Peroral endoscopic myotomy for esophageal achalasia
Background
The concept of natural orifice transluminal endoscopic surgery (NOTES) is widely accepted all over the world. The combination of the basic principle of the endoscopy and surgery make the marvelous concept of the less invasive surgical intervention. Peroral endoscopic myotomy (POEM) was recently introduced as the alternative treatment of Achalasia. Inoue H. (1) stated first POEM series in 2010 and widely spread to all over the world. Nowadays more than two thousand cases of POEM procedure had successfully done.
Achalasia is one of the esophageal motility disorders which impair relaxation of lower esophageal sphincter. In the North America, the estimated prevalence and incidence is 10.82 cases per 100,000 and 1.63 cases per 100,000 per year respectively (2). The choices of treatment are varies from medication to surgery. POEM is safe, scarless, and able to perform in various type of achalasia. It may replace standard procedure in the future.
Indication of POEM
Patients
All patients who diagnosed achalasia can be candidate for POEM. Since there is no direct contraindication of this procedure. The various types of achalasia and esophageal abnormalities are candidated for this procedure.
Disease condition
POEM can be performed in all types of achalasia [categorized by high resolution manometry (HRM)] especially in tortuous dilated sigmoid achalasia which is contraindication to surgical myotomy. Sigmoid achalasia was successfully performed more than sixty cases without complications in our series.
Previous procedures
POEM was indicated in prior endoscopic intervention or surgical myotomy.
Even though palliative ballon dilatation in dysphagia patients makes some fibrosis, the following POEM is safe and feasible. The prior surgery or POEM is also possible to re-perform without any difficulty. Eleven cases of previous surgical myotomy and ten cases of second POEM were performed without any complications.
Equipments
A forward-viewing endoscope of outer diameter 9.8 mm, which is designed for routine upper gastrointestinal screening is used with a transparent distal cap attachment (DH-28GR, Fujiflim). This distal attached cap provided a better endoscopic vision even in submucosal space. With the smooth tapering cap, it takes the advantage to penetrate through the narrow part of submucosal tunnel. Air ventilation slit was designed to release smoke and provided clear vision during the procedure.
Mixture of 0.9% normal saline with 0.3% indigo carmine dye is usually used for submucosal injection. The concentration depends on the operator preference. This mixture offers a good plane for dissection and prevented unexpected injury to esophageal mucosa.
Injection needle: initially normal saline is injected with a 25 gauge injection needle. After that injection is repeated injection in the submucosal space by injection spray (non-needle type).
A triangle-tip knife (TT knife) (KD-640L, Olympus) was used to dissect the submucosal tissue and to divide circular muscle bundles. The maximum diameter for insertion portion of KD-640L is 2.6 mm.
A coagulating forceps (Coagrasper, FD-411QR; Olympus) is used for homeostasis and coagulated large vessels.
For electrosurgical energy generator, a VIO 300D electrogenerator (ERBE, Tübingen, Germany) is recommended. Generator mode of Spray coagulation in ERBE300D allows non-contact tissue dissection. It makes submucosal dissection much easier, faster and less bleeding.
Carbon dioxide insufflation is insufflated during the procedure with a CO2 insufflator (UCR; Olympus). CO2 insufflator with a regular insufflating tube (MAJ-1742; Olympus) offers controlled gas feeding of 1.2 liter/minute during procedure. Endoscopic CO2 insufflation is beneficial for reducing the risk of both mediastinal emphysema and air embolization. During the procedure, the air insufflation had been strictly closed. If not, the pressure of air insufflation will overcome the carbon dioxide pressure resulted in complication, e.g., pneumomediastinum, pneumoperitoneum. CO2 insufflation is safe, rapidly absorption, decrease intra procedural, post procedural pain and recovery time (3-5). The CO2 insufflation is safety as regular usage in laparoscopic and thoracoscopic surgery.
Gentamicin solution: 40 mg of Gentamicin diluted by 0.9% NSS 20 cc was injected before closing mucosal opening as a local antibiotic.
