
Additional effect of neuromuscular electrical stimulation on knee extension lag, pain and knee range of motion in immediate postsurgical phase (0–2 weeks) in primary total knee arthroplasty patient
Introduction
Knee joint osteoarthritis (OA) is the second most existing disease in India with the prevalence of 22% to 39%. It is more commonly seen in females than in males, also the disease tremendously increases with the age leading to pain, inflammation, impairments in mobility, etc. (1,2). Total knee arthroplasty (TKA) is the treatment for the individuals with end stage disease (3). TKA is a surgical procedure in which the weight bearing surfaces of the knee joint are changed with an implant which consists of 3 components- femoral component, tibial component, a centre plate and it may or may not consist of a tibial extension rod. TKA is a procedure done to relieve pain and disability of the patients (4).
Despite the recent advances in the TKA, there are numerous studies suggesting that TKA is not achieving the goal of reducing pain and restoring function (5-7). Few of the complications that arise post TKA are pain in and around the knee joint, loss of knee joint range of motion (ROM), reduced quadriceps muscle activation giving rise to an extension lag (8). There are also functional limitations like reduced walking speed, difficulty in ascending and descending stairs, etc. The satisfaction index is found to be low in patients with post TKA resulting in pain and poor functional outcomes due to weakness in quadriceps muscle strength, and voluntary activation (3). It is found that because of constant deficits in residual quadriceps femoris muscle strength after TKA can prevent patients from returning quickly and fully to functional activities. It is seen that the muscle activation failure is not only due to knee pain during muscle contraction in the patient population, but due to failure of voluntary muscle activation (attributed to reflex inhibition) and atrophy contributed to strength loss (force generation capacity) (9,10). Studies have shown almost 19% to 23% deficits in knee flexor and extensor muscle power. This significant reduction in muscle strength should be taken into consideration during rehabilitation programs, because in day to day activities it is important to have the muscle power, needed to produce effective force quickly to generate desirable and prevent undesirable movements (11).
It is seen that, post TKA the quadriceps muscle strength drops by 50% to 60% of the pre-operative levels, despite introducing early rehabilitation i.e., within 2 days after surgery (9,12). Hence, improving pain and muscle weakness should be the primary aim while treating patients post TKA. Physiotherapy management post TKA includes, cryotherapy and electrotherapy, exercises and hydrotherapy to reduce pain and improve strength and function (13,14). Various studies on younger adults have shown that neuromuscular electrical stimulation (NMES), at sufficient intensities, combined with active exercises had better improvement in muscle strength and functional performance than exercises alone (15). A case series reported that, use of high intensity NMES on quadriceps muscle in early stage of rehabilitation, improves its strength drastically in patients with TKA (16).
In most of the studies performed, NMES was given at a later stage of the rehabilitation program post a TKA (16,17). Very limited research is available for giving NMES in the early acute stages post TKA. So, the short-term effect of NMES had not yet been researched upon widely. As, there were conflicting evidences in giving NMES post TKA, this study was proposed to assess the short-term effect of early NMES on knee joint pain, ROM and extension lag on patients undergoing bilateral TKA.
Methods
The study included 28 bilateral TKA patients following OA knee within the age group of 50–75 years (60.82±5.69). Patients who perceived pain between 4 to 10 on visual analogue scale (VAS) i.e., moderate to severe, both males and females were included in the study (12 males, 16 females). Patients suffering from any cardiovascular or neurological conditions, surgical complications post TKA, where rehabilitation protocol needed to be altered and contraindication to NMES where excluded from the study. The study was done in a hospital setup. The study was approved from the Institutional Review Board. The study was explained to all the patients and a written informed consent was taken from all the patients.
The knees of 28 bilaterally operated patients were randomly divided into two groups: experimental and control group; 1 knee was allocated in the experimental group and the other knee of the same patient became the control. Experimental group was given NMES with exercises, while control group was given only exercises. The intervention was given for 7 days which started on day 3 post operatively (post op) and continued till day 9 post operatively. The patients were assessed for pain on VAS, knee ROM in side lying and knee extension lag in supine lying with an angle frame, before the intervention on day 3 and on day 9 after the intervention (18,19). Both the groups were advised to apply ice packs every two hours till day 9 to reduce pain and swelling (13).
