
Never too old for hip arthroplasty: a 111-year-old woman walks out of hospital—a case report and literature review
Introduction
Although centenarians (people ages ≥100) are still unusual, their population is growing rapidly. According to United Nations estimates (1), there are over half a million centenarians worldwide, which is projected to grow eightfold by 2050. As the number of centenarians is expected to increase considerably in the coming years, the need for joint arthroplasty in this population represents an enormous challenge to patients, surgeons, and anesthesiologists. Currently, hip fractures are responsible for >10% of all hospital admissions for centenarian patients (2). Therefore, thoroughly investigate, review, and summarize the existing literature would contribute to developing a comprehensive knowledge base for future management practices.
Case presentation
A 111-year-old woman was referred to our emergency department with symptoms of right hip pain after a mechanical fall from standing height. Physical examination revealed external rotation and shortening of the right lower extremity. Radiographs confirmed a complete fracture of the femoral neck with partial displacement (Figure 1). She was admitted and scheduled for surgery.

She was 1.57-meter-high, 54 kg, body mass index (BMI) 21.91 kg/m2. Echocardiogram revealed an ejection fraction of 61%, a light mitral and tricuspid insufficiency. Dynamic electrocardiography (DCG) presented atrial flutter with 2–6:1 conduction (heart rate: maximum 160 bpm, average 98 bpm). The numerical rating scale (NRS) for pain was 4 at rest and 6 when active, the Pittsburgh sleep quality index (PSQI) was 15. Preoperative ultrasound screening for the detection of thrombosis came back negative. The main abnormal perioperative laboratory tests are shown in Table 1. Other laboratory results, such as clotting time and liver function, were within the normal range. Arterial blood gas (ABG) analysis (at a continuous oxygen flow 2 L/min): oxygen pressure 131 mmHg, oxygenation index 451 mmHg. Based on these careful preoperative assessments, the enhanced recovery after surgery multidisciplinary team (ERAS-MDT) taken a number of measures to improve the patient's clinical state: (I) selective COX-2 inhibitor was used to relieve pain and control NRS at 1–2 when rest and 3–4 when active; (II) sleep intervention such as desultory conversation with family members during daytime, reducing noise and distraction at night to treat situational insomnia, and the PSQI score was improved to 13; (III) nutritionist prepared small-peptide and whole-protein for oral administration; (IV) continuous low-flow oxygen via nasal cannula to enhance oxygenation, breathing exercises to improve pulmonary function; (V) maintaining fluid balance to prevent heart failure and other heart problems; (VI) perioperative tests for acute phase reactants were obtained to monitor and diagnose of infections.
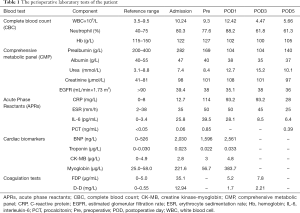
Full table
After a three-day improvement of clinical state, she received a cemented hemiarthroplasty surgery. General anesthesia in combination with a single femoral nerve block was used to tailor to individual patient requirements. The intraoperative fluid administration was restricted to 1,000 mL. The surgery was uneventful and lasted for 35 minutes. Tranexamic acid was injected intra-articular to reduce blood loss. No blood products were required.
Vital signs were monitored closely after surgery. The postoperative target for fluid administration was to keep the daily fluid balance. Patient-controlled analgesia was used for pain relief. Weight-bearing was started about 1.5 hours after surgery when the patient completely recovered from anesthesia in the post-anesthesia care unit, and independent ambulation with a walker was achieved on postoperative day 1. Low-molecular-weight heparin (4,000 IU) was administered subcutaneously 8 hours postoperatively for thromboprophylaxis and once daily until discharge. Oral feeding formula containing small peptides, whole protein, and probiotics was given after surgery (3). Despite the preventable measures taken, delirium occurred the night following the surgery. The motor subtypes of postoperative delirium (POD) were both hyperactive and hypoactive delirium (also called mixed delirium). Olanzapine (5 mg) was added after a psychiatry consultation, other measures including active surveillance, continuous low-flow oxygen, minimizing the complexities of the physical constraints, kept the patient oriented, familiar family members talk about family news to provide mental stimulation throughout the daytime, reducing noise and distraction to ensure the patient obtains maximum uninterrupted sleep at night. The improvement of delirious symptoms was continued until postoperative day 2, and fully recovered from delirium on postoperative day 3. The patient was discarded to a rehabilitation facility on postoperative day 6, aware, oriented, and pain-free. At 7 months of telephone follow-up, the patient was able to walk 50 meters with a metal walker.
