
Timing for removing prophylactic drains after liver resection: an evaluation of drain removal on the third and first postoperative days
Introduction
Conventionally, drains are inserted to detect postoperative hemorrhage and/or to drain bile or ascites in patients undergoing a hepatectomy (1). However, several drawbacks of drain placement have been recognized in recent years (2). In the field of several general and visceral surgeries, abdominal drains are not placed as frequently as before (3-5).
In the field of liver surgery, six randomized controlled trials (RCTs) have been conducted to evaluate the need for prophylactic drains since the 1990s (6-11). As five of the six RCTs advocated against prophylactic drain insertion (6,7,9-11), previous meta-analyses concluded that no evidence exists to support routine drain use after uncomplicated liver resections (1,12). However, there are two major problems. First, four of the trials did not contain a calculation of the sample size or defined endpoints (6-8,11). Furthermore, the primary endpoint of the other two trials was the incidence of local wound complications (9,10), most of which are now classified as grade I according to the Clavien-Dindo classification (13). Meanwhile, the incidences of serious complications classified as grade III or higher were not investigated properly. Second, bile leakage was not clearly defined in five of the trials (6,8-11). Despite these trials, prophylactic drains remain in common use in many institutions (14-16).
At our institute, prophylactic drains are used in all patients undergoing liver resection, and usually removed from postoperative day (POD) 7 to 14. With such careful management, we speculate that the operative mortality at our institution became relatively low (0.07%) (17). However, among patients undergoing a hepatectomy between January and December 2010, the incidence of postoperative drain infection and the median duration of the postoperative hospital stay were 12% and 14 days, respectively, which are unsatisfactory. Improving these outcomes while maintaining a high level of safety still seems to be an important issue in liver surgery.
When considering where to begin to solve this problem, careful attention was given to applying the results of previous RCTs, i.e., no drain management, not only because of the methodological problems mentioned above, but also because of the problem of external validity. We recently reported that the incidence of retrograde drain infections increased when drain placement was prolonged for more than 4 PODs in patients with hepatocellular carcinoma (18). After considering these matters, we decided to begin with drain removal during the early postoperative period. Based on recent reports (19,20) and data from our previous cases, we defined three criteria for the early removal of drains. By applying these criteria, we removed the drains on POD 3 between January 2012 and February 2013 and on POD 1 between February and December 2013. In the present study, the outcomes of drain removal on POD 3 and on POD 1 were retrospectively evaluated.
Methods
Patients
Patients who underwent open liver resection at the University of Tokyo Hospital were included. Patients with any of the following were excluded: a need for bilioenteric reconstruction; required resection of another organ (except cholecystectomy); other malignant disease outside the liver; an age of less than 20 years or over 80 years; an indocyanine green retention rate at 15 min ≥20%; and severe co-morbidity. As we had just started laparoscopic liver resection when the present study was conducted, we decided to exclude these patients considering for safety. The current study was approved as project number 11,660 by the Graduate School of Medicine and Faculty of Medicine, the University of Tokyo Research Ethics Committee. The protocol and the data of the study were retrospectively registered at the UMIN Clinical Trial Registry (UMIN000030518).
Surgical technique and intraoperative care
The surgical procedures were selected according to a previously described algorithm (21). Liver transection was performed using the clamp crushing method, while an ultrasonically activated device or a bipolar vessel-sealing device was used according to the surgeons’ preference (22). Pringle’s maneuver (15 min clamping and 5 min release) was applied in all the patients. Fibrin glue (BeriplastR P; CSL Behring, King of Prussia, Pennsylvania, USA) was applied to the raw liver surface after the completion of all the procedures. A silicone rubber closed-suction drain (recommended by the previous reports (23) and the Guidelines for Prevention of Surgical Site Infection (24), issued by the Centers for Disease Control and Prevention) with an inner diameter of 8 mm and with one hole at the tip and two side holes (Phycon drain; Fuji system, Tokyo, Japan) was placed near each transection surface of the liver via the shortest route from the abdominal wall. Penrose drain was not used because it has the potential of retrograde infection and it is difficult to exchange when drainage is necessary for a long period.
