Evaluation of aniseikonia with an auto-stereoscopic smartphone
Introduction
Aniseikonia is a binocular condition in which the apparent sizes of the images seen by the two eyes are unequal. The symptoms of aniseikonia may express as headache, asthenopia, photophobia, reading difficulty, nausea, vertigo, and dizziness (1,2).
Aniseikonia can be classified as physiologically, neurologically, optically, or retinally induced (3). Physiological aniseikonia originates from the physiological differences between the two eyes. Neurological aniseikonia arises from the cortical neural processing of the input images from two eyes. Optical aniseikonia is caused by the difference of refractive components between the two eyes, and is commonly associated with anisometropia, especially when correcting with spectacles. However, according to Knapp’s law, using spectacles to correct axial anisometropia while using contact lenses to correct refractive anisometropia may make the optical retinal images of the two eyes closer to each other, and thus improve aniseikonia symptoms. Despite this solution, the situation is different in clinical practice. Using contact lenses to reduce aniseikonia is more effective than wearing spectacles. The cause of aniseikonia is not simply caused by the angular sizes of images falling on each retina. It also affected by the distribution of the retinal receptive fields and the cortical mapping of the visual fields in the brain (3). Oblique astigmatism, aphakia, pseudophakia, and corneal refractive surgery, can lead to optical aniseikonia (4-6). Retinal-induced aniseikonia is caused by the stretching or compression of the retina, which leads to the distribution density of photoreceptors changing (7). Retinal-induced aniseikonia has been reported in various pathologies, including epiretinal membrane (ERM) (8-12), retinal detachment (RD) (13-15), age-related macular degeneration (AMD) (16), macular edema (ME) (17), central serous chorioretinopathy (CSCR) (18), macular hole (MH) (2,19), cystoid ME with retinal vein occlusion, and diabetic macular edema (DME) (2). The change of distribution of photoreceptors may induce aniseikonia. If the photoreceptors are compressed more closely than normal, the image of a subject may stimulate more receptors than normal and appear larger than usual. If the photoreceptors are stretched apart, the image may stimulate fewer receptors than normal and appear smaller than usual. Some disorders, like ERM, may express macropsia, while others, like MH, BRVO-CME, CRVO-CME, and DME, may express micropsia.
There is a variety of measuring instruments to evaluate aniseikonia in clinical and research fields. Size lenses are commonly used to test aniseikonia. Size lenses are a type of afocal lens which can change the magnification rate without changing the refractive power. They can be used to measure aniseikonia and induce aniseikonia for research purposes in order to investigate the accuracy of testing paradigms (3,20). The gold-standard test for measuring aniseikonia is the space eikonometer (American Optical Corp, Southbridge, MA, USA); however, it is rarely used in clinical practice (3,21). The standard eikonometer is a project instrument equipped with a polarizing filter to conduct aniseikonia examination (1,3). Maddox rod test (Brecher test) and double Maddox rod test (Miles test) are all direct comparison techniques. Size lenses are adopted to measure aniseikonia in the above tests. With the development of information technology, computer-aided aniseikonia evaluation tools have been invented. The Aniseikonia Inspector (Optical Diagnostics, Culemborg, Netherlands) is a computer-based test which is assisted by red-green anaglyph glasses (21-24). The most widely used test in clinic is the New Aniseikonia Test (Handaya Co. Ltd., Japan), a hand-held test booklet (23). Both these tests use red/green anaglyph technology to separate the images between the right- and the left-eye.
However, more people are encountering refractive errors that require spectacles to correct. Wearing another set of glasses in addition to an existing one is uncomfortable and inconvenient. The auto-stereoscopic method, or naked-eye 3D display, can separate binocular vision without the help of red-green or polarizing glasses. With the development of information technology, the auto-stereoscopic method, which has been used in large-screen displays for advertising or home entertainment for a long time, is now available in modern smartphones. The resolutions of smartphone screens can reach up to 1920×1080 pixels, and sometimes 2560×1440 pixels. This high-density display makes the displayed images appear fine and smooth. We were interested in investigating the effect of this technology when used to detect aniseikonia with a portable auto-stereoscopic smartphone with the aim of obviating the need to wear glasses.
Methods
Test equipment and procedure
The Awaya new aniseikonia test
We conducted a modified Awaya new aniseikonia test in our study. A typical test is described below.