Discussion
In this case, we reported a 111-year-old woman who received a cemented hemiarthroplasty to treat a displaced femoral neck fracture. To our best knowledge, this woman should be one of the oldest patients in the world to have had a joint arthroplasty. In order to draw lessons from this case and optimize the perioperative and intraoperative management, we searched PubMed and Embase for case reports of centenarian patients who underwent hip fracture surgery or joint arthroplasty. To ensure literature saturation, a supplementary search was further conducted using Google for news reports. Data such as year, location, gender, age, hospital, surgical indication, types of surgery, types of anesthesia used was retrieved and summarized in Table 2.
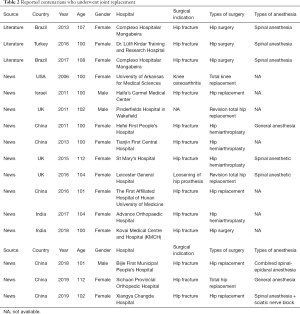
Full table
First, there is little controversy over the necessity of joint arthroplasty among the oldest age group even if short-term postoperative life expectancy estimates (4-7). A widely accepted philosophy is never too old for joint arthroplasty. Several case reports and numerous news have described successful hip hemiarthroplasty, total hip arthroplasty (THA), and revision THA in patients range 100–112 years (8-10) (Table S1). A couple of retrospective studies have found that the short-term outcomes among centenarians were comparable with those younger cohorts with similar fracture patterns (4,5,11), which suggested that hip arthroplasty is worthwhile to maintain quality of life, and should not be refused solely on account of extreme age or the concern of high in-hospital mortality risk.

Full table
Second, the surgical time in patients with hip fracture remains disputed. Although guidelines from both AAOS (12) and NICE (13) guidelines recommend surgery within 48 hours after admission, and a recent study (14) even suggested healthcare institutions and clinicians to reduce time to hip fracture surgery ideally within 24 hours as the standard, the optimal surgical time for the centenarian population was rarely investigated. A retrospective cohort study (11) found that time to surgery does not appear to affect short-term mortality rates of this extremely elderly population, which manifested a potential benefit from preoperative optimization. We should bear in mind that the primary challenge for centenarian candidates is not the surgery itself, but the frail bodies are lack of physiological reserve, they could tolerate operations, but not complications. In this case, a thorough examination was conducted to identify and treat correctable comorbidities immediately so that surgery could be arranged without delay.
Third, the choice of regional or general anesthesia is an age-old debate. More and more evidence suggested that spinal anesthesia should be considered over general anesthesia for hip fracture repair procedures, although the optimal anesthesia modality for the surgical treatment of hip fractures is controversial, and no recent study was able to address or appreciate the clinical differences fully (13,15-17). Compared with general anesthesia, regional anesthesia has been shown to reduce rates of in-hospital mortality, thromboembolism, transfusion, operative time, superficial wound infection, and length of hospitalization (18-20). In particular, for centenarians who suffered from hip fracture, a comprehensive patient-specific preoperative evaluation by the anesthesia team play a crucial role in determining anesthesia type (21). Notably, there was consolidate evidence that supports peripheral nerve blocks in hip fractures, which not only decreases pain on movement but also reduces the risk of pneumonia, decreases time to first mobilization and cost of the analgesic drugs (22).
Fourth, there are few studies focused on treatment patterns of hip fracture in the centenarian population. Manoli et al. reported that approximately 92% were internal fixation for extracapsular hip fractures, and 60% were hemiarthroplasty for intracapsular fractures (11). The management of osteoporosis-related hip fractures in such a population is always challenging because they may never be able to tolerate re-operation. Both short-term and long-term studies have found a higher incidence of re-operation after internal fixation and recommend arthroplasty for lucid elderly patients (23-25). Therefore, arthroplasty may be a better choice for hip fractures. Hemiarthroplasty, which is associated with a lower risk of dislocation, without the requirement of acetabular reaming, and decreased operative time and blood loss, is more suitable for this lower-demand population (26,27). The usage of cemented fixation could decrease the risk of periprosthetic fracture and loosening (28).
