Paraplegia during coronary artery bypass graft surgery caused by bilateral anterior cerebral artery territory infarction
Introduction
Paraplegia is an unpredictable complication that can occur after repair of coarctation of the aorta, repair of aortic dissection and valvular surgery. Paraplegia after coronary artery bypass graft (CABG) surgery is rare and mostly related to hypoperfusion of the spinal cord arteries (1). We hereby report a case of pure motor paraplegia after CABG, caused by bilateral anterior cerebral artery (ACA) infarcts.
Case report
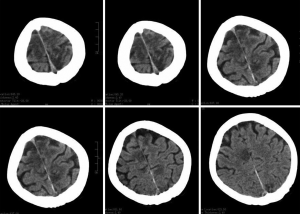
A 54-year-old woman was referred for CABG surgery after she experienced an acute coronary syndrome. Her surgery was done off pump and was uneventful. Postoperative day two, patient remained drowsy, not moving her lower limbs but occasionally moving her both upper limbs spontaneously. On postoperative day three, patient was awake, had pure motor paraplegia (zero power both lower limbs) with all sensations spared, no weakness in upper limbs and normal cranial nerves as well as higher mental functions. She was catheterized and there was no bowel incontinence. A possibility of hypoperfusion leading to spinal cord ischemia was considered. Magnetic resonance imaging (MRI) of spine was ordered but could not be done because of epicardial pacing wires. Computed tomography (CT) of the brain showed bilateral infarction in the ACA territory (Figure 1).
Discussion
Intra-operative embolization remains a major cause of post-CABG stroke (2). Two-third of cardioembolic strokes predominantly affect the occipital lobe and the watershed area between the middle cerebral and posterior cerebral artery territory. In remaining one-third of cases, infarct lesion is single and involves the area supplied by the middle cerebral, vertebral and basilar arteries. Unilateral ACA infarction is responsible for only 0.6% to 3% of all cerebrovascular accidents and usually is result of embolism from the heart or the internal carotid artery (63%) (3). Occlusion of the stem of the ACA proximal to its connection with the anterior communicating artery is usually well tolerated because adequate collateral flow is provided via the anterior communicating artery from the ACA on the opposite side. When the occlusion is localized distal to the anterior communicating artery, neurological symptoms appear.
Bilateral ACA infarction is even rare. Twenty-seven cases of ACA territory infarction were reported among 1,490 cases of cerebral infarction in the Lausanne Stroke Registry; however, there were only two cases of bilateral ACA territory infarction (3). Bilateral infarctions are usually due to spasm that complicates subarachnoid hemorrhage from an aneurysm of the anterior communicating artery. Another cause is thrombosis of the proximal part of one ACA when the contralateral proximal branch is rudimental or absent. In 2004, Yamaguchi et al. reported a similar case with a patient presenting with lower limb weakness and magnetic resonance angiography demonstrating bilateral anaplastic ACAs (4).
Most cerebral infarctions occurring after CABG are usually caused by emboli originating from intra-cardiac chambers. Atrial fibrillation (AF) is the most common complication after cardiac operation. AF significantly increases possibility of cerebral or systemic embolization. There was no history of AF in our patient prior to surgery, no intra cardiac thrombus was found on echocardiography, nor AF was documented during hospitalization. Significant carotid stenosis reduces cerebral blood flow and increases risk of stroke during cardiopulmonary bypass operation. However carotid doppler done prior to surgery was normal in our patient. CT angiography of head and neck vessels, done after this event, was also found to be absolutely normal. Transient hypotension during bypass operations may also decrease brain perfusion and increase neurological deficits. However her perioperative period was reported to be uneventful and no episode of significant hypotension was observed. Another common cause of post-CABG stroke (and another possible source in our patient) is embolization of atherothrombotic plaque from aortic arch. Clamping, releasing and cannulating the diseased aorta potentially dislodge atheromatous plaque and causes ischemic stroke.
Aortic atheroma can be identified by manual palpation or by ultrasound sonogram. Transesophageal echocardiogram has been used to locate aortic calcification and monitor emboli during bypass operation. Currently MRI technique and multi-slice CT scan have been applied to delineate amount and severity of aortic atheroma. However, none of these techniques were used to rule out aortic atheroma in this patient. Current guidelines recommend minimizing aortic manipulation or avoiding touching atheromatous aorta whenever possible (5).
Although paraparesis may initially suggest spinal cord involvement, bilateral frontal pathology should also be considered in differential diagnoses. Infarctions in the ACA territory usually involve the paracentral component of the frontal lobe affecting motor neurons with a somatotopic distribution mostly related to the lower extremities. Motor deficit with a characteristic crural distribution is the most common neurological sign of ACA stroke and was present in 96% of patients in the series of the Lausanne Stroke Registry (3). Bilateral ACA infarctions can result in acute paraparesis or tetraparesis and neuropsychological alterations due to frontal lobe damage.
Our patient presented as pure motor paraplegia without affecting higher mental functions, an unusual presentation which has never been reported. This aetiological aspect is important because a diagnosis of cardioembolism has practical implications in the management of these patients. Paraplegia after cardiac surgery is typically not diagnosed soon after onset because patients have postoperative pain and are given analgesics and sedatives in the immediate post-operative period. Secondly, use of MRI after cardiac surgery is limited because the patients often have epicardial pacemaker wires, permanent pacemakers, and implantable pacer cardioverter defibrillators. Consequently, the paraplegia may go undiagnosed until several days after its occurrence. Providing “sedation holidays” for even the most critically ill patients is imperative, to permit assessment of neurological status and detection of any deviations from the norm. Once recognized, a plan of care can be rapidly implemented to prevent further complications, even if the paraplegia is irreversible.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Scherr K, Urquhart G, Eichorst C, et al. Paraplegia after coronary artery bypass graft surgery: case report of a rare event. Crit Care Nurse 2006;26:34-6, 38-40, 42-5. [PubMed]
- Veerakul G, Veerakul G, Visudharom K. Cerebral complications in conventional coronary bypass graft surgery. Bangkok Med J 2011;2:58-66.
- Bogousslavsky J, Regli F. Anterior cerebral artery territory infarction in the Lausanne Stroke Registry. Clinical and etiologic patterns. Arch Neurol 1990;47:144-50. [PubMed]
- Yamaguchi K, Uchino A, Sawada A, et al. Bilateral anterior cerebral artery territory infarction associated with unilateral hypoplasia of the A1 segment: report of two cases. Radiat Med 2004;22:422-5. [PubMed]
- Task Force on Myocardial Revascularization of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS); European Association for Percutaneous Cardiovascular Interventions (EAPCI), Wijns W, et al. Guidelines on myocardial revascularization. Eur Heart J 2010;31:2501-55. [PubMed]


