Desirable training of endoscopic submucosal dissection: further spread worldwide
Introduction
Endoscopic mucosal resection (EMR), which consists of submucosal fluid injection, grasping and cutting the lesion by an electrocautery snare, has been widely accepted as the treatment for small (e.g., <2 cm) gastrointestinal (GI) neoplasms without metastasis. To overcome the size limitation, endoscopic submucosal dissection (ESD) has been developed, which consists of submucosal fluid injection, mucosal cutting around the lesion, and submucosal dissection beneath the lesion. Although ESD has advantages over EMR in terms of en bloc and curative resection rates (1), ESD has disseminated mainly in Asian countries (2), not in Western countries, partly due to lack of structured training systems for the meticulous and time-consuming technique with a long learning curve (3). In this narrative review, we would like to propose an appropriate training system of ESD for further spread worldwide as the standpoint of one of the leading centers in Japan.
Training system
Prerequisites for ESD operators
ESD trainees must begin their training by acquiring enough basic knowledge about ESD as well as fundamental managements of patients as gastroenterologists or GI surgeons: indications for ESD, how to set the electrosurgical generator, how to cope with adverse events, and so on. This kind of knowledge can be obtained by reading textbooks or asking mentors, so every trainee endoscopist can accomplish this first step if only they are serious about learning ESD. ESD is still a potentially risky procedure, and so it is imperative for ESD trainees to keep a positive attitude to acquire the sufficient knowledge and competent skills of ESD at all times. In this sense, we believe that not every endoscopist can stand at the start line of ESD training (4).
In terms of essential endoscopic skills, detection and precise diagnosis of GI neoplasms is absolutely necessary in order to put precise markings around the target lesions, and reliable techniques of accurate biopsy and hemostasis are also necessary in order to put ESD devices on the appropriate positions with a stable operative field during ESD. It is easy for the trainers to recognize the suitable trainees during routine endoscopy, just by checking stable and precise endoscopic manipulation for observation and biopsy. It is also desirable to obtain expertise in hemostasis as much as possible, because most of the difficulties regarding ESD procedures are related to uncontrollable hemorrhage (5). As an objective indicator for starting ESD trainees, we have reported that an endoscopist who has performed more than 1,000 cases of esophagogastroduodenoscopy (EGD) can acquire gastric ESD skills efficiently (6).
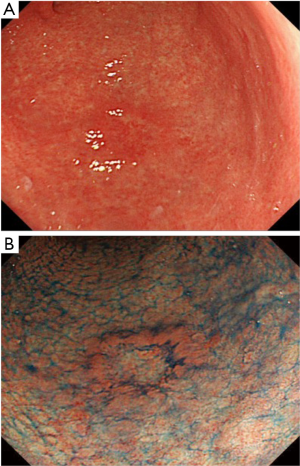
Precise diagnosis of a lesion outline is necessary for achieving complete resection. Recently there have been several reports about the efficacy of magnifying endoscopy with narrow-band imaging in determining the demarcation line of GI neoplasms (7,8), so it is advisable for ESD operators to be proficient in this kind of image-enhanced endoscopy. However, magnifying endoscopes are unavailable at most institutions in Western countries, so mastery of chromoendoscopy by using indigocarmine in the stomach & the intestine or iodine in the esophagus is essential for determining the lateral extent of lesions (9) (Figure 1).
Stepwise training system
The followings are widely accepted stepwise training system in Japan. The modification must be necessary according to the distribution of diseases and the degree of exposure to endoscopy in case of other countries.
- The first step is knowledge-based self-training and acquiring basic endoscopic skills as mentioned above;
- Before performing ESD for real human cases, trainees should go through training in ex vivo animal models (10). In Japan, the number of ex vivo models training before human cases under supervision of trainers is approximately five or less;
- Trainees should participate in ESD as an assistant as many times as possible (6). By assisting in ESD performed by trainers, trainees can observe an expert’s techniques at close range and learn not only the way to use devices but also strategy in the whole sequence in each case by moving their body and hands;
- Trainees can advance to a human gastric ESD case. Lesions of the gastric antrum are suitable for beginners, because antegrade endoscopic manipulation is possible and lesion elevation after injection in the antrum is usually good;
- Trainees can perform ESD for more difficult lesions in the stomach;
- The esophagus and the colon is thought to be more difficult organ than the stomach, so it is common that esophageal or colorectal ESD follows gastric ESD in Japan (4,11).
The minimal case load for a competent ESD operator is still unrevealed. As for gastric ESD, it has been reported that experience of at least 30 cases is required for a beginner to gain early proficiency (12,13). However, there have been other reports that the number of 30 cases is not enough for a competent ESD operator (5,6). Yamamoto et al. reported that in their study two of the three ESD operators could not achieve sufficient self-completion rate after 30 cases, so they inferred that more extensive experience is required before endoscopists can be considered to be proficient in ESD. Tsuji et al. analyzed four trainees’ learning curve for gastric ESD, and they concluded that even after 30 cases novice operators could not always complete gastric ESD. As a consensus, most Japanese experts seem to set the level of expertise at 50-100 cases of gastric ESD (3). As for colorectal ESD, Hotta et al. also reported that approximately 80 procedures should be carried out to acquire ESD skills adequate for consistent, successful removal of large colorectal tumors (14).