Fifth, it is understandable that prolonged operative time would increase the risk of multiple postoperative complications, including anemia requiring transfusion, wound dehiscence, renal insufficiency, and surgical site infection (29,30), and these risks tended to increase with increasing age. Therefore, a number of factors such as accurate preoperative planning, highly experienced surgeon, well-trained surgical assistants, circulating nurses, would shorten the operative time and should be given priority and efforts. More specifically, the minimally invasive anterolateral approach and abbreviated cementing technique also contribute to completing the surgery expeditiously (31-34). Notably, no compromise in surgical technique should be made to obtain a shorter operative time, since cemented hemiarthroplasty consists of many standardized surgical procedures, which would take some time and could not accelerate anymore (29,30).
Next, as the centenarian population continues mounting in the near future, they also represent a significant challenge to perioperative care. Although recent advances in perioperative care, especially the implementation of the ERAS program, have led to a significant decline in complications, centenarians who characterized by multimorbidity demand higher quality of perioperative care. Considering multimorbidity in centenarians is quite common, the integration of a multidisciplinary approach (ERAS-MDT) is of paramount importance in perioperative care, which would be helpful for prevention and management of various complications including delirium, congestive heart failure, malnutrition, renal disease, pain, etc. (35).
In addition, although most of the perioperative complications (e.g., urinary tract infections, pneumonia, and deep venous thrombosis) are manageable, one of the most troublesome complications is POD, which has also occurred in this case. POD is strongly associated with both short-term and long-term adverse consequences in older patients (36,37). However, over the past decades, no new effective treatment options have emerged for POD, and antipsychotics are still the most commonly used medication to treat the symptoms of delirium. There has been a general consensus regarding the role of unmodifiable risk factors (e.g., older age, history of psychiatric illness, higher comorbidity burden), the role of modifiable risk factors (e.g., operation time, electrolyte disorders, hemoglobin, and albumin level), and the role of disputed risk factors (e.g., perioperative medications, type of anesthesia) for POD (38-44). Perioperative improvement of the modifiable medical risk factors may exacerbate or attenuate the risk of POD, and further research is warranted to investigate other risk factors that impact on POD.
Finally, the steady increase of centenarians is undoubtedly a phenomenal achievement of the public healthcare system. Nevertheless, centenarians also pose an unprecedented challenge to the healthcare system in turn. Recent research has shown that the centenarians can exceptionally fit as well as younger counterparts after procedures ranging from laparoscopic cholecystectomy, vascular procedures, aortic valve repair, to spine surgery, primary and even revision joint arthroplasty (8-10,45-48). Therefore, centenarians should not be denied on the basis of chronologic age, and they deserve equal resources as younger people.
In summary, although hip fractures in centenarians pose a challenge, it is never too old for joint arthroplasty. Preoperative assessment, medical optimization, optimal anesthesia management, expeditious surgery, coordinated multidisciplinary approach, and meticulous perioperative care are paramount in treating these patients.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- United Nations. World population prospects: The 2015 revision. Available online: https://www.un.org/en/development/desa/publications/world-population-prospects-2015-revision.html
- Cummings SR, Rubin SM, Black D. The future of hip fractures in the United States. Numbers, costs, and potential effects of postmenopausal estrogen. Clin Orthop Relat Res 1990.163-6. [PubMed]
- Wu XD, Liu MM, Liang X, et al. Effects of perioperative supplementation with pro-/synbiotics on clinical outcomes in surgical patients: A meta-analysis with trial sequential analysis of randomized controlled trials. Clin Nutr 2018;37:505-15. [Crossref] [PubMed]
- Krishnan E, Fries JF, Kwoh CK. Primary knee and hip arthroplasty among nonagenarians and centenarians in the United States. Arthritis Rheum 2007;57:1038-42. [Crossref] [PubMed]
- Ng WX, Kwek EB. Too old for surgery? Outcomes of hip fracture surgery in centenarians. Ann Acad Med Singapore 2017;46:115-7. [PubMed]
- Cheung MY, Ho A, Wong S. Operative outcome of Hong Kong centenarians with hip fracture. Hong Kong Med J 2017;23:63-6. [PubMed]
- Mosfeldt M, Madsen CM, Lauritzen JB, et al. Centenarian hip fracture patients: a nationwide population-based cohort study of 507 patients. Acta Orthop 2019;90:342-7. [Crossref] [PubMed]
- Imbelloni LE, Lima U, Pedrosa FK. Successful anesthesia and hip surgery in a 107-year-old patient. Am J Case Rep 2014;15:308-11. [Crossref] [PubMed]
- Imbelloni L, Galvão A, Santos J, et al. Successful Treatment of a Hip Fracture in a 108 Years Old Patient. A Case Report. J Anesth Crit Care 2017;7:00257.
