
Comparison of albumin-bilirubin grade versus Child-Pugh score in predicting the outcome of transarterial chemoembolization for hepatocellular carcinoma using time-dependent ROC
Introduction
Liver cancer is one of the three leading causes of cancer-related deaths worldwide, and in terms of malignant tumors, it is the seventh most common type (1). Hepatocellular carcinoma (HCC) accounts for about 90% of liver cancer cases (2). The treatment options for HCC include liver transplantation, hepatectomy, local ablative therapy, transarterial chemoembolization (TACE), systemic therapies, and basic supportive care (3). However, on account of the highly aggressive and insidious nature of HCC, a large proportion of patients are classified as being at the intermediate to advanced stage by the time of diagnosis and, as such, beyond the indications for curative interventions such as liver transplantation, hepatectomy, and ablation therapy (4).
For patients with preserved liver function who are not eligible for curative treatments, TACE is the most commonly used nonsurgical treatment modality and, in several randomized controlled trials and meta-analyses, has been reported to prolong survival (5,6). Particularly for patients with intermediate-stage HCC according to Barcelona clinic liver cancer (BCLC) staging system, TACE is the standard treatment modality (7). A growing body of evidence supports the use of TACE for patients with early and advanced HCC (8-10).
Due to a combination of factors, the prognosis assessment of the HCC patients remains complicated and hepatic function, tumor characteristics and performance status must be taken into consideration (11,12). Among them, hepatic function is a vital determinant in the prognosis of HCC. Traditionally, the Child-Pugh score has been used extensively in liver function evaluation and even plays an important role in most of the prevalent HCC staging systems, which inform treatment decision making (13,14). However, the Child-Pugh scoring system has several limitations (15,16): the assessment of ascites and encephalopathy is subjective; all five parameters are given the same weight; moreover, ascites and albumin are interrelated.
Recently, a novel model based on serum albumin and bilirubin has been put forward to assist with liver function evaluation and has shown powerful discriminating ability over Child-Pugh classification in predicting overall survival for patients with HCC (17). However, until now, a consensus on whether the performance of albumin-bilirubin (ALBI) score can accurately reflect the liver function of HCC patients undergoing TACE therapy has not been reached. Besides, it is worth mentioning that the ALBI score appeared capable of classifying patients with Child-Pugh A who underwent liver resection, stereotactic body radiation and sorafenib treatment into two distinct prognostic cohorts (18-20).
This present study aimed to assess and compare the performance of ALBI grade and Child-Pugh score in predicting overall survival outcomes in HCC patients who underwent TACE.
Methods
Study population
In this retrospective study, a total of 221 consecutive HCC patients who underwent TACE therapy from January 2010 to December 2017 were enrolled at the Tangdu Hospital. Baseline parameters were retrieved from the hospital medical database. HCC was diagnosed based on the findings of abdominal ultrasonography. Dynamic computed tomography and magnetic resonance imaging, or a combination of both, were also used, in accordance with the guidelines of the American Association for the Study of the Liver Disease and the European Association for the Study of Liver disease (AASLD/EASL) (13,14).
The inclusion criteria were as follows: liver function of Child-Pugh-A; patients with only one malignant tumor; no HCC-specific-treatment before TACE therapy; and no insufficient heart, lung, kidney, or brain function before TACE therapy.
The exclusion criteria were as follows: curative treatments for HCC prior to TACE therapy; concurrent malignancies; and renal, cerebral or cardiopulmonary dysfunction. Written informed consent was obtained from all patients before the administration of TACE. This investigation was approved by the Clinical Research Ethics Committee of the Tangdu Hospital.
