
Localized bullous pemphigoid: a case report
Introduction
Bullous pemphigoid (BP) is a rare autoimmune skin disease with the predilection on the elderly. Localized BP is one of the clinical variants of pemphigoid, which comprises three basic entities based on the affected site and disease consequence: mucous membrane pemphigoid, Brunsting-Perry pemphigoid, and localized non-scarring pemphigoid (1). The occurrence of localized BP is unusual and caused attention from 1965 (2), since when few cases have been reported, mainly at the location of the extremities (3-7). The present case describes a patient with localized non-scarring pemphigoid on the breast. The distribution of skin lesions is so rare in BP that misdiagnosis for other dermatological diseases had been diagnosed.
Case presentation
We present the following case in accordance with the CARE guideline.
Patient information
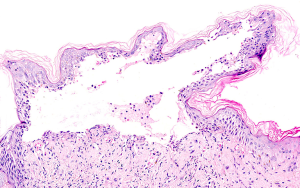
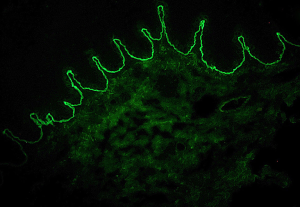
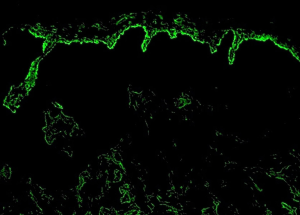
A 30-year-old woman with unremarkable medical history presented with a 4-month history of itchy erythema on her trunk. No one else in the family is known to be affected. Physical examination revealed well-demarcated erythema and maculopapules in bra’s shape (Figure 1). Routine laboratory tests were within the normal ranges. Contact dermatitis was initially diagnosed but lesions were not improved by avoiding wearing bras and treatment with antihistamines. Histopathological examination revealed a subepidermal blister with infiltration of eosinophils and neutrophils (Figure 2). Direct immunofluorescence (DIF) for IgGs or complements (C3) was negative. Indirect immunofluorescence (IIF, Figure 3) revealed linear deposition of serum IgG1. Linear deposition of IgG located at the epidermal side of the dermoepidermal junction, as shown by salt-split IIF (Figure 4). ELISA tests demonstrated positive serum autoantibodies against BP180 with an antibody titer of 21 U/mL. These findings were consistent with BP and a diagnosis of localized BP was made. Our patient had a BP disease area index (BPDAI) score of 18, supporting a mild BP disease. Treatment of mild BP aims to control skin eruption and itch while minimizing side effects of the treatment (8). Treatment of the patient with minocycline 200 mg and nicotinamide 1,500 mg per day resulted in complete remission of the skin lesions within 1 month. No relapse was noticed at the follow-up of 12 months and serum anti-BP180 antibody titer was controlled in normal range.
Patient prospective
“After taking those drugs, I felt relieved from pruritus and gradually the lesions disappeared. After 3 months, I can wear bra with no lesions. I am still under following-up and no relapse occurred.”
Discussion
BP is a chronic, recurrent autoimmune disease characterized by subepidermal blister formation with eosinophilic infiltration and linear deposition of IgGs typically against anti-BP180/230 in the lamina lucida of the basement membrane zone. The generalized BP is more frequently diagnosed in the elderly population. Herein we report a young female patient with localized non-scarring pemphigoid that primarily involved her breasts. The itchy skin lesions are relatively well-defined and symmetrically distributed in a “bra pattern”, which mimic contact dermatitis. Previous reports have shown diagnosis of localized BP tended to be delayed (3), most likely due to initial misdiagnosis as acute allergic contact dermatitis, stasis dermatitis and eczematous dermatitis (3-5). In our case, contact dermatitis was initially diagnosed and later excluded given that DIF, IIF or BP180/230 ELISA for serum autoantibodies are negative in contact dermatitis.
