Left destroyed lung caused by a pen cap in the left lower lobe bronchus “swallowed” 25 years ago
Introduction
Tracheobronchial foreign body aspiration (FBA) often involves children under three years of age and occurs more rarely in school-age children and teenagers (1,2). FBA is often overlooked by caregivers and clinicians, which leads to delayed diagnosis or misdiagnosis resulting in various pulmonary complications. In delayed cases, diagnosis and treatment are more difficult and pulmonary resection is necessary for patients with severe pulmonary complications and irreversible pulmonary damage (3). In this case report, we present a left lung destruction in a middle-aged female who was misdiagnosed with tuberculosis more than 20 years prior. This patient ultimately underwent left pneumonectomy, and the etiology of the destroyed lung was found to be an intrabronchial pen cap “swallowed” 25 years ago.
Case presentation
A 32-year-old female was admitted to the department of thoracic surgery with chronic cough and blood-tinged sputum for over 20 years and paroxysmal hemoptysis for one year. She had no fever, night sweats, or weight loss. The medical history was remarkable for cavitary lesions of the left lung upon chest radiography, and she was diagnosed with tuberculosis in a local hospital as a child, one year after the initiation of cough. Following this diagnosis, she received anti-tuberculosis therapy for 18 months. The cavitary lesions of the left lung did not recover however, and the cough became persistent with temporary remission only after antibiotic and symptomatic therapy. One year ago, her symptoms worsened, and she developed episodic hemoptysis. She was then referred to the department of thoracic surgery after conservative medical management failed to control her symptoms. She had not undergone bronchoscopy prior to this admission.
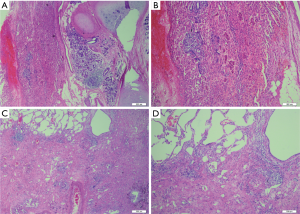
On physical examination, the left thoracic cavity was found to be collapsed, and breath sounds of the left hemithorax were absent. Blood tests showed that the white blood cell count, erythrocyte sedimentation ratio, and C-reactive protein were all normal. Repeated sputum smears and cultures found no acid-resistant bacillus or other pathogenic bacteria. Chest computed tomography (CT) scan revealed that the left lung was almost completely destroyed, the left main bronchus was stenosed, and the mediastinal structures were shifted toward the affected side (Figure 1). On flexible bronchoscopy, severe scarring and stenosis of the lower segment of the left main bronchus was found, and the distal structures were not visible. Thus, the diagnosis of left destroyed lung was made, and left pneumonectomy was recommended.
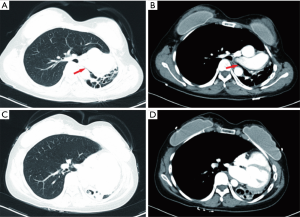
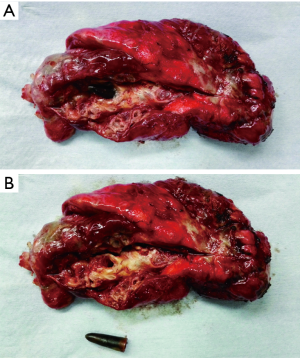
Considering the diagnosis of tuberculosis despite there being no etiological evidence for it, a three-month diagnostic anti-tuberculosis therapy was administered preoperatively. The operation was performed via a left posterolateral thoracotomy. Intraoperative exploration revealed complete collapse of the left lung with partial adhesion of the pleura. After dissection of the pleural adhesion, left pneumonectomy was performed uneventfully. The dissected surface of the resected specimen revealed granulation tissue hyperplasia of the left main bronchus and left lower lobe bronchus, and extensive consolidation of the pulmonary tissue without caseous necrosis or abscesses. Additionally, an unexpected conical foreign body was found embedded in granulation tissue of the proximal portion of the left lower lobe bronchus (Figure 2A). The foreign body was identified to be a plastic pen cap 0.5 cm in diameter and 2 cm in length (Figure 2B). Postoperative histological examination of the specimen revealed bronchiectasis and chronic inflammation of the bronchi as well as consolidation and fibrous scar hyperplasia of the pulmonary tissue (Figure 3), which, taken together, is consistent with changes secondary to long-term obstruction of the intrabronchial foreign body.