Treatment and follow-up
Prior to TACE, abdominal ultrasound and contrast-enhanced CT or MRI were used to assess tumor status and resectability. The Seldinger technique was used and a 4.1-French RC1 catheter was introduced into the tumor feeding artery. Following this, the number, location, size and branches of the feeding vessels of the tumor were carefully identified. A mixture of 10–20 mL iodized oil, gelfoam particles with 30–50 mg doxorubicin and 50−100 mg cisplatinum was injected into the arterial branches. The number of TACE sessions ranged from 1 to 6, with the procedure scheduled at 1-month intervals and performed depending on the patients’ physical condition.
All patients were followed up at 1 month after TACE therapy and then at 3-month intervals in the first year and every 3–6 months thereafter, as appropriate. Routine examinations were conducted at each follow-up. These included physical examinations, blood tests (serum AFP level, serum biochemistry, liver biochemistry) and imaging examinations (chest X-ray, abdominal ultrasonography, abdominal CT or MRI). The start of the follow-up was defined as the date when TACE therapy began. The end of follow-up was defined as the date of the final visit or death.
Child-Pugh score and ALBI score calculation
Child-Pugh score was calculated using total bilirubin, albumin, prothrombin time, and the clinical findings of encephalopathy and ascites. It was graded as: 5–6 points for Child-Pugh-A; 7–9 points for Child-Pugh-B; and 10–15 points for Child-Pugh-C (15). The ALBI score was calculated by log10Bilirubin (µmol/L) × 0.66 + albumin (g/L) × −0.085. ALBI score ≤−2.60 was defined as grade 1, >−2.60 but ≤−1.39 as grade 2, and >−1.39 as grade 3 (16). The parameters of the Child-Pugh and ALBI scores were obtained within the 1 week preceding TACE therapy to ensure that the patients did not receive albumin supplements, platelet infusion or other treatments beforehand.
Statistical analysis
Categorical variables are expressed as frequencies and percentages; continuous variables are expressed as means (interquartile range). Survival analyses were performed using the Kaplan-Meier method, and the log-rank test was used to examine the statistical differences between the ALBI grade and Child-Pugh score. The Cox proportional hazards model was used for univariate and multivariate analyses of prognostic factors of OS. Three multivariate models with stepwise methods were separately employed to select the independent prognostic factors: model 1 including the baseline characteristics; model 2 including the baseline characteristics and Child-Pugh score but excluding albumin and bilirubin; model 3 including the baseline characteristics and ALBI score but also excluding albumin and bilirubin. Model validation of different staging systems was compared using the C-index as a measure of discrimination. P values <0.05 for all analyses were identified at statistically significant. Statistical analyses were conducted using IBM SPSS software version 23.0 (SPSS Inc., Chicago, IL, USA), and R software version 3.6.1 (R Foundation for Statistical Computing, Vienna, Austria).
Results
Baseline characteristics
According to the protocol, 221 patients were finally included, of whom 194 (87.8%) were male (with a mean age of 56.1 years) and 27 (22.2%) were female (with a mean age of 56.7 years). According to the ALBI grade, there were 106 (48.0%) and 115 (52.0%) patients belonging to the ALBI-1 group and ALBI-2 group, respectively. According to the Child-Pugh system for the evaluation of liver function, there were 160 (72.4%) patients of Child-Pugh-5, and 61 (27.6%) of Child-Pugh-6. In the ALBI-1 group, there were 105 patients of Child-Pugh-A5 and only 1 patient of Child-Pugh-A6. In the ALBI-2 group, there were 55 patients of Child-Pugh-A5 and 60 patients of Child-Pugh-A6. All patients enrolled in the study had unifocal tumors, with a mean tumor size (maximum diameter of the largest tumor) of 8.20 cm. Demographic and clinical features of the patients are summarized in Table 1. Correspondences between ALBI grades and Child-Pugh scores are listed in Table 2.
