Prevalence of hypertension, diabetes, and dyslipidemia, and their additive effects on myocardial infarction and stroke: a cross-sectional study in Nanjing, China
Introduction
Noncommunicable diseases (NCDs) are one of the major health threats. They were responsible for 73.4% of deaths worldwide in 2017 (1). The number of deaths from NCDs continues to increase every year, and most of this can be attributed to cardiovascular diseases (CVDs) (1-4). In line with the global trend, the prevalence and mortality of CVDs in China are still on the rise due to rapid economic development and health transition. In 2015, the number of patients with CVDs was estimated to be 290 million, including 13 million with stroke and 11 million with ischemic heart disease (IHD) (5). Stroke has been the leading cause of death in all CVDs, followed by IHD (6,7). Both of them are the major factors for disability-adjusted life-years and consume a large amount of medical resources (8,9). Further, mortality due to IHD and stroke has increased dramatically over the past decades, with myocardial infarction (MI) playing a leading role (10,11). The aforementioned findings highlight the heavy burden of CVD-related morbidity and mortality in China.
Hypertension, diabetes, and dyslipidemia are major modifiable risk factors for CVD. The prevalence of these risk factors has increased sustainably in China, and even worse, many middle-aged people have at least two chronic diseases (12-14). The reason for disease clustering is probably mutual risk factors, such as aging, obesity, and smoking. Nevertheless, few analyses focused on common risk factors for hypertension, diabetes, and dyslipidemia. In addition, previous studies have shown that the clustering of two risk factors increases the risk of CVDs (15,16). However, limited evidence is available with regard to the relationship between multiple chronic diseases and CVDs. Therefore, a variety of chronic diseases need to be investigated in a fixed population to explore the relevant risk factors and possible interactions between different diseases. The present study aimed to identify the commonality and difference among associated risk factors for hypertension, diabetes, and dyslipidemia, and also to evaluate their additive effects on MI and stroke.
Methods
Ethical compliance
The study was approved by the Ethics Committee of the First Affiliated Hospital of Nanjing Medical University (2016-SR-242, Jiangsu Province Hospital). Written informed consents were obtained from all participants before enrollment into the study.
Study participants
The present cross-sectional study was conducted based on a secular chronic disease management project in Nanjing, the capital of Jiangsu Province located in East China. As a baseline survey, the data were collected from all residents living in Nanjing in 2017. This study adopted a multistage, stratified random cluster sampling method to select representative samples from a general population. In the first stage of sampling, 2 districts were randomly selected from 11 districts in Nanjing City using the probability proportional to size sampling method. In the second stage, two subdistricts (streets) were chosen from the aforementioned two selected districts using the simple random sampling method. In the third stage, three communities were randomly selected from each subdistrict. In the final stage, a certain number of residents aged 15 years or older were chosen from each household of the included communities using the simple random sampling method. A total of 11,036 participants completed the survey with a response rate of 95.3% and were included in the analysis.
Data collection
All eligible investigators underwent a uniform training and qualification before conducting the questionnaire survey and physical examination. Information concerning sociodemographic characteristics, lifestyle behaviors, and personal and family health history (hypertension, diabetes, dyslipidemia, MI, and stroke) was collected using a questionnaire in a face-to-face interview with each participant. In addition, a semi-quantitative food frequency questionnaire (FFQ) was used to carry out a dietary survey (17). Data on average consumption and frequency of various foods consumed in the last year were collected using the questionnaire. According to local dietary habits, the FFQ in this study consisted of 14 food categories with a 9-point scale (never, less than once per month, once to 3 times per month, once to 2 times per week, 3 to 4 times per week, 5 to 6 times per week, once per day, twice per day, and 3 times or more per day). Next, physical measurements were conducted. Participant recruitment and data collection followed strict ethical standards during each procedure.
Potential risk factors
Based on the previous evidence, smoking, drinking, family history, number of family members, education, ethnicity, salt intake, body mass index (BMI), and central obesity were selected as potential risk factors for hypertension, diabetes, and dyslipidemia (18,19).