Drainage management and postoperative care
Before January 2012, the drains were removed gradually by 2 cm each day beginning on POD 7, with drain removal usually completed within 14 PODs (17). The drained fluid was routinely submitted for laboratory testing (measurements of total bilirubin level and bacteriologic cultures) twice a week including on POD 1 and POD 3. The drains were left in place even after POD 7 if some of the following criteria were not fulfilled: (I) a drain-fluid bilirubin level of below 5 mg/dL on two consecutive tests; (II) a drain discharge volume of less than 500 mL/day; and (III) negative bacteriologic cultures and no macroscopic findings suggesting the presence of bile or infection in the drain discharge (17). The outcomes of patients undergoing a hepatectomy between January and December 2010 were retrospectively investigated as a control group.
We modified our conventional criteria mentioned above and defined three criteria for the early removal of drains based on previous reports (19,20) and data from previous cases. Our early removal criteria were as follows: (I) drain-fluid bilirubin level of below 3 mg/dL; (II) drain discharge volume of less than 500 mL/day; and (III) no macroscopic signs of bleeding or infection in the drain discharge. The drains were removed on POD 3 between January 2012 and February 2013 (POD 3 group) and on POD 1 between February and December 2013 (POD 1 group) if the early removal criteria were fulfilled on POD 3 in the POD 3 group and on POD 1 in the POD 1 group. In cases not meeting the criteria, the drains were retained until the criteria were fulfilled. In cases whose drains were not removed on the predefined POD even though the patient had met the criteria, the reason was investigated.
Prophylactic antibiotics (first-generation cephalosporin) were administered for 3 days. Abdominal ultrasonography and/or computed tomography scanning was performed if the patient developed a fever of more than 37.5 °C on or after POD 4 or if the patient’s abdominal symptoms and/or laboratory data worsened. No radiological or surgical interventions were considered in patients with asymptomatic fluid collection.
Measurement and definitions
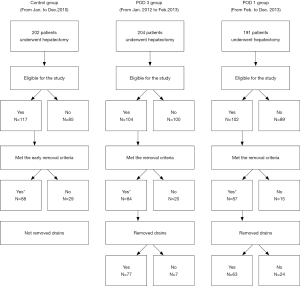
First, patients eligible for the present study were classified as to whether they met the early removal criteria on POD 3 in the control and POD 3 groups and on POD 1 in the POD 1 group. Secondly, patients meeting the criteria were classified as to whether the drains were actually removed on the predefined POD in the POD 3 and POD 1 groups (Figure 1).
In patients meeting the early removal criteria, the background characteristics, surgical outcomes, and postoperative outcomes were compared between the control and POD 3 groups and between the POD 3 and POD 1 groups. Drain infection was defined as a positive bacterial culture of the drain fluid. Bile leakage was defined as fluid with a bilirubin concentration at least 3 times greater than the serum bilirubin concentration in the abdominal drain or in the intra-abdominal fluid on or after POD 3 according to the definition and grading criteria of the International Study Group of Liver Surgery (ISGLS) (25). Grade A bile leakage caused no change in patients’ clinical management. Grade B bile leakage required active therapeutic intervention but was manageable without relaparotomy, whereas in grade C bile leakage, relaparotomy was required.
Postoperative outcomes were also evaluated in patients whose drains were actually removed on the predefined postoperative day, in patients whose drains were not removed on the predefined postoperative day though the early removal criteria were fulfilled, and in patients not meeting the criteria.
Statistical analysis
The statistical analyses were performed using the Wilcoxon rank sum test for continuous variables and the X2 test for categorical variables. Statistical significance was defined as P <0.05. For continuous variables, the medians with ranges were presented. For categorical variables, the number of patients and the proportion were presented. All the statistical calculations were performed using JMP Pro 9.0 (SAS Institute Inc., Cary, NC, USA).
Results
Between January and December 2010, a total of 202 consecutive patients underwent a hepatectomy (Figure 1). Of these, 117 patients were eligible for the present study and were analyzed as the control group. Eighty-five patients were excluded because of the simultaneous resection of other organs (n=33), an indocyanine green retention rate at 15 min ≥20% (n=17), an age of less than 20 years or over 80 years (n=16), bilioenteric reconstruction (n=12), severe co-morbidity (n=4), or laparoscopic liver resection (n=3). Among the eligible patients, 88 patients met the early removal criteria on POD 3.
Between January 2012 and February 2013, a total of 204 consecutive patients underwent a hepatectomy. Of these, 104 patients were eligible for the present study and were analyzed as the POD 3 group. One hundred patients were excluded because of the simultaneous resection of other organs (n=43), an indocyanine green retention rate at 15 min ≥20% (n=18), laparoscopic liver resection (n=17), bilioenteric reconstruction (n=9), an age of less than 20 years or over 80 years (n=7), or severe co-morbidity (n=6). Among the eligible patients, 84 patients met the early removal criteria on POD 3. The drains were actually removed on POD 3 in 77 patients. However, the drains were not removed in the remaining 7 patients because the doctors in charge decided it was better not to remove the drains at that time.