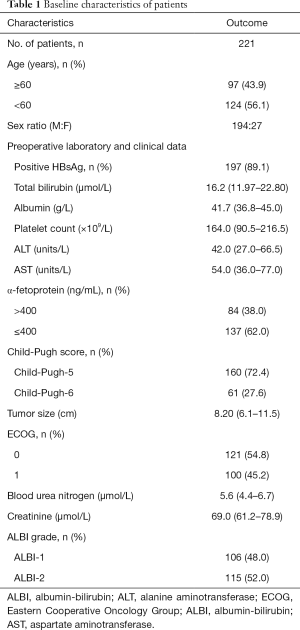
Full table
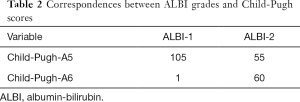
Full table
Survival analyses according to Child-Pugh score and ALBI grade
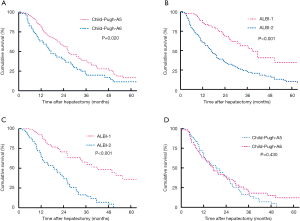
During a median follow-up time of 34.2 months, 121 patients had died and the median OS reached 25.8 months. Based on the Kaplan-Meier curves, both ALBI grade and Child-Pugh score were significantly associated with OS. In addition, patients with Child-Pugh-A5 showed better overall survival than those with Child-Pugh-A6 (OS at 1, 3 and 5 years was 81%, 37%, 13.3% vs. 63.4%, 19.9%, 7.4%, respectively; Log-rank P=0.020; Figure 1A). There was a significant difference in OS between patients with ALBI-1 and ALBI-2 grade. OS at 1,3 and 5 years was higher in patients with ALBI-1 (92.4%, 55.7%, and 27.5%, respectively) than those with ALBI-2 (63.3%, 17.3%, and 5.5%, respectively; Log-rank P<0.001; Figure 1B). Among patients with Child-Pugh-A5, the patients with ALBI-1 had a higher OS at 1,3 and 5 years than those with ALBI-2 (90.9%, 54.8%, 28.8% vs. 63.7%, 37.2%, 0%, respectively; Log-rank P<0.001; Figure 1C). Among patients with ALBI-2, there was no significant difference in OS at 1,3 and 5 years between the patients with Child-Pugh-A5 and Child-Pugh-A6 (63.7%, 34.9%, 0% vs. 62.7%, 18.1%, 12.0% months, respectively; Log-rank P=0.430; Figure 1D).
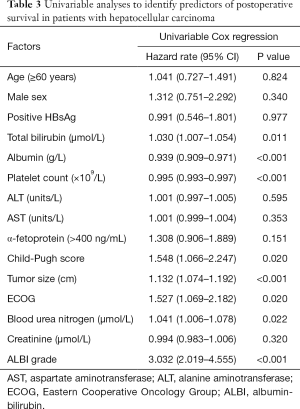
Univariate and multivariate analyses
According to the univariate analysis for OS, the ECOG performance status, tumor size, PLT, BUN, albumin and total bilirubin, as well as Child-Pugh score and ALBI grade were entered into multivariate analyses (Table 3). In multivariate model 1, BUN (HR 1.027, 95% CI: 1.012–1.042, P=0.020), PLT (HR 0.995, 95% CI: 0.993–0.997, P<0.001), total bilirubin (HR 1.029, 95% CI: 1.006–1.053, P=0.015), albumin (HR 0.944, 95% CI: 0.914–0.975, P<0.001) and tumor size (HR 1.144, 95% CI: 1.083–1.207, P<0.001) were identified as independent predictors of OS. According to multivariate model 2, the independent prognostic factors included tumor size (HR 1.121, 95% CI: 1.061–1.185, P<0.001), PLT (HR 0.995, 95% CI: 0.993–0.998, P<0.001), Child-Pugh score (HR 1.545, 95% CI: 1.053–2.267, P=0.026) and BUN (HR 1.028, 95% CI: 1.012–1.043, P<0.001). For multivariate model 3, the independent predictors of OS were tumor size (HR 1.148, 95% CI: 1.087–1.212, P<0.001), PLT (HR 0.996, 95% CI: 0.993–0.998, P<0.001), ALBI grade (HR 2.994, 95% CI: 1.968–4.556, P<0.001) and BUN (HR 1.030, 95% CI: 1.015–1.046, P<0.001) (Table 4). Therefore, according to the multivariate analyses, Child-Pugh score and the ALBI grade could independently predict OS in patients who underwent TACE therapy.
