
Action plan for improving cardiac rehabilitation-related outcomes in a university hospital based on a review of previous interventions
Introduction
Cardiac rehabilitation (CR) exists as an exercise-based, educational, and often multi-modal secondary prevention program for patients with cardiovascular disease (1), and it demonstrably reduces mortality rates (2,3) and hospital admissions (4,5). The 2010 American Association of Cardiovascular and Pulmonary Rehabilitation/American College of Cardiology Foundation/American Heart Association (AACVPR/ACCF/AHA) update on performance measures on CR favors referral to CR among a broad-based patient population (6). This includes those with a recent coronary artery bypass graft (CABG), revascularization procedure, or acute coronary syndrome (ACS) event as well as those with heart failure (Class I, Level of Evidence B for all populations) (6).
Methodist University Hospital (MUH) in Memphis, TN has developed and implemented multiple interventions for increasing the number of appropriate referrals to CR. This Action Plan reviews these interventions and their impact on referral rates. Based on these changes, further interventions are proposed.
Methods
MUH has key quality improvement personnel; one of their goals is to improve referral rates to CR post-ACS events. The Define, Measure, Analyze, Improve, Control (DMAIC) Project: Acute Myocardial Infarction (AMI) Transition of Care was the latest effort by MUH to improve CR referral rates. All data used in this paper was from the MUH DMAIC project database.
In the first quarter of 2018, the project initiated the early phases of its interventions. The interventions that this project included are listed in Table 1. First, the project called for the development of an improved documentation tool that allows nurses discharging CR-eligible patients to see the details of a patient’s referral. Next, a shared documentation tool to facilitate communication between case management and other hospital staff was development and initiated. With those tasks in motion, education to non-cardiology admitting physicians (e.g., rotating residents) about CR and the ACS order set that prompts CR referral was prioritized. A cardiology fellow was additionally tasked with improving compliance with order set utilization, and the chief of cardiology began working with a hospital-based quality improvement team to create performance indicators to assess compliance with use.
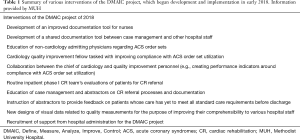
Full table
As for improving the referral process itself, the inpatient phase I CR team’s evaluation and education of patients was established as a crucial element to the referral. Case managers and abstractors were also educated about the CR referral process and the necessary documentation surrounding it. Abstractors were further instructed to provide feedback to prescribers on patients whose care did not yet meet all standard care requirements prior to discharge.
In order to promote a culture encouraging compliance with CR referrals, visual data related to the measurements of quality markers was redesigned so that hospital staff could best understand the importance of their tasks. Finally, the project team recruited support from hospital administration for the DMAIC project by providing information regarding the benefits of CR referrals.
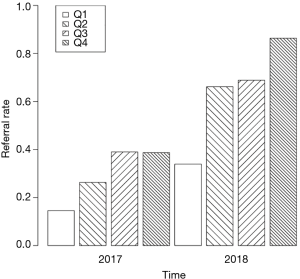
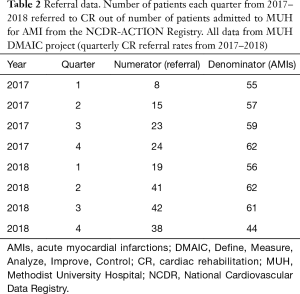
The number of referrals to CR out of total patients admitted for AMI from 2017 to 2018 were tracked quarterly via abstractors, whose data were vetted by the National Cardiovascular Data Registry (NCDR)-ACTION Registry. Bar plot of data in Figure 1 was made using R Statistical Programming Language Version 3.6.0 (7).
Results
Data from the NCDR-ACTION Registry on CR referrals from 2017–2018 are displayed in Table 2. During the first quarter (Q1) of 2017 CR referral rate was 14.5% (n=55). This rate gradually increased throughout 2017 with Q2 referral rate at 26.3% (n=57) and Q3 referral rate at 39.0% (n=59). However, there was a slight decline in the fourth quarter (Q4) of 2017 with referral rate at 38.7% (n=62). The next year referral rate continued to decline in the first quarter, but were still more than double the previous year with 2018 Q1 referral rate at 33.9% (n=56). The next three quarters of 2018 saw a continued increase in referral rates especially in comparison with the same quarter of the previous year: Q2 had rates 2.5 times higher at 66.1% (n=62), Q3 had rates 1.8 times higher at 68.9% (n=61), and Q4 had rates 2.2 times higher at 86.4% (n=44). The calculated referral rates are displayed in Figure 1.