In terms of smoking status, study participants were considered as current smokers if they reported daily smoking at present (at least one cigarette per day). Among nonsmokers, former smokers were defined as those who smoked but had quit within the previous 12 months; and never smokers were labeled as never smoking regularly. Alcohol consumption was also classified into three categories: current drinkers were those who drank more than once in the last 30 days; former drinkers were those who drank before the previous 30 days and within 12 months; and never drinkers were those who never drank in the past 12 months. If one or both of the parents had hypertension (or diabetes), the participant was considered with a family history of hypertension (or diabetes). Regarding socioeconomic factors, the education level (primary school or lower, middle school, and college or higher) and number of family members (living together for a long time) were evaluated. The dietary salt intake was calculated by multiplying the average intake by frequency according to the FFQ. Height and weight were measured indoor when the participants wore light clothing and no shoes to the nearest 0.1 cm and 0.1 kg, respectively. BMI was estimated as weight (kg) divided by height in square millimeters (m2). The waist circumference (WC) was measured as a complete cycle at the midpoint of the anterior superior iliac spine and the lower edge of the 12th rib using a fixed measurement tape (to the nearest 0.1 cm) while the participants had normal breath. Central obesity was defined as a WC of at least 90 cm in men and at least 85 cm in women (20).
Measurement and definition of hypertension, diabetes and dyslipidemia
To guarantee accuracy, participants were required to rest for at least 5 min and avoid smoking, drinking and physical exercise for at least 30 min before blood pressure (BP) measurements. Electronic sphygmomanometers were used to measure the BP of the right arm supported at heart level with sitting position for three consecutive times at 1-min interval. The average of three readings was used as a final estimate in all analysis. In addition, venous blood specimen was collected in the morning after an overnight fast at least 8 hours. Blood samples were sent to the laboratory for examination of serum glucose and total cholesterol (TC).
According to 2018 Chinese guideline for the management of hypertension, hypertension was defined as systolic BP (SBP) ≥140 mmHg, diastolic BP (DBP) ≥90 mmHg, and use of antihypertensive medicine within last 2 weeks (12). Diabetes was defined as a serum glucose ≥7.0 mmol/L in field survey or a history of diagnosed diabetes, as recommended by the American Diabetes Association (ADA) (21). The National Cholesterol Education program guidelines have defined a high concentration of TC as ≥240 mg/dL, which was defined as dyslipidemia (22). Information about the history of CVD (MI and stroke) was self-reported.
Statistical analysis
Continuous variables were reported as mean values and standard deviations. Categorical variables were presented as frequency and percentage. The chi-square and t tests were used for categorical data and continuous variables, respectively, to compare demographic characteristics between patients and normal people. Multivariable logistic regression models were used to identify the risk factors associated with hypertension, diabetes, and dyslipidemia. Additive effects among hypertension, diabetes, and dyslipidemia were estimated by first dividing data into diabetic and nondiabetic groups and then separating them into four subgroups in terms of hypertension and dyslipidemia status. Odds ratios (ORs) and 95% confidence intervals (CIs) were calculated to reflect the effects of hypertension and dyslipidemia on MI and stroke among diabetic and nondiabetic populations. Furthermore, the common factors found to be related to hypertension and dyslipidemia in the previous step were adjusted using multivariable logistic regression. The impact of diabetes in each subgroup was evaluated by comparing the prevalence of MI or stroke among diabetic and nondiabetic populations within the group. Hypertension and diabetes, hypertension and dyslipidemia, diabetes and dyslipidemia, and hypertension and dyslipidemia were sequentially included in the corresponding models to assess the effect of interactions between any two or three factors on the risk of MI or stroke. A P value less than 0.05 was considered statistically significant. All data were statistically analyzed using SAS 9.4 (SAS Institute, NC, USA).