Full table
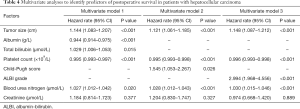
Full table
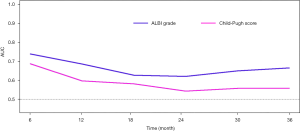
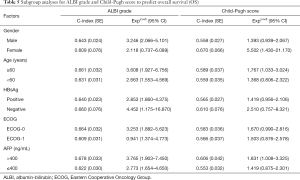
Comparison of the discriminatory abilities for Child-Pugh score and ALBI grade in predicting survival
Figure 2 shows AUCs for Child-Pugh score and ALBI grade and overall survival from 6 to 36 months after the start of follow-up using time-dependent receiver operating curve (ROC) analysis. The ALBI grade had higher predictive power than Child-Pugh score for overall survival based on time-dependent AUCs (Table 4). In addition, their predictive abilities for subsets of patients with different baseline characteristics were investigated. ALBI grade showed better prognostic performance than Child-Pugh score in the all of the subsets apart from the female subgroup (Table 5).
Full table
Discussion
In the present study on HCC patients with Child-Pugh A who received TACE therapy, we demonstrated that ALBI grade had greater discriminatory power than Child-Pugh score in predicting OS. Importantly, the ALBI grade could classify the patients into two distinct prognostic cohorts.
In predicting the outcomes of HCC patients, assessing liver function reserve in order to select appropriate candidates for various kinds of treatments is the key issue. For many years, the traditional Child-Pugh rating system has been the most widely used method for assessing liver function and predicting therapeutic efficacy. Recently, however, due to its limitations, the accuracy of Child-Pugh score has been questioned. Previous studies tried to assess the ALBI grade for patients treated with TACE, but lacked patients with ALBI-2 grade as well as results for long-term outcomes (21).
In this study, we demonstrated that ALBI grade and Child-Pugh score could separately predict the overall survival of HCC patients with Child-Pugh A who underwent TACE therapy. Almost all of the patients included in our research who had a Child-Pugh score of 5 were graded as ALBI-1. However, patients with ALBI-2 had a different Child-Pugh score. In the entire cohort, there was a significant difference in OS between ALBI-1 grade and ALBI-2 grade. Moreover, in patients with Child-Pugh A, the patients with Child-Pugh-6 had a worse prognosis than patients with Child-Pugh-5. It was noteworthy that even in the cohort of patients with Child-Pugh-5—which indicated the best level of liver function—the prognosis could be further divided into two groups by the ALBI grade according to the log-rank test, which illustrated that patients in the same stratum identified by Child-Pugh scoring system had different liver function reserve. Thus, ALBI grade might be a more reasonable and accurate evaluation tool of liver function.
Univariable and multivariable analyses were conducted to identify contributing factors to OS. For multivariable analysis, the albumin and total bilirubin, the Child-Pugh score and the ALBI grade were entered into three different Cox proportional hazards regression models in order to avoid collinearity. Poorer prognosis for patients corresponded with higher Child-Pugh score and ALBI grade. Other than Child-Pugh score and ALBI grade, tumor size, BUN and PLT were also independent predictors of overall survival. Nevertheless, the ECOG score and prothrombin time were not regarded as being statistically significant, although this is a finding to which the small sample size may have contributed.