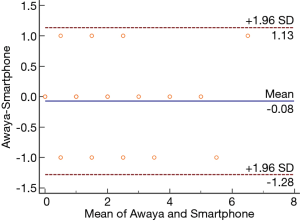
The test picture contains one red halfmoon on the left side and one green halfmoon on the right side, and a black cross set in the middle of the two halfmoons. A number indicating the rate of aniseikonia is placed at the lower left of the pattern. The diameter of the red halfmoon is fixed at 40 mm for the whole test, while the diameter of the green halfmoon changes. The diameter of the green halfmoon is smaller than 40 mm from No. 1 to No. 24. The diameter can be calculated by the number; e.g., the diameter of No. 20 is 40×(1−0.2)=32 mm, and the diameter of the green halfmoon is larger than 40 mm from No 1’ to No 24’. The diameter can also be calculated by the number; e.g., the diameter of No 20’ is 40×(1+0.2)=48 mm.
The test distance is usually set at 40 cm. When starting the test, the participant should wear red-green glasses, and the test picture is decomposed by the anaglyph spectacles. The red halfmoon can be seen through the green glasses while it cannot be seen through the red glasses. Similarly, the green halfmoon can be seen through the red glasses while it cannot be seen through the green glasses. The subject is asked to compare the size of the two halfmoons. No. 0 test picture on page 1 is usually tested in the first step. If both parts look in equal size, no aniseikonia exists. If the green part seems larger than the red part, the test should start from No. 1 on page 2, and then No. 2 and so on, until the two halfmoons appear to be equal size. The number of the test picture is the aniseikonia percent of the patient. If the red part seems larger than the green part, the test page should turn to page 6, and testing should start from No. 1’, and then No. 2’ and so on, until the two halfmoons appear to be equal size. The number of the test picture is the aniseikonia percent of the patient.
The test can be conducted in the vertical, horizontal, or oblique meridians. The book should be tilted to a certain angle according to the test purpose.
Using an auto-stereoscopic smartphone to imitate the Awaya new aniseikonia test
The test equipment adopted a naked-eye, 3D, glasses-free, PPTV King7s mobile phone (Shanghai Gallop Entertainment Media Technology Co., Ltd. China). The test symbols were a pair of halfmoons. In the Awaya test, the colors of the halfmoons are red and green, and a pair of red-green anaglyph glasses helps to divide the images. In this experiment, the original lenses of the anaglyph glasses were unloaded and inserted into two circular frames for trial lenses after grinding. When conducting the Awaya test, the green and red trial lenses are inserted into the left and right sides of the trial frame, respectively. No red-green spectacles were needed to view 3D images on a naked-eye 3D smartphone. The shapes and sizes, but not the colors of symbols were displayed on the smartphone, and all imitated the Awaya test. The halfmoons displayed on the screen were black, and the background was white (Figure 1).
All test distances were set at 40 cm. When using the 3D smartphone, the subject first observed with their right eye while keeping their left eye closed. The position of the smartphone was adjusted slightly until the letter “R” could be seen. Holding this position, the left eye was opened and the right eye closed, causing “R” to vanish and “L” to appear. The position of the smartphone and the subject’s head was held still during the test procedure. Then, the test procedure proceeded in the same way as the Awaya test. The no. 0 test picture was used first. The subject was asked to compare the size of the left and the right halfmoon. If both parts appeared equal in size, there was no aniseikonia. If the right part seemed larger than the left one, the test was started from No. 1, then No. 2 and so on until the two halfmoons appeared equal in size. If the right part seemed smaller than the left part, the test was started from No. 1’, then No. 2’ and so on, until the two halfmoons appeared equal in size. The number of the test picture was considered the aniseikonia percent of the patient.
Inducing aniseikonia
Subjects
Ten subjects (3 males and 7 females), aged 21–28 (24.6±2.5) years, were recruited. None of the study participants had severe ametropia, amblyopia, strabismus, or anisometropia. The best corrected visual acuity was set at a minimum of 0 logMAR for each eye. The stereoacuity was a minimum of 40 arcsec, as measured by the Fly Stereo Acuity Test (Vision Assessment Corporation, Elk Grove Village, IL, USA).