For final closure of the mucosal entry site, hemostatic clips (EZ-CLIP, HX-110QR; DF Olympus) are applied. Mucosal entry must securely be closed to avoid leakage of esophageal content into mediastinum.
Preoperative evaluation
Preoperatively, patients are evaluated with a history and physical examination, upper endoscopy, timed barium esophagogram (TBE), CT scan and HRM. TBE was performed using a 200-mL oral bolus of low-density barium, with radiographs taken at 1, 2, and 5 min after swallowing. CT scan is used not only to judge the degree of esophageal dilatation, but also to provide information on the anatomical features of adjacent structures. HRM was performed using a standard technique (6), and interpreted according to the Chicago Classification of esophageal pressure topography (7). An Eckardt symptom score (8) (which measures frequency of dysphagia, regurgitation and chest pain, and amount of weight loss, each on a scale of 0-3 resulting in a total scale of 0-12 with higher scores indicating more severe disease) and Vaezi symptom score (9) (which measure the height of barium column during TBE) were recorded preoperatively for POEM patients.
POEM operative technique
Patient is kept fasting overnight. Prior procedure started, residual food and liquid was clear to guarantee clear endoscopic view and avoided aspiration during induction of anaesthesia. The large channel endoscope (GIF-1T240, Olympus) is used for suction and irrigation with normal saline until clear. The antiseptic solution irrigation is not necessary. Prophylaxis intravenous antibiotic, 3rd generation cephalosporin is delivered beforehand.
Step 1: endotracheal intubation and CO2 insufflation
Patient was lying supine on the table with general anaesthesia. Positive pressure ventilation is recommended for this procedure to prevent severe mediastinal emphysema. In our series, pneumoperitoneum occurred in eight cases. The abdomen was left exposed in order to detect abdominal distention and probably abdominal compartment syndrome (Figure 1). When abdominal wall is excessively extended, abdominal paracentesis using injection needle is the most effective to release abdominal pressure (Figure 2).
Step 2: creation of a submucosal tunnel mucosal entry
A total of 10 mL normal saline with 0.3% indigo carmine mixture is injected to the mucosa as a wheal before triangular knife is applied to open the mucosal surface (Scheme 1A). The recommended incision is anterior wall usually between 11 and 2 o’clock. A 2-cm longitudinal mucosal incision was made on the mucosal surface to create a mucosal entry to the submucosal space (Endo cut Q mode, 50 W, effect 3). If the patient happens to have abnormal contraction of esophageal upper third much longer myotomy is expected. Longer myotomy can effectively control chest pain caused by spasm of hypertrophied circular muscle.
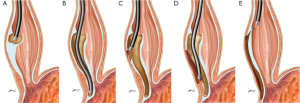
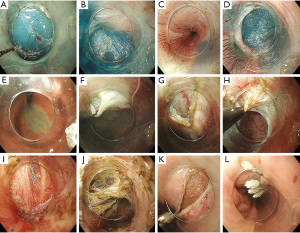
Submucosal tunnel: the tunnel is made downwards by using a technique similar to ESD, passing over the EGJ and enter the proximal stomach about 3 cm. Using TT knife (Figure 3), submucosal tissue is dissected by non-touching technique with spay coagulation 6mode, 50 W, effect 2 on ERBE 300D. Dissecting plane is definitely just beneath muscle layer surface (Figure 3B) (Scheme 1B). Mucosal injury may cause the serious complications because it is an only barrier between esophageal lumen and mediastinum after completion of myotomy. During submucosal dissection, repeated submucosal injection makes submucosal tissue dissection easier. The width of the tunnel is about 1/3 of the circumferential of the tubular esophagus.