The patient was transferred to the intensive care unit after the operation and was sent back to the general ward on postoperative day (POD) 1. Upon further questioning of her medical history, she recalled “swallowing” a pen cap about 25 years ago and developing frequent cough with blood-stained sputum from then on. However, her parents did not pay attention to this condition and did not seek medical care immediately. As mentioned above, she was misdiagnosed with tuberculosis in a local hospital one year after becoming symptomatic. However, acid-resistant bacillus test of the sputum was persistently negative.
The patient experienced right pulmonary infection postoperatively, which was cured by antibiotic therapy using moxifloxacin and piperacillin. The chest tube was removed on POD 5. She was discharged home on POD 30. At 3-month follow-up, she was in good condition without dyspnea, cough, or hemoptysis.
iMDT discussion
Discussion among physicians from West China Hospital Sichuan University
As a common and life-threatening emergency in children, FBA should be promptly diagnosed and treated. If the diagnosis is established early, the majority of foreign bodies can be removed through bronchoscopy, and the prognosis is typically good (4). Delayed diagnosis of FBA, however, occurs frequently (5). According to a retrospective analysis of 1,015 cases, diagnosis of FBA was delayed by more than a week in 29% of cases and by more than a month in 10% (6). In cases of delayed diagnosis, the time between aspiration and diagnosis ranged from several days to decades. In our case, the foreign body was found 25 years after inhalation. To the best of our knowledge, this is the second longest delay in diagnosis, and is only exceeded by a reported foreign body retention of 40 years (7).
Department of Respiratory Medicine
A witnessed aspiration event is the most important indicator when making an early diagnosis of FBA and can be elicited in 80% of cases (8,9). Caregivers may not note or remember the choking events, and the children may not reveal a history of aspiration owing to lack of speech, misunderstanding, or fear. As in our case, the girl misunderstood the aspiration event as “swallowing a pen cap”, and her parents also did not pay attention to the sudden onset of the cough.
The early clinical manifestations of FBA are usually acute and nonspecific, including coughing, choking, and dyspnea (4). Chest radiograph findings of FBA may be normal, though abnormal findings including air trapping, atelectasis, and pneumothorax can be present. However, none of these features is specific for FBA, and only about 16% of aspirated foreign bodies are radiopaque (3,9). Thus, physicians may overlook FBA in patients presenting with atypical symptoms and aspiration history, especially when the chest radiograph findings are normal (5,7). Consequently, bronchoscopy would not be typically performed.
If the FBA is not removed in time, early symptoms may disappear. The persistent existence of a foreign body in the airway may result in progressive symptoms and complications including chronic cough or wheezing, recurrent pneumonia, repeated hemoptysis, bronchiectasis, and atelectasis, which make the diagnosis even more elusive and may be misdiagnosed as other respiratory diseases (10,11). Otherwise, if the FBA is detected in time, it can be removed through the fiber-optic bronchoscope with less complications and a better prognosis. In our case, chest radiography revealed cavitary lesions in the left lung and a diagnosis of tuberculosis was made when the patient sought medical care one year after the aspiration occurred. It is unusual for FBA to mimic cavitary tuberculosis, and similar cases are exceedingly rare.
Department of Thoracic Surgery
The treatment choices of delayed-diagnosed FBA depend on length of foreign body retention and degree of respiratory complications. According to a retrospective analysis of 121 cases of late-diagnosed foreign body, 98 cases were successfully treated with bronchoscopy, while other 23 cases (19%) were treated by surgery (4). If the foreign body remains in the airway for a relatively short duration, and the complications are mild, bronchoscopic removal should be considered as the preferred choice, with bronchotomy being a possible supplementary procedure if bronchoscopic removal fails. However, for patients with severe respiratory complications and irreversible pulmonary damage, surgical resection should be performed promptly to prevent occurrence of lethal events, like septic pyemia and hemorrhage (4). In our case, even though the foreign body was located in the lower lobe bronchus, long-term inflammation and granulation hyperplasia surrounding the foreign body caused stenosis of the left main bronchus and finally resulted in a destroyed lung. In this case, pneumonectomy would be unavoidable even if the foreign body was identified prior to surgery.
Several issues regarding the diagnosis and treatment of this patient were further discussed as follows.
Question 1: In our case, the patient’s initial imaging finding was lung cavity that were misdiagnosed as tuberculosis. What are the main points for the differential diagnosis of pulmonary cavity lesions in children?
