
Is it “hybrid” or “intermediate”?—more than just a semantic issue in oncocytic renal cell tumors
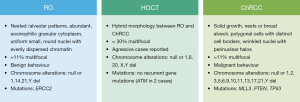
Hybrid oncocytic/chromophobe tumor (HOCT) is a neoplasm of renal cells encompassing cellular and architectural features of both renal oncocytoma (RO) and chromophobe renal cell carcinoma (ChRCC) (1). The first cases were recognized in patients with Birt-Hogg-Dubé (BHD) syndrome and sporadic cases were also identified, subsequently. HOCT may show distinct typical RO and typical ChRCC areas admixed within the same tumor or composite/ambiguous morphologic and immunohistochemical features intermediate between RO and ChRCC (1). Although the latest [2016] World Health Organization classification of renal cell neoplasms considers HOCT a ChRCC subtype (2), the place of HOCT in the spectrum of renal cell neoplasms remains controversial.
A recent publication from Ruiz-Cordero and co-workers attempts to illuminate the apparently dual nature of HOCT through an in-depth molecular characterization, comparing it with RO and ChRCC (3). The majority of HOCT cases analyzed in this study were sporadic and most disclosed the expected ambiguous morphology between RO and ChRCC (with only rare tumor foci displaying an abrupt transition between RO-like and ChRCC-like areas). Starting by comparing clinical and pathological characteristics of sporadic HOCT versus RO and ChRCC, the authors reported a higher frequency of multifocality in HOCT (30%) contrasting with only 11% of multifocal RO and ChRCC cases. In addition, two HOCT cases with aggressive features are reported (one case with metastasis in the liver causing patient’s death and a case with RCC of unclassified type arising in a HOCT background). Remarkably, only one other case of metastatic HOCT has been reported to date (4).
Then, the authors extensively analyzed some molecular features of HOCT cases. They performed targeted exon sequencing in 16 samples (corresponding to 14 patients): next-generation sequencing with target capture and sequencing of 261 cancer-associated genes using an in-house-developed assay (T200.1) (5). This panel was previously validated and found to be as precise as a commercially available CLIA-compliant hotspot panel, permitting the detection of a larger number of actionable gene mutations (5). The mutational landscape of HOCT unraveled by Ruiz-Cordero et al. remarkably discloses the absence of mutations in classic driver genes of renal cell carcinoma (RCC) and RO (such as VHL, BAP1, FH, MET, PTEN, TERT, TP53, ERCC2 and SDHA-D). Indeed, only one somatic mutation was found in five cases, each (including two patients with ATM gene mutations, an uncommon feature for RCC). Using publicly available data for comparison, the authors underscore significant differences between HOCT and ChRCC in terms of TP53, PTEN or MLL3 mutations. Furthermore, ERCC2 mutations, classically described in RO, were not found in the analyzed HOCT, although the number of cases was insufficiently powered to demonstrate statistical significance.
The T200.1 panel also allows for evaluation of whole-genome copy number alterations. Thus, 9/15 (60%) HOCT samples evaluated disclosed chromosomal copy number alterations. In three samples, loss of chromosome 1 was the only alteration depicted and one sample disclosed loss of chromosomes 1 and Y, only. The authors, then, concluded that copy number alteration profile of HOCT was closer to RO than to the genome wide chromosomal copy number alterations typically displayed by ChRCC. Even the HOCT case with liver metastasis, which presented multiple copy number alterations, showed copy number losses (2p-, 5p-, 8p-, 9p-, 19p-) quite different from the typical losses occurring in ChRCC (involving chromosomes 1, 2, 6 10, 13, 17 and 21). Tumor ploidy was also assessed and, remarkably, only the metastatic HOCT disclosed a ploidy value of 5.2, and a whole-genome doubling ratio of 1, sharply contrasting with the other HOCTs (with no metastases) which displayed near diploid ploidy values and lower whole-genome doubling ratios.