Identification of GEJ (Table 1): another interesting issue with the POEM technique concerns identification of the GEJ in submucosal space. As clear markers for identifying the GEJ junction, the following indicators should be checked. The first indicator is insertion depth of the endoscope from the incisors. The position of the GEJ junction in the lumen of the esophagus itself is therefore recorded accurately in advance before we inserted the endoscope into the submucosal tunnel. Insertion depth of the endoscope in the submucosal space is almost the same as the accurate position of the endoscope in the true lumen. The submucosal tunnel created ends at least 3 cm long enough distal to the estimated GEJ. The second indicator is a marked increase of resistance when the endoscope approaches the GEJ, followed by a prompt easing when the endoscope passes through the narrow GEJ and enters gastric submucosal area. The working space in the submucosal tunnel also becomes gradually narrower when the endoscope approaches closely to the LES. At the LES segment, movement of the endoscope is obviously limited with high resistance. The third indicator is identification of palisade vessels in the submucosal layer (Figure 3C). Palisade vessels are located at the distal end of the esophagus. The fourth indicator is a change of vasculature in the submucosal layer. There are plenty of gastric submucosal vessels compared to esophageal submucosal site. Finally, the aberrant innermost longitudinal muscle bundles in front of the circular muscle layer is one of the indicator for esophagogastric junction (10) (Figure 4). Large vessels in the submucosa are coagulated using the hemostatic forceps in soft coagulation mode (80 W, effect 5). Once tip of endoscope is getting into the cardia, submucosal space will be opened widely (Figure 3D). The distal margin of the tunnel can be easily checked by visualized the blue submucosal tattoo (Figure 3E) from retroflex view.
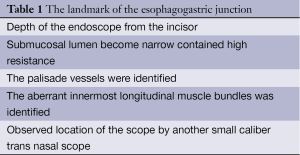
Full table
The recently published paper proposed to use a small caliber trans luminal scope inserted through natural lumen to observed real time dissection. It resulted in precise location but required another endoscopist and special instruments. It was useful in difficult cases (11).
Step 3: endoscopic myotomy
Dissection of the circular muscle bundle was begun at 2 cm distal to the mucosal entry, more than 10 cm above the GEJ (Scheme 1C). The sharp tip of the TT knife was used to first catch a couple of circular muscle bundles and then to lift them up toward the esophageal lumen. The captured circular muscle bundle was cut by spray coagulation current (50 W, effect 2). At the beginning of myotomy transverse muscle bundle should be caught and then gradually cut by electrocautery until longitudinal muscle layer was identified (Figure 3F,G). This inter-muscular space is the correct dissection plane. In any case outer longitudinal muscle layer is thin like a sheet of paper. It is regarded to have less special function of muscle contraction. Operator may reduce risk of surrounding structures injury by keep outer longitudinal layer intact. Division of the sphincter muscle was continued from the proximal side towards the stomach until the endoscope passed through the narrow segment of the LES (Figure 3H). Longitudinal muscle layer should be carefully preserved during the dissection procedure. The injured or torn longitudinal muscle, the mediastinal structures were exposed, does not caused any sequelae or complication if the mucosa was still intact (Figure 3I).
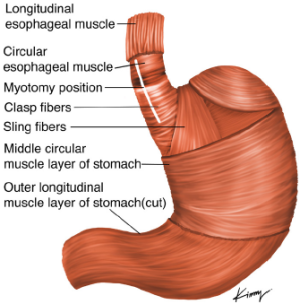
How to avoid symptomatic GERD?
Anterior myotomy in the two o’clock direction in the supine position seems most appropriate, as this leads to lesser curvature of stomach. In contrast, the angle of His is located at in the eight o’clock direction. Anterior myotomy potentially avoids damage to the sling muscle, and especially His angle (Scheme 2). In surgical myotomy an antireflux measure, such as a Dor procedure, is also carried out in order to avoid postoperative GERD, since adjacent structures surrounding the distal esophagus are inevitably dissected which may impair natural antireflux mechanisms. With POEM no antireflux procedure is carried out, since the endoscopist never touches surrounding structures. However, complete myotomy potentially may have a risk for post-therapeutic GERD. When the tip of the endoscope reached the stomach region, the submucosal space suddenly became wider. Thickness of inner circular muscle layer is different in individual cases. Muscle layer cutting was continued for at least 2 cm distal to the EGJ (Figure 3J) (Scheme 1D). Complete division of the circular muscle bundle was confirmed by the endoscopic appearance. Any muscle bundle which runs transversely should not be remained. Complete hemostasis also achieved using coagulating forceps. After completion of the myotomy, smooth passage of an endoscope through the GEJ with minimal resistance was confirmed. The other abnormal esophageal motility patients, presented with odynophagia, need a very long myotomy which surgical myotomy cannot be performed. The myotomy length is approximately 10-15 cm depend on individual cases.