Between February and December 2013, a total of 191 consecutive patients underwent a hepatectomy. Of these, 102 patients were eligible for the present study and were analyzed as the POD 1 group. Eighty-nine patients were excluded because of the simultaneous resection of other organs (n=26), bilioenteric reconstruction (n=22), laparoscopic liver resection (n=20), an age of less than 20 years or over 80 years (n=8), severe co-morbidity (n=7), or an indocyanine green retention rate at 15 min ≥20% (n=6). Among the eligible patients, 87 patients met the early removal criteria on POD 1. The drains were actually removed on POD 1 in 63 patients. However, the drains were not removed in the remaining 24 patients.
Among the patients who met the early removal criteria, the background patient characteristics and surgical outcomes were similar between the control and POD 3 groups and between the POD 3 and POD 1 groups except for the proportion of patients who underwent a repeat hepatic resection, the operative duration, and the proportion of patients who received a thoracotomy (Table 1). The operative duration was shorter in the POD 3 group, presumably because of the smaller number of repeat hepatic resections in this group. A thoracotomy has been used in fewer patients in recent years.

Full table
As for the postoperative outcomes, the median duration of the postoperative hospital stay was shorter in the POD 3 group (11 days; range, 7–60 days) than in the control group (14 days; range, 7–41 days) (P<0.0001) (Table 2). Though the incidence of drain infection was lower in the POD 3 group (1.2%) than in the control group (5.7%), the incidence was as high in the POD 1 group (5.8%) as it was in the control group. In all the patients with drain infection in the POD 1 group, the drains were not actually removed on POD 1 and were retained for more than 9 days. The incidence of grade A bile leakage according to the ISGLS definition was highest in the control group (23.9%), since it is difficult to detect grade A bile leakage if the drains are removed early. No special treatment was provided for these patients. Meanwhile, the proportion of grade B bile leakage was highest in the POD 1 group (5.7%). In patients with grade B bile leakage, drains were retained until the bile leakage improved. In cases without improvement, endoscopic nasobiliary drainage (ENBD) was performed. If drains were not effective or had already been removed, percutaneous puncture was performed. The incidence of percutaneous puncture was similar in all the groups.
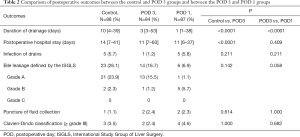
Full table
The proportion of patients with complications ≥grade III was highest (4.6%) in the POD 1 group. Except for patients requiring a percutaneous puncture, two patients had complications ≥grade III in each of the control and POD 1 groups. In the control group, one required incisional drainage because of a wound infection and the other required drainage under a laparotomy because of an infected hematoma. In the POD 1 group, one required coronary artery bypass grafting because of a postoperative myocardial infarction and the other required ENBD because of bile leakage. No deaths occurred in this study.
From the results presented in Table 2, the incidences of grade B bile leakage and complications ≥grade III were highest in the POD 1 group. However, the incidences were almost the same as those in the other groups when the comparisons were limited to those patients whose drains were actually removed on the predefined postoperative day (Table 3). Drain infection was rarely seen in these patients.
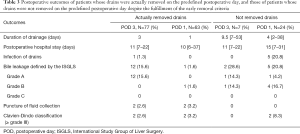
Full table
The postoperative outcomes of the patients whose drains were not removed on the predefined postoperative day despite the fulfillment of the early removal criteria are also presented in Table 3. In the POD 3 group, only one patient experienced a clinically significant complication (i.e., grade B bile leakage). Meanwhile, in the POD 1 group, 4 patients experienced grade B bile leakage and 2 patients had complications ≥ grade III.
The reasons why the drains were not removed on the predefined postoperative day even though the patient had met the early removal criteria are presented in Table S1. In the POD 3 group, the most common reason was a concern regarding bile leakage based on the intraoperative findings. However, in the POD 1 group, other concerns based on the intraoperative findings were also included.