Although the exact mechanism of limited disease remains unclear, localized BP appears to preferentially occur at the sites of frequent mechanical shear stress or trauma, such as the pretibial area (5). This disease has been rarely reported to affect the breast (3). The localized nature is likely derived from multiple triggering factors such as trauma, burns, radiation, hydrostatic forces, and topical medicines that have been previously described to initiate localized BP in case reports (3-7,9). Our patient presented as persistently localized erythema and papules distributed in a bra pattern, suggesting that the local mechanical pressure/friction or an allergic reaction due to the bra could be an incentive factor of blister formation. If the skin disease has predilection to the body sites of trauma, it is also important to differentiate it from epidermolysis bullosa acquisita (EBA) due to the similarities in clinical, pathological, and immunological features to localized BP. In BP, autoantibodies could be detected at the epidermal side using salt-split IIF and confirmed by positive BP180/230 ELISA results. By contrast, EBA is characterized by circulating autoantibodies binding to the dermal side by salt-split IIF and specific antibodies against type VII collagen as measured by ELISA.
With the presence of circulating BP180 autoantibodies, localized BP can progress to a generalized form of BP. Approximately up to 36.8% (7/19) of the localized BP cases ultimately developed generalized BP 1 month to 3 years after diagnosis of localized BP (6,9,10). A plausible hypothesis is that the susceptible yet symptom-free individuals might have prior subclinical BP with BP180 autoantibodies. An additional local insult such as UV radiation, trauma, topical chemicals or mechanical shear stress is necessary to trigger the prodrome such as the eczema- or dermatitis-appearing skin lesions. Consequently, a surge of antibody quantity and antibody affinity by chronic antigen stimulation may give rise to generalized eruption of BP.
In general, localized BP has a more benign disease course compared to the generalized counterpart. However, it should be emphasized that a long-term follow-up of patients with localized BP may be important for management of the chronic disease, given a relatively high risk of developing generalized BP. While topical corticosteroid as first-line therapy failed to achieve disease control of our patient, administration of antibiotics in combination with nicotinamide led to a complete remission of skin lesions within a month. Our case reports a new location of localized BP that is supposed to be triggered by pressure, while the mechanism behind pressure and localized BP remains to be further discovered.
Acknowledgments
Funding: This work was supported by the Milstein Medical Asian American Partnership Foundation, Education Reform Projects of Peking Union Medical College (No. 2016zlgc0106), and the National Natural Science Foundation of China (81972945).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. Ethical approval was obtained from the Ethics Committee of Peking Union Medical College Hospital, Peking Union Medical College and Chinese Academy of Medical Sciences. Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Kaplan RP. Cutaneous involvement in localized forms of bullous pemphigoid. Clin Dermatol 1987;5:43-51. [Crossref] [PubMed]
- Lever WF. Pemphigus and Pemphigoid. Springfield: Charles C Thomas Publishers; 1965.
- Tran JT, Mutasim DF. Localized bullous pemphigoid: a commonly delayed diagnosis. Int J Dermatol 2005;44:942-5. [Crossref] [PubMed]
- Salomon RJ, Briggaman RA, Wernikoff SY, et al. Localized bullous pemphigoid. A mimic of acute contact dermatitis. Arch Dermatol 1987;123:389-92. [Crossref] [PubMed]
- Borradori L, Prost C, Wolkenstein P, et al. Localized pretibial pemphigoid and pemphigoid nodularis. J Am Acad Dermatol 1992;27:863-7. [Crossref] [PubMed]
- Dahl MG, Cook LJ. Lesions induced by trauma in pemphigoid. Br J Dermatol 1979;101:469-73. [Crossref] [PubMed]
- Bart BJ, Bean SF. Bullous pemphigoid following the topical use of fluorouracil. Arch Dermatol 1970;102:457-60. [Crossref] [PubMed]
- Feliciani C, Joly P, Jonkman MF, et al. Management of bullous pemphigoid: the European Dermatology Forum consensus in collaboration with the European Academy of Dermatology and Venereology. Br J Dermatol 2015;172:867-77. [Crossref] [PubMed]
- Prakken JR, Woerdeman MJ. "Pemphigoid" (para-pemphigus): its relationship to other bullous dermatoses. Br J Dermatol 1955;67:92-7. [Crossref] [PubMed]
- Sanders SL, Nelson CT. Pemphigus and pemphigoid. Med Clin North Am 1965;49:681-94. [Crossref] [PubMed]



