pediatric vision screening. Graefes Arch Clin Exp Ophthalmol 2019;257:413-23. [Crossref] [PubMed]
- Kim J, Yang HK, Kim Y, et al. Distance stereotest using a 3- dimensional monitor for adult subjects. Am J Ophthalmol 2011;151:1081-6. [Crossref] [PubMed]
- Wu H, Jin H, Sun Y, et al. Evaluating stereoacuity with 3D shutter glasses technology. BMC Ophthalmol 2016;16:45. [Crossref] [PubMed]
- Lv GJ, Wang QH, Zhao WX, et al. 3D display based on parallax barrier with multiview zones. Appl Opt 2014;53:1339-42. [Crossref] [PubMed]