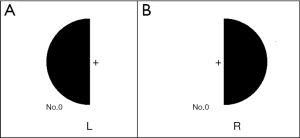
Inducing aniseikonia with trial frame and trial lenses
Three out of the ten participants recruited for the tests had myopia. All the myopes wore soft contact lenses to correct refractive error. A trial frame was utilized to induce aniseikonia (Figure 2). The trial frame used had 4 cells for each eye, with the distance between the forwardmost and rearmost cells being approximately 16 mm. With the appropriate calculation of the lens power, some degree of “size lens” could be created (1). However, 4 pairs of combinations were chosen to create different magnification rates: group 1, 6.3% [+4.00DS vs. −4.25DS (+4.00 DS was inserted into the forwardmost cell of the trial frame while −4.25DS was inserted into the rearmost cell, similarly hereafter)]; group 2: 10% (+5.00DS vs. −5.50DS); group 3: −6.3% (−4.00DS vs. +3.75DS); and group 4: −8.3% (−6.00DS vs. +5.50DS). The actual magnification rate might have changed due to the influences of several factors; e.g., different rear vertex distances, inclination angles etc. However, the purpose of this combination was only to create some degree of aniseikonia to enable a comparison of the examination results of the Awaya new aniseikonia test and the naked-eye 3D glasses-free smartphone test. The exact value of the magnification rate was ignored.
Test aniseikonia in clinic
The test was carried out in the Optometry Department in the Second Hospital of Jilin University. Forty subjects (18–35 years old) whose anisometropia was higher than 2.00D without astigmatism were recruited (range: 2.00D to 4.75D). Worth 4-dot test was used to exclude monocular suppression when finishing routine subjective refraction with a phoropter. The test was carried out with a trial frame for loading the correct lenses. The test sequence of the Awaya new aniseikonia test or auto-stereoscopic smartphone test was set randomly. The test interval was no less than 5 min.
All participants provided their informed written consent before undergoing the experiment. The research protocol observed the tenets of the Declaration of Helsinki and was approved by the ethics committee of the Second Hospital of Jilin University (No. 2017-89).
Statistical analysis
Wilcoxon signed-rank test was used to explore the differences between groups. The Bland-Altman method was used to evaluate the agreement between the two tests (MedCalc Statistical Software, version 17.6, MedCalc Software bvba, Ostend, Belgium).
Results
Test for inducing aniseikonia
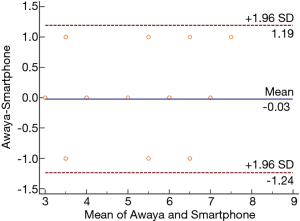
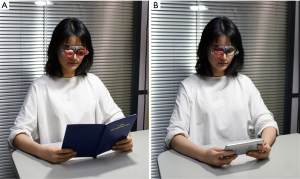
The results are shown in Table 1. No significant difference was found between the results of the Awaya New Aniseikonia Test and the auto-stereoscopic smartphone test (Wilcoxon signed-rank test, P=0.85). Bland-Altman plots showed that the difference between the two tests was less than or equal to 1% (Figure 3). Note that 1% is the minimum test step range of the Awaya new aniseikonia test.
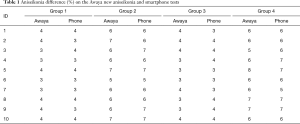
Full table
Test for anisometropia
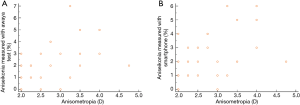
The amount of anisometropia was correlated with the quantity of aniseikonia measured with the Awaya new aniseikonia test [Spearman’s coefficient of rank correlation (rho) =0.588, P<0.01].The scatter diagram is shown in Figure 4A. Similarly, the amount of anisometropia was also correlated with the quantity of aniseikonia measured with the auto-stereoscopic smartphone [Spearman’s coefficient of rank correlation (rho) =0.606, P<0.01]. The scatter diagram is presented in Figure 4B. No significant difference was found between the results of the Awaya new aniseikonia test and the auto-stereoscopic smartphone test (Wilcoxon signed-rank test, P=0.53). Bland-Altman plots showed that the difference between the two tests was less than or equal to 1% (Figure 5).
Discussion
The Awaya new aniseikonia test is widely used in the clinic. The majority of the recent literature related to evaluating aniseikonia using this test. However, there still different instruments to measure aniseikonia in the clinical or in research field. The space eikonometer is considered to be the gold standard in this domain. The original space eikonometer produced by the American Optical Company (1), was designed as a laboratory unit with a test area of 5 square feet. A tabletop unit was then manufactured for office use. The general structure of the space eikonometer was an enclosed box, containing a red cross set in the center, two vertical green lines, and two white lines set in the front, and the rear inside of the box, respectively. A set of sized lenses was used to produce magnification in two rotatable primary meridians. If aniseikonia was present, the cross would be rotated or tilted. Adjusting the lens size could correct the rotation and return it to normal status. The size of the lens represented the amount of aniseikonia. As a condition to perform the test, the stereopsis of the subject should be relatively good. For research purposes, space eikonometer is still considered the gold standard for aniseikonia measurement. However, it is no longer commercially available. The standard eikonometer is a project instrument with a polarizing filter to separate the right and the left eye. Also, the eikonometer can help size lenses to eliminate aniseikonia and restore the misaligned lines to normal situations (1,3). This method also relies on binocular perception, but does not rely on stereoscopic depth perception as the space eikonometer does.