- Cevik B. Anaesthesia for hip fracture surgery in a 100-year old. Br J Anaesthesia 2016;117. [Crossref]
- Manoli A III, Driesman A, Marwin RA, et al. Short-term outcomes following hip fractures in patients at least 100 years old. J Bone Joint Surg Am 2017;99:e68. [Crossref] [PubMed]
- Roberts KC, Brox WT. AAOS clinical practice guideline: management of hip fractures in the elderly. J Am Acad Orthop Surg 2015;23:138-40. [Crossref] [PubMed]
- The management of hip fracture in adults. London: Royal College of Physicians (UK); 2011. NICE Clinical Guidelines, No. 124.
- Pincus D, Ravi B, Wasserstein D, et al. Association between wait time and 30-day mortality in adults undergoing hip fracture surgery. JAMA 2017;318:1994-2003. [Crossref] [PubMed]
- Rashid RH, Shah AA, Shakoor A, et al. Hip fracture surgery: does type of anesthesia matter? Biomed Res Int 2013;2013:252356. [Crossref] [PubMed]
- Neuman MD, Rosenbaum PR, Ludwig JM, et al. Anesthesia technique, mortality, and length of stay after hip fracture surgery. JAMA 2014;311:2508-17. [Crossref] [PubMed]
- O'Donnell CM, McLoughlin L, Patterson C, et al. Perioperative outcomes in the context of mode of anaesthesia for patients undergoing hip fracture surgery: systematic review and meta-analysis. Br J Anaesth 2018;120:37-50. [Crossref] [PubMed]
- Fields AC, Dieterich JD, Buterbaugh K, et al. Short-term complications in hip fracture surgery using spinal versus general anaesthesia. Injury 2015;46:719-23. [Crossref] [PubMed]
- Van Waesberghe J, Stevanovic A, Rossaint R, et al. General vs. neuraxial anaesthesia in hip fracture patients: a systematic review and meta-analysis. BMC Anesthesiol 2017;17:87. [Crossref] [PubMed]
- Chen DX, Yang L, Ding L, et al. Perioperative outcomes in geriatric patients undergoing hip fracture surgery with different anesthesia techniques: A systematic review and meta-analysis. Medicine (Baltimore) 2019;98:e18220. [Crossref] [PubMed]
- Rozell JC, Hasenauer M, Donegan DJ, et al. Recent advances in the treatment of hip fractures in the elderly. F1000Res 2016;5. [Crossref] [PubMed]
- Guay J, Parker MJ, Griffiths R, et al. Peripheral nerve blocks for hip fractures. Cochrane Database Syst Rev 2017;5:CD001159. [PubMed]
- Gao H, Liu Z, Xing D, et al. Which is the best alternative for displaced femoral neck fractures in the elderly?: A meta-analysis. Clin Orthop Relat Res 2012;470:1782-91. [Crossref] [PubMed]
- Johansson T. Internal fixation compared with total hip replacement for displaced femoral neck fractures: a minimum fifteen-year follow-up study of a previously reported randomized trial. J Bone Joint Surg Am 2014;96:e46. [Crossref] [PubMed]
- Jiang J, Yang CH, Lin Q, et al. Does arthroplasty provide better outcomes than internal fixation at mid-and long-term followup? A meta-analysis. Clin Orthop Relat Res 2015;473:2672-9. [Crossref] [PubMed]
- Moerman S, Mathijssen NM, Tuinebreijer WE, et al. Hemiarthroplasty and total hip arthroplasty in 30,830 patients with hip fractures: data from the Dutch Arthroplasty Register on revision and risk factors for revision. Acta Orthop 2018;89:509-14. [Crossref] [PubMed]
- Wang F, Zhang H, Zhang Z, et al. Comparison of bipolar hemiarthroplasty and total hip arthroplasty for displaced femoral neck fractures in the healthy elderly: a meta-analysis. BMC Musculoskelet Disord 2015;16:229. [Crossref] [PubMed]
- Langslet E, Frihagen F, Opland V, et al. Cemented versus uncemented hemiarthroplasty for displaced femoral neck fractures: 5-year followup of a randomized trial. Clin Orthop Relat Res 2014;472:1291-9. [Crossref] [PubMed]