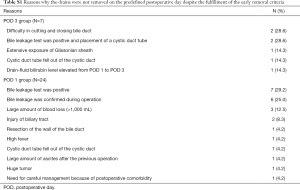
Full table
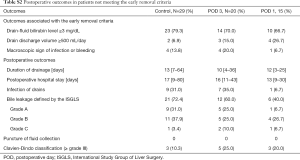
The postoperative outcomes of the patients who did not meet the early removal criteria are presented in Table S2. The proportions of patients with Grade B or C bile leakage and complications ≥ grade III were relatively high in all the groups. In patients with grade C bile leakage, macroscopic bile leakage became apparent on the next day of hepatectomy. Closure of bile leakage, abdominal lavage, and placement of a cystic duct tube was performed. In addition to patients with grade C bile leakage, one patient in the POD 3 group required re-operation because of postoperative bleeding.
Full table
Discussion
In the present study, the application of the early removal criteria for drain removal on POD 3 reduced the length of the postoperative hospital stay and the incidence of drain infection without impairing safety. To remove drains safely on POD 1, however, not only these criteria but also the intraoperative findings must be considered. Drain removal based on these clinical findings is safe and useful for identifying patients with a high risk of complications.
Before conducting the analysis, a decrease in the incidence of retrograde infection and a shortening of the postoperative hospital stay were expected as advantages of early drain removal. Indeed, the incidence of drain infection among patients who met the early removal criteria was lower in the POD 3 group than in the control group (Table 2), and the incidence among patients whose drains were actually removed was also lower in the POD 1 group (Table 3). As a result, among all the patients eligible for the study, the incidence of drain infection decreased from 12.0% (14 out of 117 patients, control group) to 6.7% (7 out of 104 patients, POD 3 group) and 5.9% (6 out of 102 patients, POD 1 group). The median duration of the postoperative hospital stay also decreased from 14 days (range, 7–160 days; control group) to 12 days (range, 7–60 days; POD 3 group) and 11 days (range, 6–37 days; POD 1 group) in all the eligible patients.
Meanwhile, the occurrence of bile leakage and/or symptomatic fluid collection after drain removal were expected to be disadvantages of early drain removal. We previously advocated that drains should be retained for a longer period because 37% of bile leakage complications were diagnosed on or after POD 3 (17). However, in the present study, most of the patients with a high risk for bile leakage were identified no later than POD 3 (Table 2) or POD 1 with the aid of the intraoperative findings (Table 3). The more stringent criteria used in the present study might have enabled the identification of the patients with a high risk for bile leakage during the early postoperative period. Regarding symptomatic fluid collection, the incidence of percutaneous puncture was almost the same among groups (Table 2). As mentioned above, puncture was performed for symptomatic fluid collection when drains were not effective or had already been removed. Among 5 patients who underwent puncture (Table 2), bilirubin concentration was elevated in 2 patients and bacterial culture was positive in 3 patients. The symptoms soon got better after puncture in all the patients. The safety of drain removal on POD 2 or on POD 3 was also presented in some previous reports though the criteria for drain removal were a bit different from ours (26,27).
Compared with no drain management, the biggest advantages of prophylactic drain placement are early detection and treatment of bleeding and bile leakage. In patients not meeting the early removal criteria, drain placement was especially beneficial because we could safely manage patients with high incidences of grade B or C bile leakage and complications ≥grade III (Table S2). In patients whose drain discharge was bloody, monitoring of drain discharge was helpful especially on the next day of operation. Since the mortality rate for hepatectomy at our institute is near-zero (28), drain placement is indispensable, at least in high-risk patients, to maintain safety.
As for the clinical features of high-risk patients identified, 20 out of 104 patients (19.2%) in the POD 3 group who did not meet the early removal criteria on POD 3 were considered to be high risk of complications (Table S2). The incidence of grade B or C bile leakage was 35% and one patient underwent re-operation because of postoperative bleeding. In patients with massive ascites (drain discharge volume ≥500 mL/day on POD 3), drains were removed within the 9th POD with the use of diuretics. In the POD 1 group, 39 out of 102 patients (38.2%) who did not meet the early removal criteria on POD 1 (Table S2) or for whom the intraoperative findings had led to some concerns (Tables 3,S1) were identified as having a high risk. The incidence of grade B or C bile leakage was 23.1% and drains were removed within the 14th POD in patients with massive ascites. Among the 39 patients, drains were removed on POD 3 in 17 patients. Postoperative course was uneventful in the 17 patients.
