
Acute kidney injury and long-term renal function after partial nephrectomy—is there a true association?
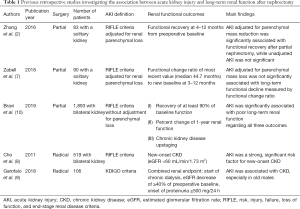
Acute kidney injury (AKI) is a common complication after partial nephrectomy with its incidence up to 54% (1,2). Nephrectomy-induced chronic renal insufficiency is associated with increased mortality (3) and a new baseline estimated glomerular filtration rate (eGFR) can impact survival after nephrectomy (4,5). As postoperative AKI is now considered to be interconnected with chronic kidney disease (CKD) (6), the AKI after nephrectomy could be also associated with the development of long-term renal functional decline and eventually CKD. However, the potential impact of AKI after partial nephrectomy on long-term renal function has been debated. There were only a few studies which investigated the impact of AKI after nephrectomy with controversy (2,7-9) (Table 1). Previous studies of radical nephrectomy reported that AKI is associated with new-onset CKD (8,9). However, the other two studies of partial nephrectomy in solitary kidneys reported no signification association between AKI determined by standard criteria with long-term renal function (2,7).
Full table
Standard criteria diagnosing AKI include RIFLE (Risk, Injury, Failure, Loss of function, End-stage kidney disease), AKIN (Acute Kidney Injury Network) and KGIDO (Kidney Disease: Improving Global Outcomes) criteria (11). However, AKI after nephrectomy is different from other surgeries because postoperative creatinine elevation could be due to both this parenchymal mass reduction and ischemic injury of the remaining renal nephrons (2,5,12). In this regard, a previous retrospective cohort study of 83 solitary kidneys managed by partial nephrectomy proposed new criteria of AKI after partial nephrectomy which uses an adjusted serum creatinine as a baseline to determine AKI. Adjusted creatinine was determined as projection creatinine value after removing the effect of parenchymal mass reduction determined by volumetric assessment of pre- and postoperative computed tomography (2). They reported a significant association between the renal functional recovery after surgery and AKI determined by their proposed criteria, while no significant association for the AKI determined by conventional criteria. However, another retrospective study which reviewed 90 solitary kidneys managed with partial nephrectomy reported no association between AKI and long-term renal functional change after partial nephrectomy even though they adjusted for parenchymal mass reduction using the same volumetric analysis in the diagnosis of AKI (7). These two studies selected only the patients with solitary kidney because it was beneficial to measure the ischemic injury. However, this could also be a limitation for the applicability of the study finding to patients with two kidneys. Also, these two studies were a small single-center retrospective study, with significant limitations in external validity.
In this regard, Bravi et al. timely published a well-implemented retrospective cohort study with a large sample size of 1,893 patients with two kidneys and undergoing partial nephrectomy (10). They defined three outcomes regarding long-term renal functional change including (I) recovery of at least 90% of baseline function one year after surgery, (II) percentage change of one-year renal function compared to baseline, and (III) CKD upstaging during one-year follow-up. AKI defined by conventional RIFLE serum creatinine criteria was associated with worse renal function one year after surgery regarding all three endpoints. These results were also confirmed by a sensitivity analysis using a different definition of AKI. Furthermore, they corroborated that longer duration of AKI is associated with increased risk of CKD upstaging by presenting a granular data of 21% absolute risk increase when the duration of AKI is ≥4 days than 1–3 days as well as cubic spline function curve. These findings are clinically relevant not only because they reported the association between AKI and long-term renal function in patients with two kidneys and undergoing partial nephrectomy in a large sample size cohort but also because their finding could enhance risk stratification of AKI on long-term renal function. As the authors correctly commented, further studies are required to establish a more sophisticated definition of AKI integrating the severity and duration of renal injury.