Results
Prevalence of hypertension, diabetes, and dyslipidemia, and associated risk factors
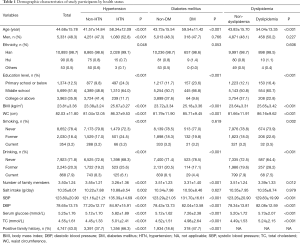
The demographic characteristics of the study population classified by hypertension, diabetes, and dyslipidemia status are summarized in Table 1. The mean values of age, BMI, WC, number of family members, serum glucose, SBP, DBP, and TC were significantly higher in participants with hypertension than in those without hypertension (P<0.001). Similar results were found when comparing diabetic population with nondiabetic population and dyslipidemia population with non-dyslipidemia population. Additionally, the proportion of male patients, patients with middle school education (P<0.001), and patients with Han ethnicity (P=0.048) was higher than that of total population. However, the daily salt intake was significantly higher only in the hypertension population (P=0.002). Besides, the percentage of patients with hypertension (or diabetes) having a positive family history of hypertension (or diabetes) was higher compared with those without hypertension (or diabetes) (P<0.001). In addition to the smoking status of patients with diabetes, the difference in alcohol consumption and smoking status between any two groups was significant (P<0.001).
Full table
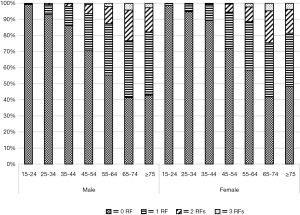
Table 2 shows the prevalence of hypertension, diabetes, and dyslipidemia stratified by sex and age. The overall prevalence rates were estimated to be 18.5% for hypertension, 6.0% for diabetes, and 8.3% for dyslipidemia. A similar pattern was observed in regard to the age trend. The prevalence of hypertension, diabetes, and dyslipidemia generally increased with age, reached a peak at the age of 65–74 years, and subsequently decreased. In particular, the prevalence of hypertension and diabetes more than doubled between 35 and 45 years while the prevalence of dyslipidemia increased fastest at the age of 25–34 years. After gender stratification, men had higher BP levels compared with women at all ages except for the first age group. However, the prevalence of diabetes and dyslipidemia was slightly higher in men than in women, mainly among middle-aged participants; it was significantly higher in women than in men for other age ranges (P<0.05). In the total population, more men suffered from hypertension compared with women, while no significant sex-related difference was found in the prevalence of diabetes and dyslipidemia. Figure 1 presents the prevalence rates for CVD risk factor clustering based on age and sex. The proportion of two or more risk factors (hypertension, diabetes, or dyslipidemia) increased with advanced age and reached the highest at the age of 65–74 years in both men (approximately 23%) and women (approximately 24%).
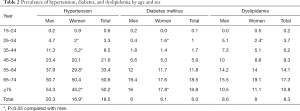
Full table
Table 3 shows the results of multivariable logistic regression models that identified risk factors for each disease. Increasing age and higher BMI were associated with increased risks of all three conditions. Moreover, the risk factors for hypertension included male sex, central obesity, smoker, former alcohol consumer, daily salt intake, and family history of hypertension; living with more family members was a protective factor. Relative to the nondiabetic population, patients with diabetes were more likely to smoke, suffer from central obesity, and have a family history of diabetes, but they were less likely to consume alcohol. Different risk factors for dyslipidemia were identified. Female participants were more likely to have dyslipidemia compared with male participants. Furthermore, a higher level of education and alcohol consumption were related to dyslipidemia.