Experimental group: in addition to exercises NMES was given to this group. The Empi PHOENIX NMES was used which consisted of 4 programs, P1-Endurance, P2-Strength, P3-Modulated TENS and P4-Edema. In this study, we used program P2 for strength. The waveform was symmetrical square biphasic asynchronous. There were three phases in this program, warm up, work phase and cool down phase. It was a battery operated machine. The warm up treatment time consisted to 2 min with a continuous cycle, frequency 6 Hz. In the work phase, the treatment time was 15 min, cycle type was intermittent. Frequency of work was 75 Hz and that of rest was 4 Hz with work time to be 4 s and rest time was 10 s. This was followed by cool down with a treatment time of 3 min and cool down frequency is 3 Hz. The cycle was continuous. The pulse duration was 300 µs throughout the program (20).
The patient was in supine lying with an angle frame below the knee on slot 1, which maintained the knee flexion in 15º of flexion. Four electrodes of NMES were placed over maximum bulk of quadriceps femoris muscle, and patient was asked to perform active terminal knee extension along with NMES (whenever the current is perceived) as many repetitions as the subject could perform. NMES was given for 20 min. Gradually as the knee joint ROM increased the angle frame slots were increased till the third slot. So, till day 9 all the subjects could perform knee extension on angle frame on slot 3 which was 45º of knee flexion.
Control group: Exercises were started from day 1 post operatively which continued till day 9 (14,16,21,22).
In Supine position: (I) ankle toe movements, 10 repetitions; (II) isometric contraction of quadriceps, hamstrings, gluteus maximus, 10 repetitions with 6 s hold; (III) straight leg raise, 10 repetitions; (IV) hip abduction, 10 repetitions; (V) hip knee flexion, 10 repetitions; (VI) posterior capsular stretching, 30 s × 3 sets.
Progression to Side line position: (I) hip abduction, 10 repetitions; (II) knee flexion, 10 repetitions.
Bed side sitting: dynamic activation of quadriceps, 10 repetitions.
Walking with aid of walker weight bearing as per tolerance.
Results
The results were analysed using SPSS version 18. Within group analysis for VAS was done using Wilcoxon signed rank test and between for the same was done using Mann Whitney U test. While within group comparison for knee ROM and extension lag was done using paired t test and between group analyses was done using unpaired t test. The significance level was set at P≤0.05.
As there was no baseline matching for extensor lag, no statistical test was performed. Hence, the percent change was calculated, which was 71% in the exp group and that in control group, was only 67%.
Discussion
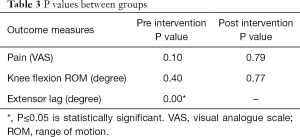
This study was done to find out the additional effect of NMES on extensor lag, knee ROM and pain in TKA patients. There was significant improvement in both the groups with respect to extensor lag, knee ROM and pain P≤0.05 (Tables 1,2). It was seen that pain and knee flexion range improved in both the groups but there was no significant difference between the groups P>0.05 (Table 3). Individually in the groups, the pain and knee flexion range did improve from the baseline values i.e., the exercises and NMES did have an effect on pain and knee flexion range. The improvement in pain and ROM can be attributed to the improved quadriceps muscle strength and thereby improving the stability of the knee joint (23).

Full table

Full table
Full table
Furthermore, a study done by Lim et al. 2008 (24) reported that quadriceps strengthening has a positive effect on pain and function in patients with OA knee. There is also another study done by Amin et al. 2009 (25) which stated that subjects having better quadriceps strength had less knee pain and enhanced physical function as compared to those with the lower strength. Strong muscles help in stabilizing the joints in a proper alignment, reduce shocks that are transmitted to the joints and also help in reducing the effect of impact by spreading the forces to a larger area so it may be said that improving muscle strength would help in reducing pain and disability.
The extension lag also improved from baseline to day 9 in both the groups, the percent change in experimental group was 71% as compare to control which was only 67%. Hence it could be attributed to NMES which helps in activating a larger portion of type II muscle fibers than through volitional exercise at comparable intensities (26,27).
Besides, afferent input from NMES may help in facilitating plastic changes throughout sensorimotor networks in the central nervous system, ultimately improving strength and motor control (28). These neural changes have been specifically sought for patients following neurologic injury. For example, in patients following stroke, a 77% improvement in quadriceps force and nearly 20% improvement in motor unit recruitment were achieved through NMES treatment, compared to minimal changes in a group of patients not receiving NMES (29).
