
Accurate fixation of complicated comminuted femur fracture with customized LCP referencing a life-size 3D-printed model: a case report
Introduction
The fixation of comminuted mid-distal femur fracture is challenging in clinical practice, mainly due to the high degree of comminution and malformation caused by traction of the attached muscles (1,2). Notably, there is a lack of mechanical support on the medial side of the fracture when the medial cortex is pulverized. This condition is more prone to complications such as valgus deformity, fracture nonunion, and internal fixation failure (3).
Although various treatments such as skin and bone traction, external fixation, interlocking intramedullary nails, and anatomical plates have been attempted, some complications remain unresolved (4). For instance, long-term skin and bone traction may cause joint stiffness, deformity, and complications related to bed confinement (5). External fixation is potentially complicated by needle infection and limited functionality (6). The application of interlocking intramedullary nail may experience bone union linked to difficulties in the anatomical reduction of comminuted fracture (7). Meanwhile, open reduction and internal fixation (ORIF) with an anatomical plate requires reduction of the fracture fragment by periosteum removal over a large area, which may lead to delayed bone healing (8).
A lateral locking compression plate (LCP) has recently been recommended for comminuted femur fracture fixation for its excellent mechanical characteristics (9). Maximum protection of bone fracture fragments and the surrounding blood supply can be achieved by minimally invasive percutaneous plate osteosynthesis (MIPPO) technology. These provide a good biological environment for fracture healing, thereby reducing bone graft rate and the occurrence of nonunion (10). However, this surgical procedure is still limited by poor alignment correction and insufficient bone fragment reduction (11).
Here we report the application of three-dimensional (3D) computed tomography (CT) scanning to print a life-size 3D model of a patient’s contralateral femur using a mirroring technique. The 3D-printed model served as a preoperative tool for preshaping the customized LCP and simulating implantation. The preshaped LCP was consistent with the femoral anatomy, which was beneficial for fracture fragment reduction and ligament correction. The MIPPO technique was then used to treat the multisegment comminuted femur fracture, with the patient achieving good clinical recovery. The combination of these approaches should be considered for the treatment of comminuted femoral fractures.
Case presentation
The study was conducted in accordance with the principles outlined in the Declaration of Helsinki, and was approved by the Ethics Committee of the Second Hospital of Jilin University (No. 2019025). The patient provided written, informed consent to participate. Data were kept anonymous to protect the patient’s privacy.
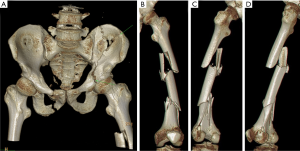
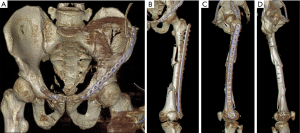
A 35-year-old male was admitted to the hospital with high fall injury. Physical examination revealed obvious external rotation and deformity (shortening) of the left lower extremity, with tenderness and longitudinal throbbing pain as well as bone squeaking and rubbing. Subcutaneous ecchymosis was visible on the lateral side of the greater trochanter and buttock. This patient denied previous illness and surgery history, and family members have no inherited diseases. X-ray (Figure 1) and 3D CT (Figure 2) reconstruction revealed that the patient had multiple fractures including a left acetabular double column fracture with quadrilateral body displacement to the medial side (AO classification: C1.3), combined with left iliac wing and right pubic fractures. There were multiple comminuted fractures in the left femur with significant displacement, and several irregular fracture lines were detected between the lateral femoral condyle and intercondylar fossa with no obvious displacement. A left tibia avulsion fracture of the posterior cruciate ligament (PCL) was also observed.