The following step was to analyze and compare the gene expression profile of HOCT, RO and ChRCC. Firstly, in silico analysis of publicly available gene expression data was done to detect the most differentially expressed genes between RO and ChRCC and the genes associated with aggressive behavior of ChRCC. The most differentially expressed genes in terms of fold change, and genes that were differentially expressed across the various studies, were selected. This expression signature of renal cell oncocytic neoplasms was subsequently evaluated in tissue material using Nanostring’s nCounter (NanoString Technologies) platform. Concerning RNA transcript data, HOCTs leading fold change values were intermediate between those of RO and ChRCC. Interestingly, the two aggressive HOCT cases did not cluster towards ChRCC. Moreover, a subgroup of genes was significantly differentially expressed in HOCT vs. RO (n=25 genes) and in HOCT vs. ChRCC (n=58 genes).
The study of Ruiz-Cordero et al. provides very relevant and detailed data concerning the genetic landscape of HOCT: in addition to assess DNA copy number alterations it also examined, for the first time, the mutational and transcriptomic profile of these neoplasms in direct comparison with RO and ChRCC. Previous studies had also analyzed DNA copy number alterations in HOCT case series (6,7). Indeed, Petersson et al. found, in one or more of the chromosomes tested, either monosomy or polysomy in all 14 cases analyzed (most commonly they found chromosome 20 monosomy) (6), but these alterations were distinct from the cytogenetic anomalies classically found in ChRCC or RO: combined losses of 1, 2, 6, 10, 13, 17, 21 and Y in ChRCC (with eosinophilic variant showing fewer or no genetic losses) and losses of 1, 14, Y; 11q rearrangements or normal karyotype in RO (2). Contrarily, Poté et al. found no chromosome imbalance in most HOCT cases tested (58% of the 12 cases studied), whereas chromosome 1 deletions were identified in four cases, similar to RO (7). These findings, in addition to the demonstration of apical Hale staining and the globally favorable prognosis of HOCT cases (also similar to RO), suggested that the molecular profile of HOCT was nearer to RO (7). Concerning DNA copy number, the findings of Ruiz-Cordero et al. are closer to those of Poté et al., with predominant losses of chromosome 1 or Y and ~40% of cases lacking chromosomal gains or losses, similarly to RO (or to some ChRCC, namely the eosinophilic variant). Interestingly, the similarity between HOCT and RO seems to be more evident regarding DNA copy number alterations, since deep-targeted next-generation sequencing of HOCTs failed to find the same gene mutations commonly described in RO (namely in ERCC2) (8). The gene mutations found in HOCT were also distinct from those most frequently described in ChRCC (such as in PTEN, TERT and TP53) (8,9). Moreover, the mRNA signature of HOCT also appears distinct from RO and ChRCC, with HOCT displaying an intermediate profile between RO and ChRCC, although seemingly closer to RO than to ChRCC, as apparent in Figure 3 of Ruiz-Cordero et al. (3).
One limitation of this study is the small number of cases associated with BHD syndrome included in the analysis (two cases of patients with BHD stigmata; one of these was genetically confirmed). This might be expected since these correspond to the minority of cases available. Could the findings be different if a bigger sample of such cases is analyzed? Also, could there be different molecular profiles between sporadic and BHD-related cases? Curiously, in sporadic HOCT cases, no folliculin (FLCN) gene mutations were found. Another aspect is that the study of Ruiz-Cordero et al. comprised mostly cases with morphologic intermingled features of RO and ChRCC and, as such, no separate microdissection of the different components was performed. Indeed, there seems to be two different types of HOCT at morphological level: those disclosing “hybrid” features between RO and ChRCC at cellular and architectural level, and those showing discrete RO-like and ChRCC-like foci (mosaic pattern) within the same neoplasm. We have recently reported one HOCT case disclosing the mosaic pattern, in which chromosomal alterations (using FISH) and differential microRNA expression were assessed in each component separately (10). Interestingly, higher relative miR-141 and miR200b expression were found in the ChRCC-like area, whereas higher miR-21 was depicted in the RO-like areas, in agreement with our previous observations in sporadic ChRCC and sporadic RO (11). Using FISH analyses, we have also found a dissimilar genetic pattern among RO-like and ChRCC-like components, i.e., multiple tetrasomies or no chromosomal alterations, respectively. This contrasted with the previous study of Poté et al. that found no differences between the two HOCT components, using comparative genomic hybridization (7). Thus, we believe that analysis of a larger number of HOCT cases including tumors with mosaic pattern allowing for differential assessment of RO-like and ChRCC-like foci will further illuminate the origin and character of HOCT. Indeed, we are tempted to speculate whether HOCT cases disclosing the mosaic pattern might also differ (clinically and molecularly) from those showing the intermingled/ambiguous morphology.