Full table
Discussion
The above interventions have been successful at MUH with an increase in CR referral rate from 14.5% in the first quarter of 2017 to 86.4% in the fourth quarter of 2018 (Figure 1). This is a notable increase in the referral rate, especially when compared with national rates of referral. For example, in 2014, the ACTION-Get With the Guidelines registry showed 84.5% of ST-elevation myocardial infarction (STEMI) patients and 75.9% of NSTEMI patients were referred to CR (8). From 2009 to 2012, data from the NCDR showed around 60% of post-percutaneous coronary intervention (PCI) patients were referred (9). This recent increase in referral rates is likely due to the multidisciplinary targets and collaborative nature of the interventions by the DMAIC project.
Previous projects at MUH targeting referrals to CR were more exclusive in their interventions. For example, past projects focused solely on case management or solely on the inpatient CR team, rather than targeting both groups or promoting better communication between the groups and other hospital staff. With CR-referral rates as low as 14.5% in early 2017, it became clear that an interdisciplinary approach to this problem would be necessary.
Referral strategies
The interventions employed by the DMAIC project are also advantageous for referral rates and even other outcomes since they entail both automatic referrals and liaison referrals. In their review article, Gallagher and colleagues suggest that the “liaison type of referral strategy” is more educational for patients and could allow clinicians the opportunity to strongly recommend CR (10). This, in turn, could lead to an increase in participation rates after referral (10). Gravely-Witte et al. found in their review that studies examining automatic referrals achieved the highest rates of referral; studies examining a combination of liaison referral and automatic referral achieved the highest rates of enrollment (11).
The automatic referral strategy at MUH consists of non-physician staff (e.g., case managers, CR team members, etc.) verbally ordering referrals to CR by default if the physician has not done so via the ACS order set. It should be noted that this form of automatic referral is considered the last resort for ensuring a quality standard-of-care and highlights how order set utilization is an area that continues to require improvement. The liaison referral strategy at MUH consists of inpatient CR team members evaluating and educating patients regarding CR referral.
The future of the DMAIC project: interventions for improvement
Despite the overall strength of the interventions employed in 2018, various parts of the project are still underway. There are also multiple areas where additional interventions could be employed to further optimize patient referral to CR as well as improve outcomes at the outpatient CR level.
First, while the project discussed in this Action Plan entailed efforts to create a CR pathway for patients with AMI, there are other categories of patients who should be offered CR per guidelines, such as those with heart failure (6). A CR pathway for such groups of patients has yet to be well-developed by MUH.
Second, great strides remain in the education of physicians on the benefits and referral process of CR. Gallagher and colleagues show concern that physicians attend potentially non-accredited online CR-courses due to the lack of a CR-specific international governing body or a paucity of CR-specialized graduate programs (10). Thus, the creation of an accredited, online CR course could satisfy this void and fill this need. A quarterly workshop as well as the inclusion of CR-referral training in the orientation of residents, fellows, and new physicians entering the hospital system could also be helpful in educating physicians at MUH. Alternatively, noon conferences, quarterly meetings, or continuing medical education (CME) events could be used for physician education. However, these interventions come at the cost of time and patience, and knowledge may not be optimally retained. It remains important to find the optimal means of physician education.
Next, the literature has revealed and commented on the apparent drop-off that can occur between referral and subsequent enrollment to CR (12-15). While CR referrals theoretically lead to enrollment, it is important to assess the actual enrollment and participation rates at those CR programs to which that MUH refers. This data could be used to create specific interventions that will concretely affect patient mortality and hospitalization rates rather than simply treating low CR-referral numbers with no patient-related benefit.
Last, Grace and colleagues found that Canadian outpatient CR programs were unexpectedly strained due to the influx of patients after implementing successful referral strategies (16). It is very possible that the outpatient CR programs to which MUH refers are experiencing a similar burden. Assessing enrollment rates and current capacities of these programs would provide case managers with data on wait times for enrollment. This, in turn, would trigger referrals to less-overburdened programs, thus improving delays in care.
In order to optimally address the current areas for improvement in the DMAIC project, the following deliverables have been proposed:
- Creation of a preliminary protocol for referring non-AMI patients (e.g., those with heart failure) to CR;
- Development of an online CR course, accredited via the University of Tennessee Health Science Center;
- Improvement of the curriculum for hospital-based physician education to include CR;
- Preparation of educational materials for CR-training during orientations for residency and fellowship or during educational conferences;
- Tabulation of the enrollment rates, participation rates, capacities, and measures of resource strain at local outpatient CR programs.
These interventions are anticipated to allow more patients with different cardiovascular conditions to partake in a program that would be beneficial to them; they also provide an opportunity for closer relationships between hospitals and outpatient CR programs, which would also benefit patients’ care.