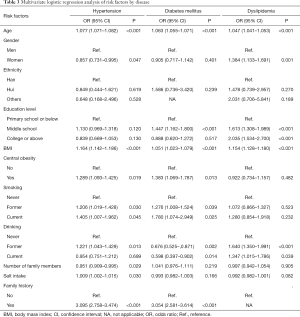
Full table
Effect of hypertension, diabetes, and dyslipidemia on stroke and MI
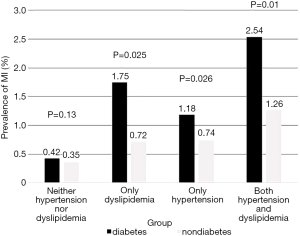
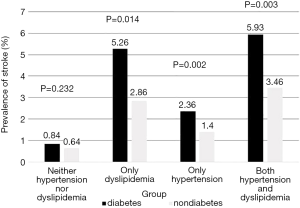
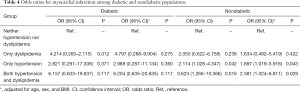
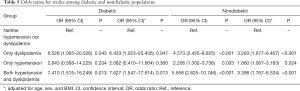
The overall prevalence of self-reported stroke and MI was 1.9% (210/11,036) and 1.0% (112/11,036), respectively. The participants were first classified into two categories according to the prevalence of diabetes and then divided into four groups. Group 1 comprised participants with neither hypertension nor dyslipidemia. Group 2 comprised participants with dyslipidemia but no hypertension. Group 3 comprised participants with hypertension but no dyslipidemia. Group 4 comprised participants with both hypertension and dyslipidemia. The prevalence of self-reported MI in Groups 1–4 in the diabetic population was 0.42%, 1.75%, 1.18%, and 2.54%, respectively. A significant decrease in prevalence was observed in the nondiabetic population except Group 1 (Figure 2). The prevalence of self-reported stroke in Groups 1–4 in the diabetic population was 0.84%, 5.26%, 2.36%, and 5.93%, respectively. Similar changes in the prevalence of MI were observed. Diabetes contributes to about twofold excess increase independently of other factors (Figure 3).
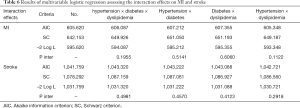
The results of univariate logistic regression that assessed which group was associated with an increased risk of MI and stroke are shown in Tables 4 and 5. In the diabetic population, the group difference showed no statistical significance with reference to the increase in the risk of MI, while Groups 2 and 4 were associated with an increased risk of stroke compared with Group 1 (reference) (OR, 6.528; 95% CI, 1.065–20.526; OR, 7.410; 95% CI, 1.515–16.249). However, a stronger association between risk factors and CVD was observed in the nondiabetic population. Each group showed an association with an increased risk of stroke, while Groups 3 and 4 showed an increased risk of MI. After adjusting for age, sex, and BMI, similar results were found.
Full table
Full table
As shown in Table 6, the test statistics and criteria of the corresponding model increased regardless of which interactive factor was added to the model, indicating that none of the interactive factors optimized the fit of the model. In addition, every interaction factor was not statistically significant (P inter >0.05). Therefore, the interaction effects on stroke or MI were not found.
Full table
Discussion
This population-based study in eastern China explored changes in the burden of major risk factors for CVD. It found that the prevalence rate was 18.5% for hypertension, 6.0% for diabetes, and 8.3% for dyslipidemia. The burden of hypertension and diabetes seemed to be lower while the prevalence of dyslipidemia was higher compared with the national epidemiological reports (23-25). Hypertension contributes the most to the population-attributable risk of stroke and is a leading risk factor for MI, especially in the elderly Chinese population (26,27). As a disorder of glucose metabolism, diabetes causes damage to multiple organ systems and confers excess risk for various vascular events (28). Therefore, hypertension and diabetes need to be controlled for preventing CVDs. Substantial efforts have been made to control the epidemic of chronic diseases. The Chinese government is committed to establish a comprehensive surveillance system with a greater emphasis on management (29). Further, in Nanjing, a new mode of cooperation between the government and tertiary hospitals has been explored and put into practice. Experts from tertiary hospitals are sent to the community to deliver regular lectures on health education and train doctors in primary health care centers so as to improve their capabilities in terms of diagnosis and treatment. Consequently, these centers provide residents with effective basic medical and public health services to improve their health literacy. Although the findings of this study indicated a substantial improvement in hypertension and diabetes, the increase in cholesterol levels cannot be ignored. Unfortunately, recent evidence shows that health care professionals and administrators have only recently begun to pay more attention to dyslipidemia (30). Moreover, the present study revealed that clustering of CVD risk factors was common among middle-aged people in both men and women. Accordingly, a more comprehensive approach to managing dyslipidemia, hypertension, and diabetes should be considered in the next stage of management.