One limitation of this well-conducted study is the absence of renal functional evaluation longer than one year. A previous study reported an endpoint of functional change ratio which compared the most recent eGFR up to 5 years with the new baseline during 3–12 months after partial nephrectomy (7). This outcome could not be compared with the previous study. Additionally, as the previous study reported (2), evaluation of AKI on the basis of standard AKI criteria does not correct the surgical loss of parenchymal renal mass and, therefore, it could overestimate the risk or the stage of AKI after partial nephrectomy. As a result, the outcome of functional recovery measured by the ratio of % eGFR preservation to % parenchymal mass saved was not reported in this study (2). These outcomes could help readers to compare their results with previous ones. Finally, this study reviewed the series of partial nephrectomy over a long period of time of almost 30 years, which could limit the validity of their data because perioperative patient care including anesthesia technique and surgical procedure has evolved.
This study calls for further prospective trials to confirm the causal relationship between AKI and long-term renal dysfunction. However, despite these limitations, this study provided an important demise which the following studies should investigate—we should avoid or attenuate the risk of AKI to prevent or mitigate long-term renal functional decline after partial nephrectomy. How can we decrease the incidence of AKI? First of all, the surgical factor would be of utmost importance. Surgeon’s experience and skill may affect the renal outcomes (13). Ischemic renal injury seems to be the main pathophysiology of AKI. However, other modifiable etiology should be also evaluated. Although functional recovery after partial nephrectomy is mainly determined by parenchymal volume preservation (14), ischemic insult of the remaining kidney could also affect the functional outcome if ischemic time is prolonged. Efforts have been made to reduce the remaining renal parenchymal injury after partial nephrectomy. The effects of pharmacologic agents, such as mannitol and dopamine have been questioned (15,16). Renal ischemic time (1,17,18) and cold ischemia are regarded as a modifiable factor to reduce renal injury despite existing controversy (4,5,19). Cold ischemia is known to be effective in restoring renal function after partial nephrectomy (20). Zero ischemia partial nephrectomy or selective arterial clamping has been suggested (21,22). Remote ischemic conditioning using transient limb ischemia was suggested to reduce short-term renal functional impairment after laparoscopic partial nephrectomy (23). Hydrogen sulfide was effective to attenuate prolonged warm renal ischemia-reperfusion injury in a previous animal study (24). However, these measures are of only potential benefit and further clinical trials are strongly warranted.
In summary, the significant impact of AKI after partial nephrectomy on long-term renal functional decline or CKD was reported in a large retrospective study by Bravi et al. The clinical relevance of this association calls for further prospective clinical trials to confirm the causal relationship and to evaluate any interventions to mitigate the risk of AKI to prevent long-term renal functional deterioration after partial nephrectomy.
Acknowledgments
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
References
- Rajan S, Babazade R, Govindarajan SR, et al. Perioperative factors associated with acute kidney injury after partial nephrectomy. Br J Anaesth 2016;116:70-6. [Crossref] [PubMed]
- Zhang Z, Zhao J, Dong W, et al. Acute Kidney Injury after Partial Nephrectomy: Role of Parenchymal Mass Reduction and Ischemia and Impact on Subsequent Functional Recovery. Eur Urol 2016;69:745-52. [Crossref] [PubMed]
- Weight CJ, Larson BT, Fergany AF, et al. Nephrectomy induced chronic renal insufficiency is associated with increased risk of cardiovascular death and death from any cause in patients with localized cT1b renal masses. J Urol 2010;183:1317-23. [Crossref] [PubMed]