The learning curve is quite different between trainees with and without the close supervision by experts at the initial stage of trainees’ ESD procedures. Probst et al. reported the results of 91 cases of gastric ESD in a single German institution (15). In their study, their ESD procedures at the initial stage were supervised by two Japanese experts, and their treatment results were favorable: perforation occurred in only one case and the rate of en block resection without residual tumors was 74.1%. ESD needs complex endoscopic maneuvers associated with a high risk for procedural complications (perforation, bleeding), so the importance in supervision by experts is self-evident (5,6,12,16). However, Japanese experts are not always available at most institutions worldwide. Therefore, training in animal models must play a major role in ESD training at the initial stage.
Animal model training
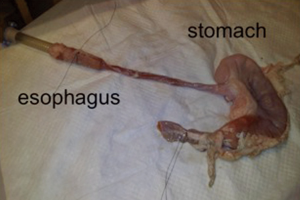
How to set ex vivo models is shown in the previous report by Parra-Blanco et al. (16). Figure 2 is an example of a harvested pig stomach and esophagus model.
In Japan, the case number of ex vivo training before starting a human case is inclined to be small, because each trainee can easily find out volunteer ESD trainers for supervision inside and outside his/her institution throughout Japan. However, in other countries, where very few endoscopists are proficient with ESD, patient-based training supervised by experts is almost impossible (9). Parra-Blanco et al. argued that the number of experimental resections before performing ESD in human cases should probably be as great as possible (10). According to their previous report, there existed a learning curve for gastric ESD in animal models after performing 15 cases of experimental resection (16).
In vivo animal models are better in that they simulate a real ESD condition; an organ movement associated with respiration, bleeding during submucosal dissection, and perforation. However, as a matter of course, such training must be carried out according to ethical principles and the law of each country.
An ex vivo animal model exerts a more powerful effect on training in esophageal or colorectal ESD than gastric ESD. In Japan, esophageal or colorectal ESD follows gastric ESD because of the technical difficulties: paradoxical movement, a thin muscular layer and an increased perforation risk. A learning curve in esophageal or colorectal ESD has not been clarified sufficiently, but according to Japanese experts’ opinions, trainees should start esophageal or colorectal ESD after performing at least 30 cases of gastric ESD (3,4,11,17). However, in most Western countries the incidence of gastric cancers is much lower than in Japan. Whereas, in those countries, esophageal or colorectal lesions are more inclined to be the targets for ESD. Therefore, ex vivo animal models play an important role on acquiring the skills.
In the future the development of new devices will make ESD much easier. However, at present, ESD is one of the most complex endoscopic procedures, and there are certain technical tricks and tips that are difficult to learn by oneself, and ESD involves maneuvers that have not been used during routine endoscopy examinations (16). Therefore, visiting to a high-volume center to observe ESDs performed by experts is the most recommendable step at the beginning of learning ESD (9). Many ESD experts in Japan can contribute to training in countries where there are few ESD experts, even when the trainees do not across the country borders (6).
Selecting an appropriate lesion for trainees
Education for trainees and clinical outcomes must be counterbalanced from an ethical viewpoint (6). In order to avoid ESD failure simply because of lack of skills, one of the important point is to select an appropriate lesion for trainees. Hirasawa et al. reported a risk assessment chart for curability of gastric ESD, and they concluded that small (≤20 mm), no-ulcerated lesions in the lower part of the stomach were the best candidates for initial-phase ESD trainees (18,19). On the other hand, the most difficult ones were large (>30 mm), ulcerated lesions in the upper part of the stomach: for which predicted probabilities of non-curability were calculated as 67.7% with a fitted logistic regression model. In Japan, ESD trainers take account of ESD difficulty from lesion characteristics, and assign each trainee an appropriate lesion.
As for esophageal or colorectal ESD, learning curve remains to be cleared, but we can speculate from several experts’ recommendation. Goda et al. recommended that esophageal ESD should be started from small (≤20 mm) and right-sided lesions in the middle esophagus (3). Blood and water, which obstruct an operative field, pool at the left esophageal wall during ESD, and so right-sided lesions are technically easier. The rectum is fairly straight and fixed in the pelvis with a wide working space, and so most experts recommended that trainees should begin colorectal ESD with the rectal lesions (11,20).
In Japan and other countries in East Asia, the incidence of gastric cancer is relatively high, but in Western countries, that is much lower and early gastric cancer is rarely detected (21). In this situation, Deprez et al. proposed that lesions in the rectum should be the first step of real ESD as well as those in the distal stomach (20). According to their statement, ESD should be performed in a step-up approach, starting with lesions presenting in the rectum or in the distal stomach, then colon, proximal stomach, and finally in the esophagus. This is one ideal model for ESD training system in Western countries.