The knee extensor lag in the experimental group reduced by 10º while in control group the reduction was only by 5.79º. Our study results are in agreement with Gotlin et al., 1994 (30) where they reported that when NMES applied within the first week after TKA reduced the knee extensor lag by 2 degrees compared with controls, who had an increase in extensor lag by 3 degrees in the same time frame.
Even though it has been difficult to establish the underlying muscular and neural mechanisms responsible for improved muscle performance with NMES, some theories have been postulated. The first is related to the intensity of the muscle contraction produced during stimulation. It has been recommended that, individuals with negligible muscle recruitment require at least 50% to 60% of maximal voluntary effort to over-burden the muscle adequately to promote hypertrophy, because higher the power more prominent is the hypertrophy (31,32). Similar to high-intensity voluntary muscle contractions, electrically induced muscle contractions at high intensities produce muscle hypertrophy and in turn help in increasing the strength (33,34). Electrically induced muscle contractions help in activation of a greater amount of type II muscle fibers than volitional exercise at the same intensity (35,36). As type II muscle fibers are larger than type I fibers, there is greater activation of these fibers which help in increasing the force production (37). There are evidences suggesting, that NMES affects functional motor performance measures via peripheral afferent inputs that change the excitability of the motor cortex (28,38). Stimulation of these peripheral afferent nerves can cause extended changes in the excitability of the human motor cortex, which can help explain improvements in muscle function with NMES (39,40).
However, there was no significant difference between the groups; our results are in agreement with other studies where they found similar outcomes. A systematic review done by Volpato et al., 2016 (41) found studies where pain and ROM did not have a statistically significant difference between the groups, Stevens-Lapsley et al. 2012 (42) and Petterson et al. 2009 (17) reported no statistically significant difference between NMES and exercise groups (P>0.01). In a study done by Mizusaki Imoto et al. 2013 (43), where they found that there was no significant difference between NMES+ ex and exercise group alone with respect to pain and knee flexion ROM. Hence, in the present study, the training intensities and the time period where NMES was given were lower than those expected to produce muscle hypertrophy. Therefore, we can conclude that, altered motor unit recruitment may explain some of the improvements in muscle function.
As there was no baseline matching for extensor lag, the results of this study are inconclusive of whether NMES has an additional effect on extensor lag, pain and knee ROM after TKA. Hence it would be appropriate to do the study on a larger sample which will give us more definitive results.
Conclusions
The present study was done to understand the additional effect of NMES along with exercises on extensor lag, knee flexion ROM and pain after TKA. There was a significant improvement with NMES and exercises with respect to extensor lag, knee ROM and pain, but when compared between the groups, both the groups performed equally well. Hence our results concluded that there was no additional effect of NMES on extensor lag, knee ROM and pain when applied for 7 days in patients operated with TKA.
Acknowledgments
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was approved from the Institutional Review Board (IRB-SIOR/Agenda043/09). The study was explained to all the patients and a written informed consent was taken from all the patients.
References
- Pal CP, Singh P, Chaturvedi S, et al. Epidemiology of knee osteoarthritis in India and related factors. Indian J Orthop 2016;50:518-22. [Crossref] [PubMed]
- Akinpelu AO, Alonge TO, Adekanla BA, et al. Prevalence and pattern of symptomatic knee osteoarthritis in Nigeria: A community-based study. Internet J Allied Health Sci Pract 2009;7:3.