Time-dependent ROC curves have been introduced to assess the predictive power of diagnostic markers for time-dependent disease outcomes (22). Although both Child-Pugh score and ALBI grade have been confirmed as independent factors associated with OS by means of multivariate analysis, in this study, time-dependent ROC analysis showed that the discriminatory ability of ALBI grade was superior to that of Child-Pugh score for OS of more than 3 years, especially with regard to long-term outcomes. Additionally, subgroup analysis revealed that both ALBI grade and Child-Pugh score were significant predictors of OS in the entire subsets. However, ALBI grade showed better prognostic performance than Child-Pugh score in all subsets apart from the female subgroup.
Although, unlike the Child-Pugh score system, the ALBI grade system excludes subjective factors, its limitations should also be acknowledged. In this system, only two factors (albumin and bilirubin) reflecting liver function are included and considered. However, several factors like positive HBsAg, AST and ALT are excluded. The serum albumin level has a relatively short half-life period and its level is affected by clinical treatment (albumin supplements), as a result, patients with ALBI-1 do not necessarily have good liver function. Furthermore, patients with poor albumin and bilirubin caused by other relevant reasons do not necessarily have severely impaired liver function. As for these above, more accurate models to evaluate liver function are still needed and joint assessment which combines multiple approaches is advisable.
However, this study has several limitations. Firstly, although quality control was ensured because all procedures and administrations were conducted by the same experienced team, the single-centered and retrospective nature of this study may have instilled some bias. Secondly, this study included a relatively small sample size, in which patients with Child-Pugh B and C and ALBI-3 grade were excluded. Whether the results of our study could be applied to the patients with a poorer liver function requires further studies with a larger sample size and effective controls. Finally, most of the study population in our study were Chinese patients with hepatitis B viral infection as the etiology of HCC. This is in contrast to patients in most Western countries, where the etiologies of HCC are mainly hepatitis C virus infection and alcoholic liver disease. Thus, the generalization of our findings should be cautious and future prospective studies are needed.
In summary, for HCC patients with preserved liver function (Child-Pugh A) who are treated with TACE therapy, our study demonstrates that ALBI grade could be used as an alternative assessment of liver function and might be superior to Child-Pugh score in terms of stratifying prognosis. These observations may have major implications for future study design insofar that it is vital to apply this high-quality and evidence-based ALBI grade model to the present HCC staging system to enhance its discriminatory ability.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/atm.2020.02.124). SZ serves as the unpaid editorial board member of Annals of Translational Medicine from Apr 2020 to Mar 2022. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. This investigation was approved by the Clinical Research Ethics Committee of the Tangdu Hospital.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Bray F, Ferlay J, Soerjomataram I, et al. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 2018;68:394-424. [Crossref] [PubMed]
- Llovet JM, Ducreux M, Lencioni R, et al. EASL-EORTC clinical practice guidelines: management of hepatocellular carcinoma. J Hepatol 2012;56:908-43. [Crossref] [PubMed]
- Grandhi MS, Kim AK, Ronnekleiv-Kelly SM, et al. Hepatocellular carcinoma: From diagnosis to treatment. Surg Oncol 2016;25:74-85. [Crossref] [PubMed]