The results of the present trial, suggesting the safety and efficacy of early drain removal, provide important fundamental data for determining optimal drain management in the future. Hepatectomy at our institute includes anatomical resections for hepatocellular carcinoma (29), non-anatomical partial resections for colorectal liver metastasis even with multiple tumors (30), repeat resections (31,32), and so on. Liver transection is performed in the manner described above in the Methods section (22). The present results may be applicable to other institutes performing hepatectomy in the same manner. Meanwhile, in patients undergoing complicated parenchymal-sparing hepatectomy or repeat resection, RCTs have not yet adequately evaluated the need for prophylactic drains (6-11). Based on the present results, we are now planning to evaluate the safety and efficacy of no drain management in low-risk patients.
We have prioritized the safety of patients in adopting the early removal of drains. As a result, we have changed our policy for drain removal in a step-by-step manner, and the doctors in charge did not remove drains in some patients even though they fulfilled the early removal criteria. We did not perform an RCT because, at the time, we were not convinced of the safety of early removal. Though the differences in the background characteristics of the patients became a limitation of the present study, we were able to adopt the early removal of drains safely.
Another limitation was the relatively small sample size for evaluating the incidences of bile leakage, drain infection, percutaneous puncture, and complications ≥ grade III. As the incidences of these complications were less than 10%, we could not obtain statistically significant results.
In conclusion, the results of the present study indicated that drain removal on POD 1 based on the early removal criteria and intraoperative findings is safe and useful. In cases with some concern based on the intraoperative findings, drain removal on POD 3 in patients who meet the early removal criteria is worth considering. Though some low-risk patients can possibly be managed safely without abdominal drains, careful attention to the intraoperative findings is needed when selecting candidates.
Acknowledgements
The authors thank Y. Sugawara, T. Aoki, and T. Ishizawa for their contribution to this study.
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/atm.2020.04.04). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. This study was approved as project number 11660 by the Graduate School of Medicine and Faculty of Medicine, the University of Tokyo Research Ethics Committee.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Gurusamy KS, Samraj K, Davidson BR. Routine abdominal drainage for uncomplicated liver resection. Cochrane Database Syst Rev 2007;18:CD006232. [PubMed]
- Shrikhande SV, Barreto SG, Shetty G, et al. Post-operative abdominal drainage following major upper gastrointestinal surgery: single drain versus two drains. J Cancer Res Ther 2013;9:267-71. [Crossref] [PubMed]
- Zhang W, He S, Cheng Y, et al. Prophylactic abdominal drainage for pancreatic surgery. Cochrane Database Syst Rev 2018;6:CD010583. [PubMed]
- Wang Z, Chen J, Su K, et al. Abdominal drainage versus no drainage post-gastrectomy for gastric cancer. Cochrane Database Syst Rev 2015.CD008788. [PubMed]
- Zhang HY, Zhao CL, Xie J, et al. To drain or not to drain in colorectal anastomosis: a meta-analysis. Int J Colorectal Dis 2016;31:951-60. [Crossref] [PubMed]
- Belghiti J, Kabbej M, Sauvanet A, et al. Drainage after elective hepatic resection. A randomized trial. Ann Surg 1993;218:748-53. [Crossref] [PubMed]
- Fong Y, Brennan MF, Brown K, et al. Drainage is unnecessary after elective liver resection. Am J Surg 1996;171:158-62. [Crossref] [PubMed]
- Fuster J, Llovet JM, Garcia-Valdecasas JC, et al. Abdominal drainage after liver resection for hepatocellular carcinoma in cirrhotic patients: a randomized controlled study. Hepatogastroenterology 2004;51:536-40. [PubMed]
- Liu CL, Fan ST, Lo CM, et al. Abdominal drainage after hepatic resection is contraindicated in patients with chronic liver diseases. Ann Surg 2004;239:194-201. [Crossref] [PubMed]