- Bourne RB, Chesworth BM, Davis AM, et al. Patient satisfaction after total knee arthroplasty: who is satisfied and who is not? Clin Orthop Relat Res 2010;468:57-63. [Crossref] [PubMed]
- Lewek M, Stevens J, Snyder-Mackler L. The use of electrical stimulation to increase quadriceps femoris muscle force in an elderly patient following a total knee arthroplasty. Phys Ther 2001;81:1565-71. [Crossref] [PubMed]
- Dunbar MJ, Robertsson O, Ryd L, et al. Appropriate questionnaires for knee arthroplasty. Results of a survey of 3600 patients from the Swedish Knee Arthroplasty Registry. J Bone Joint Surg Br 2001;83:339-44. [Crossref] [PubMed]
- Hawker G, Wright J, Coyte P, et al. Health-related quality of life after knee replacement. Results of the knee replacement patient outcomes research team study. J Bone Joint Surg Am 1998;80:163-73. [Crossref] [PubMed]
- Heck DA, Robinson RL, Partridge CM, et al. Patient outcomes after knee replacement. Clin Orthop 1998.93-110. [Crossref] [PubMed]
- Gondin J, Cozzone PJ, Bendahan D. Is high-frequency neuromuscular electrical stimulation a suitable tool for muscle performance improvement in both healthy humans and athletes? Eur J Appl Physiol 2011;111:2473. [Crossref] [PubMed]
- Mizner RL, Petterson SC, Snyder-Mackler L. Quadriceps strength and the time course of functional recovery after total knee arthroplasty. J Orthop Sports Phys Ther 2005;35:424-36. [Crossref] [PubMed]
- Moore SD, Laudner KG, Mcloda TA, et al. The immediate effects of muscle energy technique on posterior shoulder tightness: a randomized controlled trial J Orthop Sports Phys Ther 2011;41:400-7. [Crossref] [PubMed]
- Monaghan B, Caulfield B, O'Mathúna DP. Surface neuromuscular electrical stimulation for quadriceps strengthening pre and post total knee replacement. Cochrane Database Syst Rev 2010.CD007177. [PubMed]
- Stevens JE, Mizner RL, Snyder-Mackler L. Quadriceps strength and volitional activation before and after total knee arthroplasty for osteoarthritis. J Orthop Res 2003;21:775-9. [Crossref] [PubMed]
- Kullenberg B, Ylipää S, Söderlund K, et al. Postoperative Cryotherapy after Total Knee Arthroplasty. J Arthroplasty 2006;21:1175-9. [Crossref] [PubMed]
- Mockford BJ, Thompson NW, Humphreys P, et al. Does a standard outpatient physiotherapy regime improve the range of knee motion after primary total knee arthroplasty? J Arthroplasty 2008;23:1110-4. [Crossref] [PubMed]
- Delitto A, Snyder-Mackler L. Two theories of muscle strength augmentation using percutaneous electrical stimulation. Phys Ther 1990;70:158-64. [Crossref] [PubMed]
- Stevens JE, Mizner RL, Snyder-Mackler L. Neuromuscular Electrical Stimulation for Quadriceps Muscle Strengthening After Bilateral Total Knee Arthroplasty: A Case Series. J Orthop Sports Phys Ther 2004;34:21-9. [Crossref] [PubMed]
- Petterson SC, Mizner RL, Stevens JE, et al. Improved function from progressive strengthening interventions after total knee arthroplasty: a randomized clinical trial with an imbedded prospective cohort. Arthritis Rheum 2009;61:174-83. [Crossref] [PubMed]
- Crossley KM, Bennell KL, Cowan SM, et al. Analysis of outcome measures for persons with patellofemoral pain: which are reliable and valid? Arch Phys Med Rehabil 2004;85:815-22. [Crossref] [PubMed]
- Norkin CC, White DJ. Measurement of Joint Motion: A Guide to Goniometry. 3rd edition. Philadelphia: FA Davis Co, 2003.
- Empi PHOENIX Complete Electrotherapy System. Empi Inc., Clear Lake, USA, 2013. Accessed on: June 13, 2019. Available online: https://total-wellness.co.uk/wp-content/uploads/Empi-Phoenix-Manual1.pdf
- Kramer JF, Speechley M, Bourne R, et al. Comparison of clinic and home-based rehabilitation programs after total knee arthroplasty. Clin Orthop Relat Res 2003.225-34. [Crossref] [PubMed]
- Demircioglu DT, Paker N, Erbil E, et al. The effect of neuromuscular electrical stimulation on functional status and quality of life after knee arthroplasty: a randomized controlled study. J Phys Ther Sci 2015;27:2501-6. [Crossref] [PubMed]
- Anwer S, Alghadir A. Effect of Isometric Quadriceps Exercise on Muscle Strength, Pain, and Function in Patients with Knee Osteoarthritis: A Randomized Controlled Study. J Phys Ther Sci 2014;26:745-8. [Crossref] [PubMed]