- Choi JW, Kim HC, Lee JH, et al. Transarterial chemoembolization of hepatocellular carcinoma with segmental portal vein tumour thrombus. Eur Radiol 2017;27:1448-58. [Crossref] [PubMed]
- Lo CM, Ngan H, Tso WK, et al. Randomized controlled trial of transarterial lipiodol chemoembolization for unresectable hepatocellular carcinoma. Hepatology 2002;35:1164-71. [Crossref] [PubMed]
- Silva JP, Berger NG, Tsai S, et al. Transarterial chemoembolization in hepatocellular carcinoma with portal vein tumor thrombosis: a systematic review and meta-analysis. HPB (Oxford) 2017;19:659-66. [Crossref] [PubMed]
- Han K, Kim JH. Transarterial chemoembolization in hepatocellular carcinoma treatment: Barcelona clinic liver cancer staging system. World J Gastroenterol 2015;21:10327-35. [Crossref] [PubMed]
- Kim JW, Kim JH, Sung KB, et al. Transarterial chemoembolization vs. radiofrequency ablation for the treatment of single hepatocellular carcinoma 2 cm or smaller. Am J Gastroenterol 2014;109:1234-40. [Crossref] [PubMed]
- Kim JH, Won HJ, Shin YM, et al. Medium-sized (3.1-5.0cm) hepatocellular carcinoma: transarterial chemoembolization plus radiofrequency ablation versus radiofrequency ablation alone. Ann Surg Oncol 2011;18:1624-9. [Crossref] [PubMed]
- Chung GE, Lee JH, Kim HY, et al. Transarterial chemoembolization can be safely performed in patients with hepatocellular carcinoma invading the main portal vein and may improve the overall survival. Radiology 2011;258:627-34. [Crossref] [PubMed]
- Fujiwara N, Friedman SL, Goossens N, et al. Risk factors and prevention of hepatocellular carcinoma in the era of precision medicine. J Hepatol 2018;68:526-49. [Crossref] [PubMed]
- Bruix J, Reig M, Sherman M. Evidence-Based Diagnosis, Staging, and Treatment of Patients With Hepatocellular Carcinoma. Gastroenterology 2016;150:835-53. [Crossref] [PubMed]
- Bruix J, Sherman M. American Association for the Study of Liver Diseases. Management of hepatocellular carcinoma: an update. Hepatology 2011;53:1020-2. [Crossref] [PubMed]
- European Association For The Study Of The Liver and European Organisation For Research And Treatment Of Cancer. EASL-EORTC clinical practice guidelines: management of hepatocellular carcinoma. J Hepatol 2012;56:908-43. [Crossref] [PubMed]
- Wang YY, Zhao XH, Ma L, et al. Comparison of the ability of Child-Pugh score, MELD score, and ICG-R15 to assess preoperative hepatic functional reserve in patients with hepatocellular carcinoma. J Surg Oncol 2018;118:440-5. [PubMed]
- Zheng J, Xing RC, Zheng WH, et al. A comparative study on postoperative mortality prediction of SFLI scoring system and Child-Pugh classification in patients with hepatocellular carcinoma. J BUON 2017;22:709-13. [PubMed]
- Johnson PJ, Berhane S, Kagebayashi C, et al. Assessment of liver function in patients with hepatocellular carcinoma: a new evidence-based approach-the ALBI grade. J Clin Oncol 2015;33:550-8. [Crossref] [PubMed]
- Zhang ZQ, Xiong L, Zhou JJ, et al. Ability of the ALBI grade to predict posthepatectomy liver failure and long-term survival after liver resection for different BCLC stages of HCC. World J Surg Oncol 2018;16:208. [Crossref] [PubMed]
- Su TS, Yang HM, Zhou Y, et al. Albumin - bilirubin (ALBI) versus Child-Turcotte-Pugh (CTP) in prognosis of HCC after stereotactic body radiation therapy. Radiat Oncol 2019;27;14:50.
- Ogasawara S, Chiba T, Ooka Y, et al. Liver function assessment according to the Albumin-Bilirubin (ALBI) grade in sorafenib-treated patients with advanced hepatocellular carcinoma. Invest New Drugs 2015;33:1257-62. [Crossref] [PubMed]
- Hickey R, Mouli S, Kulik L, et al. Independent Analysis of Albumin-Bilirubin Grade in a 765-Patient Cohort Treated with Transarterial Locoregional Therapy for Hepatocellular Carcinoma. J Vasc Interv Radiol 2016;27:795-802. [Crossref] [PubMed]
- Lambert J, Chevret S. Summary measure of discrimination in survival models based on cumulative/dynamic time-dependent ROC curves. Stat Methods Med Res 2016;25:2088-102. [Crossref] [PubMed]