The present study found that older age and higher BMI were associated with the development of hypertension, diabetes, and dyslipidemia, which was highly consistent with the latest findings from Korea (18). Moreover, age showed a strong association with all three diseases on comparing age-specific prevalence rates. A comparative study also indicated that higher BMI was an independent risk factor for hypertension, diabetes, and dyslipidemia in both Japan and the United States (31). Therefore, it is likely that general adiposity and aging contribute the most to the development of all three conditions in the Chinese population.
In addition, central obesity was a risk factor for hypertension and diabetes, which was consistent with numerous studies conducted in various regions of China (32-34). It has been well acknowledged that central obesity has a strong positive correlation with increased risks of incident hypertension and diabetes (35,36). Moreover, individuals with a family history of hypertension (or diabetes) have a higher likelihood of having hypertension (or diabetes) compared with those without a family history. Genetics has been recognized as an important factor in ensuring normal glucose metabolism and BP stabilization (37,38). Moreover, younger generations are likely to inherit unhealthy lifestyle and dietary habits from their parents. Therefore, individuals with a family history should be given close attention and careful surveillance. Contrary to other epidemiological studies (33,39), the present study revealed that alcohol consumption was a protective factor for diabetes. This might be because some individuals abstained from alcohol for a long time once they were diagnosed with diabetes. The behavioral transformation might benefit from health education conducted in the communities. However, no associations were found between education level and hypertension. More educated people were likely to suffer from dyslipidemia in the present study, which was contrary to the findings of previous studies (40,41). This might be because most individuals with high academic qualifications were engaged in mental work with no exercise. Interestingly, smoking was a risk factor for hypertension and diabetes, but not for dyslipidemia. This might partially be attributable to the identification of dyslipidemia based on hypercholesterolemia. Previous studies have described different relationships between the development of various dyslipidemias and smoking status. However, the finding that the effect of smoking on elevated TC was not statistically significant was consistent (25,42,43).
Another important finding of the present study was the additive effects of hypertension, diabetes, and dyslipidemia on stroke and MI. Overall, hypertension complicated with dyslipidemia conferred a more significant risk of CVD than independent effects. Compared with dyslipidemia, hypertension had stronger effects on MI and weaker effects on stroke. In addition, the cumulative effect of hypertension and dyslipidemia on MI was not significant in diabetic patients, whereas the impact on stroke was more pronounced compared with nondiabetic people. This implied that the additive effects of the three risk factors were greater on stroke than on MI, corresponding to a heavier burden of stroke than MI in China. Fortunately, both hypertension and dyslipidemia are modifiable risk factors. Long-term prospective results of a randomized trial have indicated that the interventions for controlling BP and cholesterol levels are associated with long-term benefits in terms of cardiovascular outcomes (44). Therefore, greater efforts should be made to control these risk factors as an effective strategy for preventing CVDs. Another important cardiovascular risk factor is diabetes. Its cumulative effect is significant with hypertension or dyslipidemia or both. It has been validated that insulin resistance not only leads to abnormal glucose metabolism but also causes lipid metabolism disorder (15). Moreover, patients with diabetes complicated with hypertension have an increased risk of cardiovascular events than those only with diabetes. However, a recent cohort study showed that patients with diabetes who had elevated BP and dyslipidemia within the target ranges appeared to have little or no excess risk of MI or stroke compared with the general population (45). Therefore, further studies are warranted to better understand the additional effects of risk factors on MI and stroke. Further, the interaction between the three factors did not contribute to the development of MI or stroke in the present study, similar to the results of large cohort studies at home and abroad (16,46). This indicated that any two risk factors were independent of each other in increasing the risk of MI or stroke.
Limitations
The present study had some limitations. First, causal relationships could not be established because the study was cross-sectional. Second, dyslipidemia was defined according to TC concentrations while triglyceride, low-density lipoprotein cholesterol, and high-density lipoprotein cholesterol concentrations also played important roles in the development of CVDs. Third, the generalizability of results might be limited given that the study participants were from a specific geographical region. Although this study had several shortcomings, the findings might provide guidance for designing a more systematic method for managing hypertension, diabetes, and dyslipidemia in the future. Further, precise causality can be inferred based on a comparison between the results of the present study and subsequent results.