- Bohl DD, Ondeck NT, Darrith B, et al. Impact of operative time on adverse events following primary total joint arthroplasty. J Arthroplasty 2018;33:2256-62.e4. [Crossref] [PubMed]
- Wu X-D, Hu K-J, Tian M, et al. Letter to the editor on “impact of operative time on adverse events following primary total joint arthroplasty”. J Arthroplasty 2018;33:2701-2. [Crossref] [PubMed]
- de Jong L, Klem TM, Kuijper TM, et al. The minimally invasive anterolateral approach versus the traditional anterolateral approach (Watson-Jones) for hip hemiarthroplasty after a femoral neck fracture: an analysis of clinical outcomes. International orthopaedics 2018;42:1943-8. [Crossref] [PubMed]
- Fullam J, Theodosi PG, Charity J, et al. A scoping review comparing two common surgical approaches to the hip for hemiarthroplasty. BMC Surg 2019;19:32. [Crossref] [PubMed]
- Robertson GA, Wood AM. Hip hemi-arthroplasty for neck of femur fracture: What is the current evidence? World J Orthop 2018;9:235. [Crossref] [PubMed]
- Chandler M, Z, Kowalski R, Watkins N, et al. Cementing techniques in hip resurfacing. Proc Inst Mech Eng H 2006;220:321-31. [Crossref] [PubMed]
- Pioli G, Giusti A, Barone A. Orthogeriatric care for the elderly with hip fractures: where are we? Aging Clin Exp Res 2008;20:113-22. [Crossref] [PubMed]
- Gleason LJ, Schmitt EM, Kosar CM, et al. Effect of delirium and other major complications on outcomes after elective surgery in older adults. JAMA Surg 2015;150:1134-40. [Crossref] [PubMed]
- Bin Abd Razak HR, Yung WY. Postoperative Delirium in Patients Undergoing Total Joint Arthroplasty: A Systematic Review. J Arthroplasty 2015;30:1414-7. [Crossref] [PubMed]
- Weinstein SM, Poultsides L, Baaklini L, et al. Postoperative delirium in total knee and hip arthroplasty patients: a study of perioperative modifiable risk factors. Br J Anaesth 2018;120:999-1008. [Crossref] [PubMed]
- Ravi B, Pincus D, Choi S, et al. Association of Duration of Surgery With Postoperative Delirium Among Patients Receiving Hip Fracture Repair. JAMA Network Open 2019;2:e190111. [Crossref] [PubMed]
- Patel V, Champaneria R, Dretzke J, et al. Effect of regional versus general anaesthesia on postoperative delirium in elderly patients undergoing surgery for hip fracture: a systematic review. BMJ Open 2018;8:e020757. [Crossref] [PubMed]
- Huang J, Razak HRBA, Yeo SJ. Incidence of postoperative delirium in patients undergoing total knee arthroplasty—an Asian perspective. Ann Transl Med 2017;5:321. [Crossref] [PubMed]
- Wang L-H, Xu D-J, Wei X-J, et al. Electrolyte disorders and aging: risk factors for delirium in patients undergoing orthopedic surgeries. BMC Psychiatry 2016;16:418. [Crossref] [PubMed]
- Chung KS, Lee JK, Park JS, et al. Risk factors of delirium in patients undergoing total knee arthroplasty. Arch Gerontol Geriatr 2015;60:443-7. [Crossref] [PubMed]
- Wang L, Seok S, Kim S, et al. The risk factors of postoperative delirium after total knee arthroplasty. J Knee Surg 2017;30:600-5. [Crossref] [PubMed]
- Nagamine Y, Godai K, Oki H, et al. Management of a centenarian who underwent emergency laparoscopic cholecystectomy under general anesthesia with subcostal transversus abdominis plane block. JA Clin Rep 2016;2:24. [Crossref] [PubMed]
- Wheatley BJ, Gorsuch JM, Mansour MA, et al. Vascular procedures in nonagenarians and centenarians are safe. Am J Surg 2011;201:301-4. [Crossref] [PubMed]
- Aslan AN, Ayhan H, Özdemir E, et al. A centenarian transcatheter aortic valve implantation case. J Geriatr Cardiol 2016;13:869. [PubMed]
- Garcia RM, Belding J, Bohlman HH. Lumbar decompression and fusion in a centenarian. Orthopedics 2012;35:e1141-4. [Crossref] [PubMed]