The Awaya new aniseikonia test was conducted with anaglyph glasses to separate the two eyes. The naked-eye, 3D, glasses-free, PPTV King7s mobile phone used in this experiment adopts parallax barrier technology (24), which uses a switched liquid crystal screen to produce an ultrathin vertical grating pattern that divides the images seen by the eyes. Although the methods of dividing the binocular image were different, the size of the test pattern remained the same. The test results were in high agreement.
Some literature reports that the Awaya new aniseikonia test underestimates the amount of aniseikonia (23,25). This phenomenon was also apparent in our test. However, what we used was not an accurate quantitative method as the “size lens” was. The emphasis of the testing was to detect the difference between the tests. The color may affect the aniseikonia test result because of the size-color illusion, which means the perceived size of two physically identical areas varies with their hue (26,27). The hue and brightness difference between the two eyes using red-green anaglyphs may also affect the comparison of the two halfmoons in the test (27). However, this effect did not influence the test result of our experiment. In this regard, the auto-stereoscopic smartphone test imitated the Awaya new aniseikonia test perfectly.
Clinically, one diopter (D) or more of a difference in refractive power between the two eyes in corresponding meridians is considered to cause symptoms (1). However, the type of anisometropia was only spherical in our experimental design. The amount of anisometropia was no less than 2 D. The inclusion criteria aimed to simplify the test procedure and increase the opportunity to detect aniseikonia. The purpose of this study was to compare the outcome of the two instruments. Normally, the amount of anisometropia was correlated with the quantity of aniseikonia in the test range. The correlations were to express a tendency. In our experiment, the maximum anisometropia was 4.75 D and occurred in an 18-year-old first-year student whose aniseikonia test result was 2%; meanwhile, the maximum aniseikonia result was 7% and occurred in a 25-year-old man tested by the Awaya test with the amount of anisometropia being 3.25 D. Many factors affect the test result of aniseikonia in real life.
There are advantages to using a naked-eye 3D smartphone to evaluate aniseikonia in the clinic: (I) it is easy to carry, as most people already carry a cell phone. (II) The naked-eye 3D technology eliminates the need to use spectacles, but most people in China encounter refractive errors that require spectacles. Wearing additional glasses on their existing ones is uncomfortable and inconvenient.
In the experiment, our test was only conducted in the vertical direction. The Awaya new aniseikonia test can measure any one of the meridians by rotating the booklet. However, the smartphone must be kept in a horizontal direction during the whole test procedure. If the aniseikonia checking requires a different n degree, the pattern should be re-drawn at the given angle. Fortunately, this is not complicated to do.
Conclusions
The auto-stereoscopic smartphone can be an effective tool for evaluating aniseikonia.
Acknowledgments
Funding: Funding was received from the Jilin Provincial Science & Technology Department, China (No. 20190303150SF), and the Jilin Provincial Special Fund for Talent Team (No. 2019SCZT030).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was approved by the ethics committee of the Second Hospital of Jilin University (No. 2017-89).
References
- Taylor Kulp MA, Raasch TW, Polasky M. Patients with Anisometropia and Aniseikonia. In: Benjamin WJ. Borish's Clinical Refraction. 2 edition. Butterworth-Heinemann, 2006:1479-508.