Conclusions
In conclusion, this study indicated that the burden of hypertension and diabetes stopped increasing while TC concentration in the population was not well controlled. Individuals with two or more risk factors for CVDs accounted for a large proportion of a middle-aged population. In addition, increasing age and higher BMI were associated with the development of all three conditions. Moreover, hypertension, diabetes, and dyslipidemia contributed to an excess risk of MI and stroke independently of each other. A more comprehensive guideline needs to be developed for preventing and controlling dyslipidemia, hypertension, and diabetes. The focus of management should be on middle-aged people with multiple CVD risk factors.
Acknowledgments
Funding: The present study was supported by grants from the National Key Research & Development plan of Ministry of Science and Technology of the People’s Republic of China (No. 2018YFC1314900, 2018YFC1314901), the 2016 industry prospecting and common key technology key projects of Jiangsu Province Science and Technology Department (No. BE2016002-4), the 2016 projects of Nanjing Science Bureau (No. 201608003), the 2017 projects of Jiangsu Provincial Department of Finance (No. 2150510), the 2018 project of Jiangsu Committee of Health (No. H2018071), Research Topic on Hospital Management Innovation of Jiangsu Hospital Association (No. JSYGY-3-2017-207).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study was approved by the Ethics Committee of the First Affiliated Hospital of Nanjing Medical University (2016-SR-242, Jiangsu Province Hospital). Written informed consents were obtained from all participants before enrollment into the study. The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
References
- GBD 2017 Causes of Death Collaborators. Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet 2018;392:1736-88. [Crossref] [PubMed]
- Lim SS, Vos T, Flaxman AD, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012;380:2224-60. [Crossref] [PubMed]
- GBD 2015 Mortality and Causes of Death Collaborators. Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980-2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet 2016;388:1459-544. [Crossref] [PubMed]
- GBD 2016 Causes of Death Collaborators. Global, regional, and national age-sex specific mortality for 264 causes of death, 1980-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet 2017;390:1151-210. [Crossref] [PubMed]
- Chen WW, Gao RL, Liu LS, et al. China cardiovascular diseases report 2015: a summary. J Geriatr Cardiol 2017;14:1-10. [PubMed]
- Yang G, Wang Y, Zeng Y, et al. Rapid health transition in China, 1990-2010: findings from the Global Burden of Disease Study 2010. Lancet 2013;381:1987-2015. [Crossref] [PubMed]
- Zhou M, Wang H, Zhu J, et al. Cause-specific mortality for 240 causes in China during 1990-2013: a systematic subnational analysis for the Global Burden of Disease Study 2013. Lancet 2016;387:251-72. [Crossref] [PubMed]
- Turkstra E, Hawkes AL, Oldenburg B, et al. Cost-effectiveness of a coronary heart disease secondary prevention program in patients with myocardial infarction: results from a randomised controlled trial (ProActive Heart). Bmc Cardiovasc Disord 2013;13:33. [Crossref] [PubMed]
- Feigin VL, Nguyen G, Cercy K, et al. Global, Regional, and Country-Specific Lifetime Risks of Stroke, 1990 and 2016. N Engl J Med 2018;379:2429-37. [Crossref] [PubMed]
- Zhang G, Yu C, Zhou M, et al. Burden of Ischemic heart disease and attributable risk factors in China from 1990 to 2015: findings from the global burden of disease 2015 study. BMC Cardiovasc Disord 2018;18:18. [Crossref] [PubMed]
- Retraction and republication--ST-segment elevation myocardial infarction in China from 2001 to 2011 (the China PEACE-Retrospective Acute Myocardial Infarction Study): a retrospective analysis of hospital data. Lancet 2015;385:402. [Crossref] [PubMed]
- Liu LS. 2018 Chinese guidelines for the management of hypertension. Beijing: People’s Medical Publishing House (China), 2018.