Expert opinion 1: Dr. Khosro Hekmat
Cavities in the lung are present in a wide variety of infectious and non-infectious processes. The differential diagnosis of pulmonary “cavities” in children includes pneumatoceles, bronchiectatic cysts, bullous emphysema, congenital cysts, and intrapulmonary sequestration. True cavities are the result of inflammation, neoplasms, or vascular insufficiency with ischemic necrosis. The processes that lead to infectious cavities may be divided into acute pyogenic infection and granulomatous inflammation. Our case of granulomatous infection caused by foreign body aspiration may also produce radiologic findings of chronic disease including mycobacterial infection.
Expert opinion 2: Dr. Erin M. Corsini & Dr. Mara B. Antonoff
As with adults, the differential diagnosis of a cavitary lung lesion in the pediatric population is broad, and may span a variety of etiologies. Infectious causes may be bacterial, fungal, parasitic, or typical or atypical mycobacterium. Manifestations of such infections may commonly include abscesses, aspergillomas, or tuberculosis (12). It may also be important to consider septic emboli, with resultant microabscesses, in the differential diagnosis, if systemic symptoms are present (13). In the AIDS population, cavitary lesions may also be observed with pneumocystis jirovecii infections (14). Thin-walled cavitary lesions can be seen with langerhans cell histiocytosis, and should be considered if cutaneous or osseous lesions are present, though other lesions may manifest elsewhere in the body (15). Congenital malformations may include congenital lobar emphysema, congenital cystic adenomatoid malformation, pleuropulmonary blastoma, bronchogenic cyst, or pulmonary sequestration (16).
As in this case, in which the patient presented for evaluation as an adult, additional diagnoses may be considered in this population, including malignancy or autoimmune cause. Malignancy may be of primary lung etiology or metastatic origin. If metastatic, tumors of the gastrointestinal tract, breast, or sarcomatous disease are most likely to cavitate (17). Lastly, autoimmune disease, such as sarcoidosis, rheumatoid arthritis or granulomatosis with polyangiitis, may also be considered in adult populations (18-20).
Question 2: Our case was a left lung destruction that was accidentally discovered as a foreign body in the trachea during the surgery. What are the special preoperative preparations for this type of patient, do we need to give anti-infective therapy before the surgery?
Expert opinion 1: Dr. Khosro Hekmat
In this case, antibiotic therapy before surgery is not necessary, as it is a chronic disease process.
Expert opinion 2: Dr. Erin M. Corsini and Dr. Mara B. Antonoff
In the case of a destroyed lung, definitive treatment requires surgical resection, and, thus, operative management should not be delayed while providing systemic antibiotic therapy. Important aspects of preoperative planning, however, include assurance of adequate nutritional status as well as consideration of possible need for muscle flaps to provide well-vascularized tissue for buttressing airways or occupying dead space. With regard to the choice of perioperative antibiotics, they should include broad-spectrum antimicrobials in the instance of a destroyed lung. Intraoperatively, cultures should be taken, including those for aerobes, anaerobes, fungi, and atypical/typical mycobacteria. Broad-spectrum antibiotics should be continued until additional culture data are available, at which time antibiotic coverage may be narrowed to cover the target organism(s).
Question 3: Missed diagnosis or misdiagnosis of tracheal foreign bodies could lead to severe consequences. What are the diagnostic points for children with tracheal foreign bodies without typical clinical manifestations?
Expert opinion 1: Dr. Khosro Hekmat
The right main bronchus is wider and runs more vertically, thus foreign body aspiration is more frequently on the right side. Sudden onset of cough after a choking episode suggests foreign body aspiration. However, a proportion of patients may have a negative history in unrecognized aspiration. The diagnosis of FBA should be kept in mind for children with acute onset of cough, cyanosis, localized wheezing, unilateral absence of breath sounds and stridor.
Expert opinion 2: Dr. Erin M. Corsini and Dr. Mara B. Antonoff
A high index of suspicion should be maintained, particularly if clinical signs or witnessed events are consistent with a potential aspiration event. If any signs or symptoms are consistent with FBA, a low threshold should be maintained for either axial imaging and/or bronchoscopy.
Conclusions
We present here a rare case of a destroyed lung caused by a pen cap remaining in the left lower lobe bronchus for 25 years, which was previously misdiagnosed as cavitary tuberculosis. Our case is a typical example of the grave consequence of the misdiagnosis of FBA, in which the patient finally underwent left pneumonectomy. To prevent delayed diagnosis and misdiagnosis of FBA, clinicians should maintain a high index of suspicion of FBA, and an early bronchoscopic examination should be considered in suspected cases.