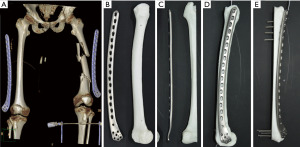
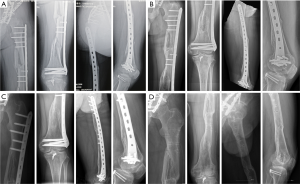
The diagnosis and treatment flow chart of the patient, as shown in Figure 3. The 3D CT scan confirmed that even the longest available 14-hole LCP was insufficient for fracture fixation (Figure 4A). A customized 17-hole LCP (length =400.0 mm, with a 4.5-mm cortical screw and 5.0-mm locking screw) was designed and fabricated. A resin model was 3D-printed based on the contralateral femur using the mirror principle (Figure 4B,C), and was used to preshape the LCP and simulate screw implantation. The simulation showed that the self-designed plate could attach perfectly to the outer side of the 3D-printed femur model after preshaping and that 4 to 5 locking screws were sufficient for distal and proximal fixation (Figure 4D,E). Emergency traction of the left tibia tubercle was performed and a large distractor was fixed across the knee joint for temporary external fixation to maintain the positions of bone fragments (Figure 5) and gain time for the fabrication of a customized bone plate, and to reduce the size of the fracture prior to surgery. Two weeks later, the pelvis fractures were fixed by ORIF and after 1 week, the femur fracture and tibia avulsion fracture of the PCL were treated simultaneously. This article focuses on the treatment of multisegment comminuted femur fracture by customized LCP using the MIPPO technique.
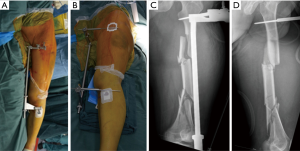
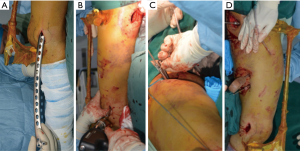
With the patient in the supine position, the left lower extremity was externally rotated by 30° and elongated by 0.5 cm based on the preoperative X-ray. Accordingly, the stretcher was rotated and shortened by the same angle to correct the deformity. A 3.5-cm longitudinal incision was then made at the center of the lateral femoral condyle by a distal approach. A proximal incision was made by the original approach for the pelvis operation (after removing 5.0 cm of suture), and the lateral femoral muscle was partially cut at the insertion point of the greater trochanter to expose the proximal femur. The plate was inserted (Figure 6A) and temporarily fixed with Kirschner wires (Figure 6B,C), and the free bone fragment in the middle was fixed with 3 screws (Figure 6D). The fracture line and plate position were confirmed by fluoroscopy (Figure 7A,B). A locking screw was fixed at each end (Figure 7C,D). Finally, 4 and 3 locking screws were placed at the distal and proximal ends, respectively (Figure 7E,F). After internal fixation, passive exercises were performed on the patient under anesthesia.
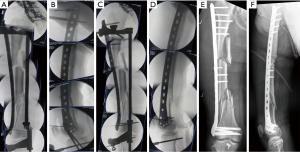
Postoperative 3D CT confirmed that the left femur line was basically restored, with the internal fixation in a good position (Figure 8). On day 3 after surgery, positive and passive flexion and extension exercises of the knee joint were started. After 6 weeks, partial weight-bearing walking was achieved and at 3 months, total weight-bearing walking was recommended. An X-ray examination at 5 months showed no displacement at the fracture end, and the fracture line was blurred by the formation of a large amount of callus (Figure 9A). X-ray examination at 1 year showed good lower limb alignment and complete plasticity of the bone structure (Figure 9B). The plate was removed 3 years after the surgery (Figure 9C,D), at which time the patient showed good limb function (Figure 10).

Discussion
Subjecting the femoral shaft to high-impact injury can lead to comminuted fracture (12). Successful surgery depends on effective reduction and internal fixation of the fracture with maximal preservation of the blood supply at the fracture site (13). The locking mechanism of the LCP has good angle stability, and the screws and plate are combined into an internal fixation bracket. The plate can be inserted into the incision with the MIPPO technique and attached to the periosteal channel, with 4 to 6 screws installed at the fracture ends. The bone surface does not need to be in close contact with the plate; the fracture end is not exposed, and the blood supply is preserved as much as possible, thus protecting local tissue and creating an environment that promotes bone healing (14). However, it was reported that a lateral LCP is associated with a relatively high rate (up to 30%) of complications including nonunion, delayed union, and implant failure, mainly due to poorly reset fracture fragments, uncorrected lower limb alignment, and periosteal stripping during surgery (15).