Demand for establishing official training system
Even in Japan, there is no official training course sponsored by the Japan Gastroenterological Endoscopy Society (JGES) at present. Therefore, such a technical endoscopic skill as ESD is handed down to younger endoscopists by senior doctors at each hospital or by personal communication with other skilled endoscopists at other hospitals (4). So far these kinds of traditional training schemes in Japan have worked very well, but it is natural that an official training program in ESD should be structured in the future. An ideal role of authorized endoscopy organizations such as JGES must be (I) to govern or certify official training centers equipped with lecture spaces and simulation-based training workstations; (II) to release credentials for ESD trainees or trainers given by the authorized endoscopy organizations (4). Especially, certification of ESD trainers, which must become honor for their effort, is imperative.
Conclusions
ESD is a technically-demanding procedure, so a stepwise training system under close supervision by experts is desirable. In this sense, Japanese experts are willing to dedicate themselves to ESD training inside and outside Japan. At present ex vivo animal training models play an important role on acquiring ESD skills. An official training course is necessary in order to disseminate this technique worldwide.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Cao Y, Liao C, Tan A, et al. Meta-analysis of endoscopic submucosal dissection versus endoscopic mucosal resection for tumors of the gastrointestinal tract. Endoscopy 2009;41:751-7. [PubMed]
- Fujishiro M. Endoscopic submucosal dissection for stomach neoplasms. World J Gastroenterol 2006;12:5108-12. [PubMed]
- Goda K, Fujishiro M, Hirasawa K, et al. How to teach and learn endoscopic submucosal dissection for upper gastrointestinal neoplasm in Japan. Dig Endosc 2012;24 Suppl 1:136-42. [PubMed]
- Fujishiro M, Jung HY, Goda K, et al. Desirable training and roles of Japanese endoscopists towards the further penetration of endoscopic submucosal dissection in Asia. Dig Endosc 2012;24 Suppl 1:121-3. [PubMed]
- Yamamoto S, Uedo N, Ishihara R, et al. Endoscopic submucosal dissection for early gastric cancer performed by supervised residents: assessment of feasibility and learning curve. Endoscopy 2009;41:923-8. [PubMed]
- Tsuji Y, Ohata K, Sekiguchi M, et al. An effective training system for endoscopic submucosal dissection of gastric neoplasm. Endoscopy 2011;43:1033-8. [PubMed]
- Yao K, Anagnostopoulos GK, Ragunath K. Magnifying endoscopy for diagnosing and delineating early gastric cancer. Endoscopy 2009;41:462-7. [PubMed]
- Sumiyama K, Kaise M, Nakayoshi T, et al. Combined use of a magnifying endoscope with a narrow band imaging system and a multibending endoscope for en bloc EMR of early stage gastric cancer. Gastrointest Endosc 2004;60:79-84. [PubMed]
- Draganov PV, Gotoda T, Chavalitdhamrong D, et al. Techniques of endoscopic submucosal dissection: application for the Western endoscopist? Gastrointest Endosc 2013;78:677-88. [PubMed]
- Parra-Blanco A, González N, González R, et al. Animal models for endoscopic training: do we really need them? Endoscopy 2013;45:478-84. [PubMed]
- Niimi K, Fujishiro M, Goto O, et al. Safety and efficacy of colorectal endoscopic submucosal dissection by the trainee endoscopists. Dig Endosc 2012;24 Suppl 1:154-8. [PubMed]
- Gotoda T, Friedland S, Hamanaka H, et al. A learning curve for advanced endoscopic resection. Gastrointest Endosc 2005;62:866-7. [PubMed]
- Oda I, Odagaki T, Suzuki H, et al. Learning curve for endoscopic submucosal dissection of early gastric cancer based on trainee experience. Dig Endosc 2012;24 Suppl 1:129-32. [PubMed]
- Hotta K, Oyama T, Shinohara T, et al. Learning curve for endoscopic submucosal dissection of large colorectal tumors. Dig Endosc 2010;22:302-6. [PubMed]
- Probst A, Pommer B, Golger D, et al. Endoscopic submucosal dissection in gastric neoplasia - experience from a European center. Endoscopy 2010;42:1037-44. [PubMed]
- Parra-Blanco A, Arnau MR, Nicolás-Pérez D, et al. Endoscopic submucosal dissection training with pig models in a Western country. World J Gastroenterol 2010;16:2895-900. [PubMed]
- Ohata K, Ito T, Chiba H, et al. Effective training system in colorectal endoscopic submucosal dissection. Dig Endosc 2012;24 Suppl 1:84-9. [PubMed]
- Hirasawa K, Kokawa A, Kou R, et al. Determining early gastric cancer lesions appropriate for endoscopic submucosal dissection trainees: a proposal related to curability. Dig Endosc 2012;24 Suppl 1:143-7. [PubMed]
- Hirasawa K, Kokawa A, Oka H, et al. Risk assessment chart for curability of early gastric cancer with endoscopic submucosal dissection. Gastrointest Endosc 2011;74:1268-75. [PubMed]
- Deprez PH, Bergman JJ, Meisner S, et al. Current practice with endoscopic submucosal dissection in Europe: position statement from a panel of experts. Endoscopy 2010;42:853-8. [PubMed]
- Everett SM, Axon AT. Early gastric cancer in Europe. Gut 1997;41:142-50. [PubMed]