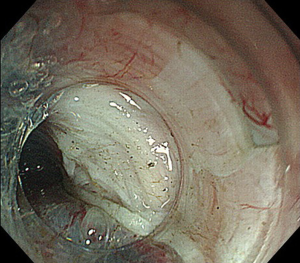
Step 4: closure of mucosal entry
Before closure mucosal entry, 40 mg gentamicin is infused into the submucosal tunnel. The mucosal entry site, usually 2-3 cm long, was closed with about 5-8 hemostatic clips (Figure 3K,L) (Scheme 1E). Whether mucosal entry is elongated over to myotomy site, tight mucosal closure only by clips avoids leakage of esophageal luminal content. Successful closure of the mucosal entry was confirmed by the endoscopic appearance (Figures 1,4). Over the scope clipping device was reported to use as the mucosal closure. Its wide mouth and ability to grasp large amount of tissue acquire secure closure of the mucosa. At the end of the procedure, the smooth passage through the gastrointestinal junction was checked by inserted scope in the natural lumen.
Post-operative care
Immediate post-operative period, Chest X-ray and abdominal plain X-ray was required. It is guarantee for non-clinical pneumomediastinum, pneumothorax nor pneumoperitoneum. Patient was kept fasting, intravenous antibiotic infusion and adequate pain killer.
1st day after POEM
Gastroscopy is needed to confirm the mucosal integrity. If mucosal was tightly closed without mucosal damage, water sipping is allowed. If mucosal defect existed or was questionable, continuing fasting for a few more days and repeated endoscopic examination would be advised. Fortunately, in our series we have no experience of mucosal damage.
TBE is also important to confirm smooth passage of contrast media through EGJ with no leakage and stasis. Mucosal integrity is the premise of diet opening. Begin with drinking liquid on day 1, soft meal can be started on 2nd day post-POEM, and normal diet on 3rd day post-POEM. TBE provided an information for Vaezi score that can predict the prognosis and able to compare with pre-operative stage.
Antibiotics: intravenous infusion of antibiotics was prescribed for three days followed by four days oral antibiotics.
Complications
Pneumoperitoneum
Pneumoperitoneum during the procedure occurred in eight cases, all are treated with abdominal paracentesis to release abdominal pressure. The long 18 gauge needle with stylet is applied through abdominal wall. Carbon dioxide is released under the water.
Pneumomediastinum is managed by inserted small caliber of intercostal drainage (ICD) for couple days.
Mucosal injury
Cardia mucosal perforation is rarely occurred during the procedure. The management guideline is conservative with intravenous antibiotics, apply hemostatic clips and fibrin sealant spray (12). All reports receive successful treatment without any complications. A cover retrievable metallic stent was reported to place to prevent the inevitably stricture following mucosal injury in children (13). The choices of treatment depend on the preference of the endoscopist.
Bleeding
Acute bleeding or intraoperative bleeding manage by pressure the bleeding point with the cap, identified the bleeding point and coagulation with the coaggrasper. The blind coagulation is avoided. In case of bleeding point cannot identified, pressure with the endoscopic tip in submucosal space or natural lumen in correspond level is advised. The postoperative hematoma may occur in this situation. Conservative treatment, keeping fasting with intravenous antibiotic is suggested. The hematoma will gradually resolve within one to two weeks. Diet will be stepping after solved hematoma.