- Zhang DD, Tang X, Jin DY, et al. Prevalence of diabetes in Chinese adults: a Meta-analysis. Zhonghua Liu Xing Bing Xue Za Zhi 2018;39:852-7. [PubMed]
- Joint Committee for Developing Chinese Guidelines on Prevention and Treatment of Dyslipidemia in Adults. 2016 Chinese guidelines on prevention and treatment of dyslipidemia in adults. Zhonghua Xin Xue Guan Bing Za Zhi 2016;44:833-53. [PubMed]
- Bloomgarden ZT. Insulin resistance, dyslipidemia, and cardiovascular disease. Diabetes Care 2007;30:2164-70. [Crossref] [PubMed]
- Sehestedt T, Hansen TW, Li Y, et al. Are blood pressure and diabetes additive or synergistic risk factors? Outcome in 8494 subjects randomly recruited from 10 populations. Hypertens Res 2011;34:714-21. [Crossref] [PubMed]
- Shu L, Zheng PF, Zhang XY, et al. Association between Dietary Patterns and the Indicators of Obesity among Chinese: A Cross-Sectional Study. Nutrients 2015;7:7995-8009. [Crossref] [PubMed]
- Boo S, Yoon YJ, Oh H. Evaluating the prevalence, awareness, and control of hypertension, diabetes, and dyslipidemia in Korea using the NHIS-NSC database: A cross-sectional analysis. Medicine (Baltimore) 2018;97:e13713. [Crossref] [PubMed]
- Lee J, Son H, Ryu OH. Management Status of Cardiovascular Disease Risk Factors for Dyslipidemia among Korean Adults. Yonsei Med J 2017;58:326-38. [Crossref] [PubMed]
- Zhai Y, Fang HY, Yu WT, et al. Epidemiological characteristics of waist circumference and abdominal obesity among Chinese adults in 2010-2012. Zhonghua Yu Fang Yi Xue Za Zhi 2017;51:506-12. [PubMed]
- American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care 2014;37 Suppl 1:S81-90. [Crossref] [PubMed]
- Mosca L, Benjamin EJ, Berra K, et al. Effectiveness-based guidelines for the prevention of cardiovascular disease in women--2011 update: a guideline from the American heart association. Circulation 2011;123:1243-62. [Crossref] [PubMed]
- Wang Z, Chen Z, Zhang L, et al. Status of Hypertension in China: Results from the China Hypertension Survey, 2012-2015. Circulation 2018;137:2344-56. [Crossref] [PubMed]
- Wang L, Gao P, Zhang M, et al. Prevalence and Ethnic Pattern of Diabetes and Prediabetes in China in 2013. JAMA 2017;317:2515-23. [Crossref] [PubMed]
- Zhang M, Deng Q, Wang L, et al. Prevalence of dyslipidemia and achievement of low-density lipoprotein cholesterol targets in Chinese adults: A nationally representative survey of 163,641 adults. Int J Cardiol 2018;260:196-203. [Crossref] [PubMed]
- Guan T, Ma J, Li M, et al. Rapid transitions in the epidemiology of stroke and its risk factors in China from 2002 to 2013. Neurology 2017;89:53-61. [Crossref] [PubMed]
- Gao XJ, Yang JG, Yang YJ, et al. Age-related coronary risk factors in Chinese patients with acute myocardial infarction. Zhonghua Yi Xue Za Zhi 2016;96:3251-6. [PubMed]
- Sarwar N, Gao P, Seshasai SR, et al. Diabetes mellitus, fasting blood glucose concentration, and risk of vascular disease: a collaborative meta-analysis of 102 prospective studies. Lancet 2010;375:2215-22. [Crossref] [PubMed]
- Zhu XL, Luo JS, Zhang XC, et al. China's Efforts on Management, Surveillance, and Research of Noncommunicable Diseases: NCD Scorecard Project. Ann Glob Health 2017;83:489-500. [Crossref] [PubMed]
- Stevens W, Peneva D, Li JZ, et al. Estimating the future burden of cardiovascular disease and the value of lipid and blood pressure control therapies in China. Bmc Health Serv Res 2016;16:175. [Crossref] [PubMed]