- Lim BW, Hinman RS, Wrigley TV, et al. Does knee malalignment mediate the effects of quadriceps strengthening on knee adduction moment, pain, and function in medial knee osteoarthritis? A randomized controlled trial. Arthritis Rheum 2008;59:943-51. [Crossref] [PubMed]
- Amin S, Baker K, Niu J, et al. Quadriceps strength and the risk of cartilage loss and symptom progression in knee osteoarthritis. Arthritis Rheum 2009;60:189-98. [Crossref] [PubMed]
- Gregory CM, Bickel CS. Recruitment patterns in human skeletal muscles during electrical stimulation. Phys Ther 2005;85:358-64. [PubMed]
- Maffiuletti NA. Physiological and methodological considerations for the use of neuromuscular electrical stimulation. Eur J Appl Physiol 2010;110:223-34. [Crossref] [PubMed]
- Golaszewski S, Kremser C, Wagner M, et al. Functional magnetic resonance imaging of the human motor cortex before and after whole hand afferent electrical stimulation. Scand J rehabil Med 1999;31:165-73. [Crossref] [PubMed]
- Newsam CJ, Baker LL. Effect of an electric stimulation facilitation program on quadriceps motor unit recruitment after stroke. Arch Phys Med Rehabil 2004;85:2040-5. [Crossref] [PubMed]
- Gotlin RS, Hershkowitz S, Juris PM, et al. Electrical stimulation effect on extensor lag and length of hospital stay after total knee arthroplasty. Arch Phys Med Rehabil 1994;75:957-9. [PubMed]
- Kalapotharakos VI, Michalopoulou M, Godolias G, et al. The effects of high- and moderate-resistance training on muscle function in the elderly. J Aging Phys Act 2004;12:131-43. [Crossref] [PubMed]
- Kraemer WJ, Adams K, Cafarelli E, et al. American College of Sports Medicine position stand: progression models in resistance training for healthy adults. Med Sci Sports Exerc 2002;34:364-80. [Crossref] [PubMed]
- Snyder-Mackler L, Delitto A, Stralka SW, et al. Use of electrical stimulation to enhance recovery of quadriceps femoris muscle force production in patients following anterior cruciate ligament reconstruction. Phys Ther 1994;74:901-7. [Crossref] [PubMed]
- Stackhouse SK, Binder-Macleod SA, Stackhouse CA, et al. Neuromuscular electrical stimulation versus volitional isometric strength training in children with spastic diplegic cerebral palsy: a preliminary study. Neurorehabil Neural Repair 2007;21:475-85. [Crossref] [PubMed]
- Binder-Macleod SA, Halden EE, Jungles KA. Effects of stimulation intensity on the physiological responses of human motor units. Med Sci Sports Exerc 1995;27:556-65. [Crossref] [PubMed]
- Sinacore DR, Delitto A, King DS, et al. Type II fiber activation with electrical stimulation: a preliminary report. Phys Ther 1990;70:416-22. [Crossref] [PubMed]
- Young A. The relative isometric strength of type I and type II muscle fibres in the human quadriceps. Clin Physiol 1984;4:23-32. [Crossref] [PubMed]
- Tinazzi M, Zarattini S, Valeriani M, et al. Long-lasting modulation of human motor cortex following prolonged transcutaneous electrical nerve stimulation (TENS) of forearm muscles: evidence of reciprocal inhibition and facilitation. Exp Brain Res 2005;161:457-64. [Crossref] [PubMed]
- Kimberley TJ, Lewis SM, Auerbach EJ, et al. Electrical stimulation driving functional improvements and cortical changes in subjects with stroke. Exp Brain Res 2004;154:450-60. [Crossref] [PubMed]
- Svensson P, Miles TS, McKay D, et al. Suppression of motor evoked potentials in a hand muscle following prolonged painful stimulation. Eur J Pain 2003;7:55-62. [Crossref] [PubMed]
- Volpato HB, Szego P, Lenza M, et al. Femoral quadriceps neuromuscular electrical stimulation after total knee arthroplasty: a systematic review. Einstein (São Paulo) 2016;14:77-98. [Crossref] [PubMed]
- Stevens-Lapsley JE, Balter JE, Wolfe P, et al. Early neuromuscular electrical stimulation to improve quadriceps muscle strength after total knee arthroplasty: a randomized controlled trial. Phys Ther 2012;92:210-26. [Crossref] [PubMed]
- Mizusaki Imoto A, Peccin S, Gomes da Silva KN, et al. Effects of neuromuscular electrical stimulation combined with exercises versus an exercise program on the pain and the function in patients with knee osteoarthritis: a randomized controlled trial. Biomed Res Int 2013;2013:1-7.