Delay bleeding. A presence of postoperative hematemesis, melena, retrosternal pain, hypotension, and/or tachycardia occurred, the postoperative bleeding should be suspected. CT scan and emergency endoscope are indicated to confirm this condition. Only 0.7% of delayed bleeding was reported (14). Emergency gastroscopy is performed to identify bleeding point in submucosal tunnel. If bleeding point cannot be identified, Sengstaken-Blakemore tube is directly placed into the stomach and lower esophagus to compress the bleeding sites. Bleeding always located at the edge of cut muscle and may related to history of predisposing bleeding factors, e.g., coagulation disorders, and history of antiplatelet/anticoagulant therapy.
Gasatroesophageal reflux (GER)
One of the complications after POEM is GER. The prevalence of mild GER is 46% (15,16) which comparable to 25-40% in laparoscopic heller myotomy (LHM) with Dor fundoplication and 20-30% after Toupet fundolplication (17,18). In our series, Over all post-operative GER was 63% but 80% is mild esophagitis [Los angeles classification (LA) 0, A, B] and symptom free. Only 4.89% (16/327 cases) need acid suppression treatment (LA C, D or symptomatic GER). However, risk factors for GER are still not identified yet. Fortunately, all patients’ symptoms are well controlled by proton pump inhibitor (PPI). One of the hypotheses is the natural antireflux mechanism of the stomach (Angle of His). The fully mobilisation of the stomach during LHM disturb this mechanism while it is not involved by POEM. Thus, it is not necessary to add antireflux procedure.
POEM in children
In our institute, we experienced nine cases of children who diagnosed achalasia. The M:F ratio is 1:2. The major chief complaints are dysphagia. The onset varied from five months to eleven years and duration of disease between 31 months (5-72 months). All of them are type I or II. Only one case is sigmoid achalasia. After treatment, the Eckardt score was significantly reduced from 6.0 to 0.8. The procedure is conducted as same as regular. The obstacles during treatment are the obscure diagnosis, unsatisfied weight and small esophagus.
POEM after endoscopic intervention
Pneumatic dilatation (PD) or Botox injection is acceptable treatment for achalasia patient even though the recurrent rate is still high. However, some patients wish to choose these options as a definite treatment in order to avoid surgery. The long term success of Botox injection and PD are 50% (19) in 1 yr and 40% in 5 yrs (20), respectively. Even the satisfactory result, there are some groups of patient need re-intervention or other treatments. It is generally accepted that the predictors of risk factors for relapse after PD include young age (<40-45 years), male sex, single dilation with a 3.0 cm balloon, post-treatment LES pressure >10-15 mmHg, poor esophageal emptying after timed barium swallow, and type I and type III achalasia pattern on HRM (21,22). It has been shown that POEM can be as safe and effective as first-or second-line treatment, even after the failure of Botox injection or PD. Regards to the technique, there are some difficulty due to existing adhesions from previous intervention. The delicate dissection with repeated normal saline injection leads us to the desirable plane. Coagulation forceps were applied to control unexpected bleeding from prior inflammatory induced vessels. The landmarks of the EGJ needs to clearly identified for adequate dissection plane. All of these techniques make POEM as a safety procedure. Besides of these, POEM also takes a role in esophageal motility disorder treatment. On the other hand, PD plays a good role for temporary treatment in dysphagic patients. It may improve nutritional status, reduced local esophagitis and prevented reflux complication during they are waiting for POEM.
POEM after laparoscopic heller myotomy (LHM)
LHM is expected as a treatment of choice for achalasia. The comparative study showed POEM has equivalent outcome to LHM regards to peri operative and short term outcomes (23,24). The failure of LHM need another intervention or surgery (redo myotomy or esophagectomy). Due to the difficulty to resect adhesions in redo surgery and high morbidity of esophagectomy, POEM is a better choice for treatment recurrence achalasia. The recently report demonstrated ten cases recurrence dysphagia was successfully treatment by POEM (25). The concept of treatment is to make another myotomy in different location from the prior surgery. Even though it showed only short term result, further study is required to define the long-term clinical outcomes.