All in all, available data on HOCT sustain the perception that it may represent a distinct disease entity, with some features resembling RO or ChRCC (e.g., copy number alterations and specific microRNA expression), whilst others differ more significantly (e.g., mutational and transcriptomic profile). Although some of the molecular alterations of HOCT seem closer to those reported for RO, there are relevant differences between these neoplasms: HOCTs are morphologically distinct, more frequently multifocal, display a different mutational profile and, importantly, may exhibit an aggressive clinical behavior (Figure 1). A similar scenario could be set for HOCT vs. ChRCC. Thus, more than “hybrid” tumors, HOCT seem, indeed, to bear “intermediate” characteristics between RO and ChRCC. Finally, HOCT is a remarkably heterogeneous neoplasm, suggesting the existence of different tumor subsets. Additional genetic and epigenetic characterization of a larger series of HOCT, including BHD-related cases and cases representing the different histological patterns, might provide critical evidence for the recognition of this distinct renal cell tumor type.
Acknowledgments
Funding: This work was supported by a grant from Research Center of Portuguese Oncology Institute of Porto (PI 112-CI-IPOP 92-2018-MCTKidCan)
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
References
- Mai KT, Dhamanaskar P, Belanger E, et al. Hybrid chromophobe renal cell neoplasm. Pathol Res Pract 2005;201:385-9. [Crossref] [PubMed]
- Moch H, Humphrey PA, Ulbright TM, et al. editors. WHO Classification of Tumours of the Urinary System and Male Genital Organs. International Agency for Research on Cancer, 2016.
- Ruiz-Cordero R, Rao P, Li L, et al. Hybrid oncocytic/chromophobe renal tumors are molecularly distinct from oncocytoma and chromophobe renal cell carcinoma. Mod Pathol 2019. [Epub ahead of print]. [Crossref] [PubMed]
- Aslam MI, Spencer L, Garcea G, et al. A case of liver metastasis from an oncocytoma with a focal area of chromophobe renal cell carcinoma: a wolf in sheep's clothing. Int J Surg Pathol 2009;17:158-62. [Crossref] [PubMed]
- Chen K, Meric-Bernstam F, Zhao H, et al. Clinical actionability enhanced through deep targeted sequencing of solid tumors. Clin Chem 2015;61:544-53. [Crossref] [PubMed]
- Petersson F, Gatalica Z, Grossmann P, et al. Sporadic hybrid oncocytic/chromophobe tumor of the kidney: a clinicopathologic, histomorphologic, immunohistochemical, ultrastructural, and molecular cytogenetic study of 14 cases. Virchows Arch 2010;456:355-65. [Crossref] [PubMed]
- Poté N, Vieillefond A, Couturier J, et al. Hybrid oncocytic/chromophobe renal cell tumours do not display genomic features of chromophobe renal cell carcinomas. Virchows Arch 2013;462:633-8. [Crossref] [PubMed]
- Durinck S, Stawiski EW, Pavía-Jiménez A, et al. Spectrum of diverse genomic alterations define non-clear cell renal carcinoma subtypes. Nat Genet 2015;47:13-21. [Crossref] [PubMed]
- Davis CF, Ricketts CJ, Wang M, et al. The somatic genomic landscape of chromophobe renal cell carcinoma. Cancer Cell 2014;26:319-30. [Crossref] [PubMed]
- Pires-Luis A, Montezuma D, Vieira J, et al. Hybrid oncocytic/chromophobe renal cell tumor: An integrated genetic and epigenetic characterization of a case. Exp Mol Pathol 2018;105:352-6. [Crossref] [PubMed]
- Silva-Santos RM, Costa-Pinheiro P, Luis A, et al. MicroRNA profile: a promising ancillary tool for accurate renal cell tumour diagnosis. Br J Cancer 2013;109:2646-53. [Crossref] [PubMed]