Acknowledgments
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Gang W, Zhengxia P, Hongbo L, et al. Diagnosis and treatment of tracheobronchial foreign bodies in 1024 children. J Pediatr Surg 2012;47:2004-10. [Crossref] [PubMed]
- Zhang H, Xiao K, Hou X, et al. Comparison between tracheal foreign body and bronchial foreign body: a review of 1,007 cases. Int J Pediatr Otorhinolaryngol. 2012;76:1719-25. [Crossref] [PubMed]
- Chen X, Zhang C. Foreign body aspiration in children: Focus on the impact of delayed treatment. Int J Pediatr Otorhinolaryngol 2017;96:111-5. [Crossref] [PubMed]
- Duan L, Chen X, Wang H, et al. Surgical treatment of late-diagnosed bronchial foreign body aspiration: a report of 23 cases. Clin Respir J 2014;8:269-73. [Crossref] [PubMed]
- Ibrahim Sersar S, Hamza UA, AbdelHameed WA, et al. Inhaled foreign bodies: management according to early or late presentation. Eur J Cardiothorac Surg 2005;28:369-74. [Crossref] [PubMed]
- Saki N, Nikakhlagh S, Rahim F, et al. Foreign body aspirations in infancy: a 20-year experience. Int J Med Sci 2009;6:322-8. [Crossref] [PubMed]
- Limper AH, Prakash UB. Tracheobronchial foreign bodies in adults. Ann Intern Med 1990;112:604-9. [Crossref] [PubMed]
- Akelma AZ, Cizmeci MN, Kanburoglu MK, et al. An overlooked cause of cough in children: foreign body aspiration. J Pediatr 2013;163:292-3. [Crossref] [PubMed]
- Wang K, Harnden A, Thomson A. Foreign body inhalation in children. BMJ 2010;341:c3924. [Crossref] [PubMed]
- Abdulmajid OA, Ebeid AM, Motaweh MM, et al. Aspirated foreign bodies in the tracheobronchial tree: report of 250 cases. Thorax 1976;31:635-40. [Crossref] [PubMed]
- Cakir E, Torun E, Uyan ZS, et al. An unusual case of foreign body aspiration mimicking cavitary tuberculosis in adolescent patient: thread aspiration. Ital J Pediatr 2012;38:17. [Crossref] [PubMed]
- Walker CM, Abbott GF, Greene RE, et al. Imaging pulmonary infection: classic signs and patterns. AJR Am J Roentgenol 2014;202:479-92. [Crossref] [PubMed]
- Han D, Lee KS, Franquet T, et al. Thrombotic and nonthrombotic pulmonary arterial embolism: spectrum of imaging findings. Radiographics 2003;23:1521-39. [Crossref] [PubMed]
- Chong S, Lee KS, Yi CA, et al. Pulmonary fungal infection: imaging findings in immunocompetent and immunocompromised patients. Eur J Radiol 2006;59:371-83. [Crossref] [PubMed]
- Abbott GF, Rosado-de-Christenson ML, Franks TJ, et al. From the archives of the AFIP: pulmonary Langerhans cell histiocytosis. Radiographics 2004;24:821-41. [Crossref] [PubMed]
- Odev K, Guler I, Altinok T, et al. Cystic and cavitary lung lesions in children: radiologic findings with pathologic correlation. J Clin Imaging Sci 2013;3:60. [Crossref] [PubMed]
- Seo JB, Im JG, Goo JM, et al. Atypical pulmonary metastases: Spectrum of radiologic findings. Radiographics 2001;21:403-17. [Crossref] [PubMed]
- Castañer E, Alguersuari A, Andreu M, et al. Imaging findings in pulmonary vasculitis. Semin Ultrasound CT MR 2012;33:567-79. [Crossref] [PubMed]
- Kanıtez NA, Çelik S, Öner SY, et al. Cavitary pulmonary nodules in rheumatoid arthritis; case reports and review of the literature. Eur J Rheumatol 2018;5:65-68. [Crossref] [PubMed]
- Park HJ, Jung JI, Chung MH, et al. Typical and atypical manifestations of intrathoracic sarcoidosis. Korean J Radiol 2009;10:623-31. [Crossref] [PubMed]