Training in POEM
Performing POEM procedure requires two professional skills. Basic anatomy beyond the esophageal mucosa and good manipulation of endoluminal procedures are needed. Both gastroenterologist as well as surgeon shared their experiences in this procedure. However, its complications risk serious adverse event including mediastinitis and sepsis. Thus, delicate skills are also needed. The porcine model, explant and living model, was proposed as a standard for POEM training (26). The porcine model has advantage as its similarity to the human anatomy, cheap and reproducible. In contrast, myotomy is limited due to the attenuated circular muscle. The cadaveric model has strong advantage as a real human anatomy but difficulty in mucosotomy and submucosal tunneling dissection due to tissue pliability and poor tissue distention (27). Till now, there is no standard training guideline for training. The training system is divided to two different systems. First is preclinical training which trainee has to practice in the animal or cadaveric model about 46 (range 12-154) hours. On the other hand, some center use clinical proctor system which done initial in human. The median number of proctored cases was 2 cases (1-7 cases) (28). However, the learning curve of POEM procedure was 20 cases in experienced hand (29).
Acknowledgements
Human and animal rights and informed consent: this article does not contain any studies with animal subjects performed by any of the authors. With regard to the authors’ research cited in this paper, all procedures were followed in accordance with the ethical standards of the responsible committee on human experimentation and with the Helsinki Declaration of 1975, as revised in 2000 and 2008.
Disclosure: The authors declare no conflict of interest.
References
- Inoue H, Minami H, Kobayashi Y, et al. Peroral endoscopic myotomy (POEM) for esophageal achalasia. Endoscopy 2010;42:265-71. [PubMed]
- Sadowski DC, Ackah F, Jiang B, et al. Achalasia: incidence, prevalence and survival. A population-based study. Neurogastroenterol Motil 2010;22:e256-61. [PubMed]
- Bretthauer M, Thiis-Evensen E, Huppertz-Hauss G, et al. NORCCAP (Norwegian colorectal cancer prevention): a randomised trial to assess the safety and efficacy of carbon dioxide versus air insufflation in colonoscopy. Gut 2002;50:604-7. [PubMed]
- Brandt LJ, Boley SJ, Sammartano R. Carbon dioxide and room air insufflation of the colon. Effects on colonic blood flow and intraluminal pressure in the dog. Gastrointest Endosc 1986;32:324-9. [PubMed]
- Yasumasa K, Nakajima K, Endo S, et al. Carbon dioxide insufflation attenuates parietal blood flow obstruction in distended colon: potential advantages of carbon dioxide insufflated colonoscopy. Surg Endosc 2006;20:587-94. [PubMed]
- Pandolfino JE, Kwiatek MA, Nealis T, et al. Achalasia: a new clinically relevant classification by high-resolution manometry. Gastroenterology 2008;135:1526-33. [PubMed]
- Bredenoord AJ, Fox M, Kahrilas PJ, et al. Chicago classification criteria of esophageal motility disorders defined in high resolution esophageal pressure topography. Neurogastroenterol Motil 2012;24:57-65. [PubMed]
- Eckardt VF. Clinical presentations and complications of achalasia. Gastrointest Endosc Clin N Am 2001;11:281-92. [PubMed]
- Vaezi MF, Baker ME, Achkar E, et al. Timed barium oesophagram: better predictor of long term success after pneumatic dilation in achalasia than symptom assessment. Gut 2002;50:765-70. [PubMed]
- Eleftheriadis N, Inoue H, Ikeda H, et al. In vivo observation of aberrant innermost longitudinal muscle bundles in front of the circular muscle layer at the level of the esophagogastric junction during peroral endoscopic myotomy. Gastrointest Endosc 2013;78:676. [PubMed]
- Baldaque-Silva F, Marques M, Vilas-Boas F, et al. New transillumination auxiliary technique for peroral endoscopic myotomy. Gastrointest Endosc 2014;79:544-5. [PubMed]
- Li H, Linghu E, Wang X. Fibrin sealant for closure of mucosal penetration at the cardia during peroral endoscopic myotomy (POEM). Endoscopy 2012;44 Suppl 2 UCTN:E215-6.