- Sun HC, Qin LX, Lu L, et al. Randomized clinical trial of the effects of abdominal drainage after elective hepatectomy using the crushing clamp method. Br J Surg 2006;93:422-6. [Crossref] [PubMed]
- Kim YI, Fujita S, Hwang VJ, et al. Comparison of Abdominal Drainage and No-drainage after Elective Hepatectomy: A Randomized Study. Hepatogastroenterology 2014;61:707-11. [PubMed]
- Gavriilidis P, Hidalgo E, de'Angelis N, et al. Re-appraisal of prophylactic drainage in uncomplicated liver resections: a systematic review and meta-analysis. HPB (Oxford) 2017;19:16-20. [Crossref] [PubMed]
- Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 2004;240:205-13. [Crossref] [PubMed]
- Butte JM, Grendar J, Bathe O, et al. The role of peri-hepatic drain placement in liver surgery: a prospective analysis. HPB (Oxford) 2014;16:936-42. [Crossref] [PubMed]
- Squires MH 3rd, Lad NL, Fisher SB, et al. Value of primary operative drain placement after major hepatectomy: a multi-institutional analysis of 1,041 patients. J Am Coll Surg 2015;220:396-402. [Crossref] [PubMed]
- Shwaartz C, Fields AC, Aalberg JJ, et al. Role of Drain Placement in Major Hepatectomy: A NSQIP Analysis of Procedure-Targeted Hepatectomy Cases. World J Surg 2017;41:1110-8. [Crossref] [PubMed]
- Kyoden Y, Imamura H, Sano K, et al. Value of prophylactic abdominal drainage in 1269 consecutive cases of elective liver resection. J Hepatobiliary Pancreat Sci 2010;17:186-92. [Crossref] [PubMed]
- Shirata C, Hasegawa K, Kokudo T, et al. Surgical site infection after heaptectomy hepatectomy for hepatocellular carcinoma. Dig Surg 2018;35:204-11. [Crossref] [PubMed]
- Yamazaki S, Takayama T, Moriguchi M, et al. Criteria for drain removal following liver resection. Br J Surg 2012;99:1584-90. [Crossref] [PubMed]
- Mitsuka Y, Yamazaki S, Yoshida N, et al. Prospective Validation of Optimal Drain Management “The 3 x 3 Rule” after Liver Resection. World J Surg 2016;40:2213-20. [Crossref] [PubMed]
- Makuuchi M, Kosuge T, Takayama T, et al. Surgery for small liver cancers. Semin Surg Oncol 1993;9:298-304. [Crossref] [PubMed]
- Ichida A, Hasegawa K, Takayama T, et al. Randomized clinical trial comparing two vessel-sealing devices with crush clamping during liver transection. Br J Surg 2016;103:1795-1803. [Crossref] [PubMed]
- Uetsuji S, Kwon AH, Komada H, et al. Clinical evaluation of closed suction drainage following heaptectomy. Surg Today 1997;27:298-301. [Crossref] [PubMed]
- Mangram AJ, Horan TC, Pearson ML, et al. Guideline for prevention of surgical site infection, 1999. Centers for Disease Control and Prevention (CDC) Hospital Infection Control Practices Advisory Committee. Am J Infect Control 1999;27:97-132. [Crossref] [PubMed]
- Koch M, Garden OJ, Padbury R, et al. Bile leakage after hepatobiliary and pancreatic surgery: a definition and grading of severity by the International Study Group of Liver Surgery. Surgery 2011;149:680-8. [Crossref] [PubMed]
- Hokuto D, Nomi T, Yasuda S, et al. The safety of the early removal of prophylactic drainage after liver resection based solely on predetermined criteria: a propensity score analysis. HPB 2017;19:359-64. [Crossref] [PubMed]
- Inoue Y, Imai Y, Kawaguchi N, et al. Management of abdominal drainage after hepatic resection. Dig Surg 2017;34:400-10. [Crossref] [PubMed]
- Imamura H, Seyama Y, Kokudo N, et al. One thousand fifty-six hepatectomies without mortality in 8 years. Arch Surg 2003;138:1198-206. [Crossref] [PubMed]
- Shindoh J, Makuuchi M, Matsuyama Y, et al. Complete removal of the tumor-bearing portal territory decreases local tumor recurrence and improves disease-specific survival of patients with hepatocellular carcinoma. J Hepatol 2016;64:594-600. [Crossref] [PubMed]
- Hasegawa K, Takahashi M, Ohba M, et al. Perioperative chemotherapy and liver resection for hepatic metastases of colorectal cancer. J Hepatobiliary Pancreat Sci 2012;19:503-8. [Crossref] [PubMed]
- Mise Y, Hasegawa K, Shindoh J, et al. The Feasibility of Third or More Repeat Hepatectomy for Recurrent Hepatocellular Carcinoma. Ann Surg 2015;262:347-57. [Crossref] [PubMed]
- Oba M, Hasegawa K, Shindoh J, et al. Survival benefit of repeat resection of successive recurrences after the initial hepatic resection for colorectal liver metastases. Surgery 2016;159:632-40. [Crossref] [PubMed]