- Kuwabara M, Kuwabara R, Niwa K, et al. Different Risk for Hypertension, Diabetes, Dyslipidemia, and Hyperuricemia According to Level of Body Mass Index in Japanese and American Subjects. Nutrients 2018. [Crossref] [PubMed]
- Liu X, Gu W, Li Z, et al. Hypertension prevalence, awareness, treatment, control, and associated factors in Southwest China: an update. J Hypertens 2017;35:637-44. [Crossref] [PubMed]
- Zhang FL, Xing YQ, Guo ZN, et al. Prevalence and risk factors for diabetes and impaired fasting glucose in Northeast China: Results from the 2016 China National Stroke Screening Survey. Diabetes Res Clin Pract 2018;144:302-13. [Crossref] [PubMed]
- Tao LX, Yang K, Huang FF, et al. Association of Waist Circumference Gain and Incident Prediabetes Defined by Fasting Glucose: A Seven-Year Longitudinal Study in Beijing, China. Int J Environ Res Public Health 2017. [Crossref] [PubMed]
- Bragg F, Tang K, Guo Y, et al. Associations of General and Central Adiposity with Incident Diabetes in Chinese Men and Women. Diabetes Care 2018;41:494-502. [Crossref] [PubMed]
- Fu W, Cao S, Liu B, et al. Association of general and central adiposity with blood pressure among Chinese adults: results from the China National Stroke Prevention Project. J Hypertens 2018;36:2406-13. [Crossref] [PubMed]
- Yu W, Hu C, Jia W. Genetic advances of type 2 diabetes in Chinese populations. J Diabetes 2012;4:213-20. [Crossref] [PubMed]
- Juhola J, Oikonen M, Magnussen CG, et al. Childhood physical, environmental, and genetic predictors of adult hypertension: the cardiovascular risk in young Finns study. Circulation 2012;126:402-9. [Crossref] [PubMed]
- Liang Z, Qiu QY, Wu JH, et al. Alcohol Drinking, Dyslipidemia, and Diabetes: A Population-based Prospective Cohort Study among Inner Mongolians in China. Biomed Environ Sci 2016;29:555-62. [PubMed]
- Liu X, Yu S, Mao Z, et al. Dyslipidemia prevalence, awareness, treatment, control, and risk factors in Chinese rural population: the Henan rural cohort study. Lipids Health Dis 2018;17:119. [Crossref] [PubMed]
- Sun GZ, Li Z, Guo L, et al. High prevalence of dyslipidemia and associated risk factors among rural Chinese adults. Lipids Health Dis 2014;13:189. [Crossref] [PubMed]
- Zhang M, Wang LM, Chen ZH, et al. Multilevel logistic regression analysis on hypercholesterolemia related risk factors among adults in China. Zhonghua Yu Fang Yi Xue Za Zhi 2018;52:151-7. [PubMed]
- Pan L, Yang Z, Wu Y, et al. The prevalence, awareness, treatment and control of dyslipidemia among adults in China. Atherosclerosis 2016;248:2-9. [Crossref] [PubMed]
- Gupta A, Mackay J, Whitehouse A, et al. Long-term mortality after blood pressure-lowering and lipid-lowering treatment in patients with hypertension in the Anglo-Scandinavian Cardiac Outcomes Trial (ASCOT) Legacy study: 16-year follow-up results of a randomised factorial trial. Lancet 2018;392:1127-37. [Crossref] [PubMed]
- Rawshani A, Rawshani A, Franzen S, et al. Risk Factors, Mortality, and Cardiovascular Outcomes in Patients with Type 2 Diabetes. N Engl J Med 2018;379:633-44. [Crossref] [PubMed]
- Zhang Y, Jiang X, Bo J, et al. Risk of stroke and coronary heart disease among various levels of blood pressure in diabetic and nondiabetic Chinese patients. J Hypertens 2018;36:93-100. [Crossref] [PubMed]