- Okamoto F, Sugiura Y, Okamoto Y, et al. Aniseikonia in various retinal disorders. Graefes Arch Clin Exp Ophthalmol 2017;255:1063-71. [Crossref] [PubMed]
- South J, Gao T, Collins A, et al. Aniseikonia and anisometropia: implications for suppression and amblyopia. Clin Exp Optom 2019. [Crossref] [PubMed]
- Gobin L, Rozema JJ, Tassignon MJ. Predicting refractive aniseikonia after cataract surgery in anisometropia. J Cataract Refract Surg 2008;34:1353-61. [Crossref] [PubMed]
- Katsumi O, Miyajima H, Ogawa T, et al. Aniseikonia and stereoacuity in pseudophakic patients. Unilateral and bilateral cases. Ophthalmology 1992;99:1270-7. [Crossref] [PubMed]
- You F, Shen H, Li S. Supracapsular implantation with optic capture of posterior chamber intraocular lens in Chinese children with aphakic after traumatic cataract. Ann Eye Sci 2017;2:58. [Crossref]
- Benegas NM, Egbert J, Engel WK, et al. Diplopia secondary to aniseikonia associated with macular disease. Arch Ophthalmol 1999;117:896-9. [Crossref] [PubMed]
- Moon BG, Yang YS, Chung H, et al. Correlation between macular microstructures and aniseikonia after idiopathic epiretinal membrane removal. Retina 2019. [Crossref] [PubMed]
- Hirata A, Nakada H, Mine K, et al. Relationship between the morphology of the foveal avascular zone and the degree of aniseikonia before and after vitrectomy in patients with unilateral epiretinal membrane. Graefes Arch Clin Exp Ophthalmol 2019;257:507-15. [Crossref] [PubMed]
- Takabatake M, Higashide T, Udagawa S, et al. Postoperative changes and prognostic factors of visual acuity, metamorphopsia, and aniseikonia after vitrectomy for epiretinal membrane. Retina 2018;38:2118-27. [Crossref] [PubMed]
- Ichikawa Y, Imamura Y, Ishida M. Associations of aniseikonia with metamorphopsia and retinal displacements after epiretinal membrane surgery. Eye (Lond) 2018;32:400-5. [Crossref] [PubMed]
- Tanikawa A, Shimada Y, Horiguchi M. Comparison of visual acuity, metamorphopsia, and aniseikonia in patients with an idiopathic epiretinal membrane. Jpn J Ophthalmol 2018;62:280-5. [Crossref] [PubMed]
- Murakami T, Okamoto F, Sugiura Y, et al. Changes in aniseikonia and influencing-factors following successful macula-off retinal detachment surgery. Sci Rep 2019;9:11588. [Crossref] [PubMed]
- Okamoto F, Sugiura Y, Okamoto Y, et al. Aniseikonia and Foveal Microstructure after Retinal Detachment Surgery. Invest Ophthalmol Vis Sci 2014;55:4880-5. [Crossref] [PubMed]
- Lee HN, Lin KH, Tsai HY, et al. Aniseikonia following pneumatic retinopexy for rhegmatogenous retinal detachment. Am J Ophthalmol 2014;158:1056-61. [Crossref] [PubMed]
- Frisén L, Frisén M. Micropsia and visual acuity in macular edema. A study of the neuro-retinal basis of visual acuity. Albrecht Von Graefes Arch Klin Exp Ophthalmol 1979;210:69-77. [Crossref] [PubMed]
- Sjöstrand J, Anderson C. Micropsia and metamorphopsia in the re-attached macula following retinal detachment. Acta Ophthalmol (Copenh) 1986;64:425-32. [Crossref] [PubMed]
- Hisada H, Awaya S. Aniseikonia of central serous chorioretinopathy. Nihon Ganka Gakkai Zasshi 1992;96:369-74. [PubMed]
- Nakashizuka H, Kitagawa Y, Wakatsuki Y, et al. Prospective study of vitrectomy for epiretinal membranes in patients with good best-corrected visual acuity. BMC Ophthalmol 2019;19:183. [Crossref] [PubMed]
- Kim JH, Kang SW, Kong MG, et al. Assessment of retinal layers and visual rehabilitation after epiretinal membrane removal. Graefes Arch Clin Exp Ophthalmol 2013;251:1055-64. [Crossref] [PubMed]
- Kehler LA, Fraine L, Lu P. Evaluation of the aniseikonia inspector version 3 in school-aged children. Optom Vis Sci 2014;91:528-32. [Crossref] [PubMed]
- Weise KK, Marsh-Tootle W, Corliss D. Evaluation of computer-based testing for aniseikonia in children. Optom Vis Sci 2010;87:883-9. [Crossref] [PubMed]
- Antona B, Barra F, Barrio A, et al. The validity and repeatability of the New Aniseikonia Test. Optom Vis Sci 2006;83:903-9. [Crossref] [PubMed]
- Lv GJ, Wang QH, Zhao WX, et al. 3D display based on parallax barrier with multiview zones. Appl Opt 2014;53:1339-42. [Crossref] [PubMed]
- McCormack G, Peli E, Stone P. Differences in tests of aniseikonia. Invest Ophthalmol Vis Sci 1992;33:2063-7. [PubMed]
- Yoo HS, Smith-Jackson TL. Colour size illusion on liquid crystal displays and design guidelines for bioinformatics tools. Behav Inform Tech 2011;30:775-85. [Crossref]
- García-Pérez MA, Peli E. Aniseikonia Tests: The Role of Viewing Mode, Response Bias, and Size-Color Illusions. Transl Vis Sci Technol 2015;4:9. [Crossref] [PubMed]