Conclusions
In order to optimally improve the quality of care for cardiac patients at MUH, the DMAIC project set out to improve CR-referral rates with resounding success. This was evidenced by referral rates skyrocketing past current national averages. Yet, there are still many key areas for further improvement, from inclusion of heart failure patients in the CR-referral model to increased utilization of the ACS order set. In medicine, there is sometimes a tendency to “treat numbers,” and creating tangible ways of measuring patient-based outcomes (e.g., mortality and hospitalization rates) are paramount to ensure that goals are truly being met. In other words, there should not only be a focus on CR-referral rates, but rates of CR-enrollment and participation must be evaluated as well. Through hospital team-member education and collaboration with community-based programs, the outcomes of cardiac patients can be tangibly improved. The deliverables described in this Action Plan are stepping stones in the pathway to ultimately achieving this end.
Acknowledgments
We would like to acknowledge Methodist University Hospital for the encouragement to undertake this research and create an action plan that other institutions may emulate. We would also like to acknowledge all those involved in making the DMAIC project a reality and their commitment to improving patient outcomes.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
References
- Freeman AM, Taub PR, Lo HC, et al. Intensive Cardiac Rehabilitation: an Underutilized Resource. Curr Cardiol Rep 2019;21:19. [Crossref] [PubMed]
- Heran BS, Chen JM, Ebrahim S, et al. Exercise-based cardiac rehabilitation for coronary heart disease. Cochrane Database Syst Rev 2011.CD001800. [PubMed]
- Lawler PR, Filion KB, Eisenberg MJ. Efficacy of exercise-based cardiac rehabilitation post-myocardial infarction: a systematic review and meta-analysis of randomized controlled trials. Am Heart J 2011;162:571-84.e2. [Crossref] [PubMed]
- Anderson L, Oldridge N, Thompson DR, et al. Exercise-Based Cardiac Rehabilitation for Coronary Heart Disease: Cochrane Systematic Review and Meta-Analysis. J Am Coll Cardiol 2016;67:1-12. [Crossref] [PubMed]
- Sagar VA, Davies EJ, Briscoe S, et al. Exercise-based rehabilitation for heart failure: systematic review and meta-analysis. Open Heart 2015;2:e000163. [Crossref] [PubMed]
- Thomas RJ, King M, Lui K, et al. AACVPR/ACCF/AHA 2010 update: performance measures on cardiac rehabilitation for referral to cardiac rehabilitation/secondary prevention services: a report of the American Association of Cardiovascular and Pulmonary Rehabilitation and the American College of Cardiology Foundation/American Heart Association Task Force on Performance Measures (Writing Committee to Develop Clinical Performance Measures for Cardiac Rehabilitation). Circulation 2010;122:1342-50. [Crossref] [PubMed]
- R Core Team. R: A Language and Environment for Statistical Computing. R Foundation for Statistical Computing. Vienna, Austria: 2019.
- Benjamin EJ, Blaha MJ, Chiuve SE, et al. Heart Disease and Stroke Statistics-2017 Update: A Report From the American Heart Association. Circulation 2017;135:e146-603. [Crossref] [PubMed]
- Aragam KG, Dai D, Neely ML, et al. Gaps in referral to cardiac rehabilitation of patients undergoing percutaneous coronary intervention in the United States. J Am Coll Cardiol 2015;65:2079-88. [Crossref] [PubMed]
- Gallagher R, Neubeck L, Du H, et al. Facilitating or getting in the way? The effect of clinicians' knowledge, values and beliefs on referral and participation. Eur J Prev Cardiol 2016;23:1141-50. [Crossref] [PubMed]
- Gravely-Witte S, Leung YW, Nariani R, et al. Effects of cardiac rehabilitation referral strategies on referral and enrollment rates. Nat Rev Cardiol 2010;7:87-96. [Crossref] [PubMed]
- Boyden T, Rubenfire M, Franklin B. Will increasing referral to cardiac rehabilitation improve participation? Prev Cardiol 2010;13:192-201. [Crossref] [PubMed]
- Scott LB. Referral to outpatient cardiac rehabilitation: intervention research at the patient, provider, and health system levels. Nat Clin Pract Cardiovasc Med 2008;5:671-2. [Crossref] [PubMed]
- Turk-Adawi KI, Oldridge NB, Tarima SS, et al. Cardiac rehabilitation enrollment among referred patients: patient and organizational factors. J Cardiopulm Rehabil Prev 2014;34:114-22. [Crossref] [PubMed]
- Weingarten MN, Salz KA, Thomas RJ, et al. Rates of enrollment for men and women referred to outpatient cardiac rehabilitation. J Cardiopulm Rehabil Prev 2011;31:217-22. [Crossref] [PubMed]
- Grace SL, Tan Y, Simpson C, et al. Perceptions of cardiac specialists and rehabilitation programs regarding patient access to cardiac rehabilitation and referral strategies. J Cardiopulm Rehabil Prev 2012;32:135-40. [Crossref] [PubMed]