- Ling T, Pei Q, Pan J, et al. Successful use of a covered, retrievable stent to seal a ruptured mucosal flap safety valve during peroral endoscopic myotomy in a child with achalasia. Endoscopy 2013;45 Suppl 2 UCTN:E63-4.
- Li QL, Zhou PH, Yao LQ, et al. Early diagnosis and management of delayed bleeding in the submucosal tunnel after peroral endoscopic myotomy for achalasia (with video). Gastrointest Endosc 2013;78:370-4. [PubMed]
- Swanstrom LL, Kurian A, Dunst CM, et al. Long-term outcomes of an endoscopic myotomy for achalasia: the POEM procedure. Ann Surg 2012;256:659-67. [PubMed]
- Simić AP, Radovanović NS, Skrobić OM, et al. Significance of limited hiatal dissection in surgery for achalasia. J Gastrointest Surg 2010;14:587-93. [PubMed]
- Khajanchee YS, Kanneganti S, Leatherwood AE, et al. Laparoscopic Heller myotomy with Toupet fundoplication: outcomes predictors in 121 consecutive patients. Arch Surg 2005;140:827-33. [PubMed]
- Rawlings A, Soper NJ, Oelschlager B, et al. Laparoscopic Dor versus Toupet fundoplication following Heller myotomy for achalasia: results of a multicenter, prospective, randomized- controlled trial. Surg Endosc 2012;26:18-26. [PubMed]
- Pasricha PJ, Ravich WJ, Hendrix TR, et al. Intrasphincteric botulinum toxin for the treatment of achalasia. N Engl J Med 1995;332:774-8. [PubMed]
- Eckardt VF, Gockel I, Bernhard G. Pneumatic dilation for achalasia: late results of a prospective follow up investigation. Gut 2004;53:629-33. [PubMed]
- Ghoshal UC, Rangan M. A review of factors predicting outcome of pneumatic dilation in patients with achalasia cardia. J Neurogastroenterol Motil 2011;17:9-13. [PubMed]
- Richter JE. Achalasia - an update. J Neurogastroenterol Motil 2010;16:232-42. [PubMed]
- Hungness ES, Teitelbaum EN, Santos BF, et al. Comparison of perioperative outcomes between peroral esophageal myotomy (POEM) and laparoscopic heller myotomy. J Gastrointest Surg 2013;17:228-35. [PubMed]
- Teitelbaum EN, Rajeswaran S, Zhang R, et al. Peroral esophageal myotomy (POEM) and laparoscopic Heller myotomy produce a similar short-term anatomic and functional effect. Surgery 2013;154:885-91. [PubMed]
- Onimaru M, Inoue H, Ikeda H, et al. Peroral endoscopic myotomy is a viable option for failed surgical esophagocardiomyotomy instead of redo surgical heller myotomy: a single center prospective study. J Am Coll Surg 2013;217:598-605. [PubMed]
- Eleftheriadis N, Inoue H, Ikeda H, et al. Training in peroral endoscopic myotomy (POEM) for esophageal achalasia. Ther Clin Risk Manag 2012;8:329-42. [PubMed]
- Talem D, Mileres OR, Gee DW, et al. Training in per-oral endoscopic myotomy (POEM): cadavers or swine? 53rd SSAT Annual Meeting. San Diago, California, 2012.
- Stavropoulos SN, Modayil RJ, Friedel D, et al. The International. Per Oral Endoscopic Myotomy Survey (IPOEMS): a snapshot of the global POEM experience. Surg Endosc 2013;27:3322-38. [PubMed]
- Kurian AA, Dunst CM, Sharata A, et al. Peroral endoscopic esophageal myotomy: defining the learning curve. Gastrointest Endosc 2013;77:719-25. [PubMed]