- Lane BR, Russo P, Uzzo RG, et al. Comparison of cold and warm ischemia during partial nephrectomy in 660 solitary kidneys reveals predominant role of nonmodifiable factors in determining ultimate renal function. J Urol 2011;185:421-7. [Crossref] [PubMed]
- Mir MC, Ercole C, Takagi T, et al. Decline in renal function after partial nephrectomy: etiology and prevention. J Urol 2015;193:1889-98. [Crossref] [PubMed]
- Chawla LS, Eggers PW, Star RA, et al. Acute kidney injury and chronic kidney disease as interconnected syndromes. N Engl J Med 2014;371:58-66. [Crossref] [PubMed]
- Zabell J, Isharwal S, Dong W, et al. Acute Kidney Injury after Partial Nephrectomy of Solitary Kidneys: Impact on Long-Term Stability of Renal Function. J Urol 2018;200:1295-301. [Crossref] [PubMed]
- Cho A, Lee JE, Kwon GY, et al. Post-operative acute kidney injury in patients with renal cell carcinoma is a potent risk factor for new-onset chronic kidney disease after radical nephrectomy. Nephrol Dial Transplant 2011;26:3496-501. [Crossref] [PubMed]
- Garofalo C, Liberti ME, Russo D, et al. Effect of post-nephrectomy acute kidney injury on renal outcome: a retrospective long-term study. World J Urol 2018;36:59-63. [Crossref] [PubMed]
- Bravi CA, Vertosick E, Benfante N, et al. Impact of Acute Kidney Injury and Its Duration on Long-term Renal Function After Partial Nephrectomy. Eur Urol 2019;76:398-403. [Crossref] [PubMed]
- Thomas ME, Blaine C, Dawnay A, et al. The definition of acute kidney injury and its use in practice. Kidney Int 2015;87:62-73. [Crossref] [PubMed]
- Chapman D, Moore R, Klarenbach S, et al. Residual renal function after partial or radical nephrectomy for renal cell carcinoma. Can Urol Assoc J 2010;4:337-43. [Crossref] [PubMed]
- Larcher A, Muttin F, Peyronnet B, et al. The Learning Curve for Robot-assisted Partial Nephrectomy: Impact of Surgical Experience on Perioperative Outcomes. Eur Urol 2019;75:253-6. [Crossref] [PubMed]
- Mir MC, Campbell RA, Sharma N, et al. Parenchymal volume preservation and ischemia during partial nephrectomy: functional and volumetric analysis. Urology 2013;82:263-8. [Crossref] [PubMed]
- Cosentino M, Breda A, Sanguedolce F, et al. The use of mannitol in partial and live donor nephrectomy: an international survey. World J Urol 2013;31:977-82. [Crossref] [PubMed]
- O'Hara JF Jr, Hsu TH, Sprung J, et al. The effect of dopamine on renal function in solitary partial nephrectomy surgery. J Urol 2002;167:24-8. [Crossref] [PubMed]
- Porpiglia F, Renard J, Billia M, et al. Is renal warm ischemia over 30 minutes during laparoscopic partial nephrectomy possible? One-year results of a prospective study. Eur Urol 2007;52:1170-8. [Crossref] [PubMed]
- Funahashi Y, Hattori R, Yamamoto T, et al. Ischemic renal damage after nephron-sparing surgery in patients with normal contralateral kidney. Eur Urol 2009;55:209-15. [Crossref] [PubMed]
- Lee H, Song BD, Byun SS, et al. Impact of warm ischaemia time on postoperative renal function after partial nephrectomy for clinical T1 renal cell carcinoma: a propensity score-matched study. BJU Int 2018;121:46-52. [Crossref] [PubMed]
- Mir MC, Takagi T, Campbell RA, et al. Poorly functioning kidneys recover from ischemia after partial nephrectomy as well as strongly functioning kidneys. J Urol 2014;192:665-70. [Crossref] [PubMed]
- Hung AJ, Cai J, Simmons MN, et al. "Trifecta" in partial nephrectomy. J Urol 2013;189:36-42. [Crossref] [PubMed]
- Paulucci DJ, Rosen DC, Sfakianos JP, et al. Selective arterial clamping does not improve outcomes in robot-assisted partial nephrectomy: a propensity-score analysis of patients without impaired renal function. BJU Int 2017;119:430-5. [Crossref] [PubMed]
- Huang J, Chen Y, Dong B, et al. Effect of remote ischaemic preconditioning on renal protection in patients undergoing laparoscopic partial nephrectomy: a 'blinded' randomised controlled trial. BJU Int 2013;112:74-80. [Crossref] [PubMed]
- Zhu JX, Kalbfleisch M, Yang YX, et al. Detrimental effects of prolonged warm renal ischaemia-reperfusion injury are abrogated by supplemental hydrogen sulphide: an analysis using real-time intravital microscopy and polymerase chain reaction. BJU Int 2012;110:E1218-27. [Crossref] [PubMed]