The reason for the distal end of the large distractor crossing the knee joint is that a femoral condyle fracture has limited fixation strength, which affects implantation of the bone plate and increases the risk of infection of the distal incision. The rationale for using a large distractor was to restore and maintain the femoral force line and length; in the process of pelvic and acetabular fracture reduction and fixation, this allowed traction and rotation without secondary damage.
A plate with insufficient supporting length is presumed to be the main cause of fracture nonunion and internal fixation fracture (16). However, it has also been suggested that the lateral LCP has unstable eccentric fixation due to inadequate support on the medial side when subjected to longitudinal load. This causes significant strain at the fracture end, which affects callus formation and delays or prevents healing. At the same time, stress is concentrated in the lateral plate over a prolonged period, which can induce internal fixation failure (17). Life-size 3D-printed models that reflect the actual size and structure of fractures have been widely used in the field of trauma surgery in recent years as a reference for designing surgical schemes and for preoperative simulation (18). The use of 3D-Printed model in this study obviously reduced the operation difficulty and improved surgical accuracy, which can further prevent the internal fixation failure to some degree (19).
The customized LCP had several advantages. (I) The retractor effectively restored the femoral alignment line and limb length, and helped to adjust the position of bone fragments during the operation. (II) The bone plate was well designed and pre-bent according to the 3D-printed resin model. (III) The effective fixation of multiple bone segments was completed at one time under minimally invasive conditions, allowing functional exercises to be performed soon after surgery. However, this case also had the following limitations. (I) The femoral alignment line was not fully adjusted and the lower limb had a slight valgus deformity. (II) The bone plate should have had a lag screw near the fracture line at the distal end that could correct the valgus deformity and increase the fixation strength of the femur. (III) The large free bone fragment at the proximal end was not reset; the use of percutaneous bundling wire can achieve superior resetting. (IV) An eccentrically fixed elongated bone plate experiences significant strain and stress, thereby increasing the probability of fatigue fractures.
Conclusions
A novel strategy was developed for the treatment of multisegment comminuted femur fracture with a customized LCP that involved the MIPPO technique along with a 3D-printed model. The patient showed good limb function at the 3-year follow-up without any complications. Therefore, this procedure is worth considering as an option for accurate fixation of comminuted mid-distal femur fractures.
Acknowledgments
Funding: This work was supported by the National Natural Science Foundation of China (grant No. 81671804 and 81772456); Scientific Development Program of Jilin Province (grant No. 20190304123YY, 20180623050TC, and 20180201041SF); Program of Jilin Provincial Health Department (grant No. 2019SCZT001, 2019SCZT014, and 2019SRCJ001); Cultivation Program from the Second Hospital of Jilin University for National Natural Science Foundation (grant No. KYPY2018-01); and Youth Talents Promotion Project of Jilin Province (grant No. 192004).
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/atm.2020.03.115). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Anaya R, Rodriguez M, Gil JM, et al. Evaluation of a strategy to shorten the time to surgery in patients on antiplatelet therapy with a proximal femur fracture (AFFEcT Study): Study protocol for a multicenter randomized controlled clinical trial. Medicine (Baltimore) 2019;98:e15514. [Crossref] [PubMed]
- Bai Y, Zhang X, Tian Y, et al. Incidence of surgical-site infection following open reduction and internal fixation of a distal femur fracture: An observational case-control study. Medicine (Baltimore) 2019;98:e14547. [Crossref] [PubMed]
- Neumann MV, Südkamp NP, Strohm PC. Management of femoral shaft fractures. Acta Chir Orthop Traumatol Cech 2015;82:22-32. [PubMed]
- Callan JP. New intramedullary nail aids femur fracture healing. JAMA 1979;241:1089. [Crossref] [PubMed]
- Koerner MR, Young LE, Daniel A, et al. Does traction decrease the need for open reduction in femoral shaft fractures treated within 24 hours? J Surg Orthop Adv 2018;27:303-6. [PubMed]
- Biswas SP, Kurer MH, Mackenney RP. External fixation for femoral shaft fracture after Stanmore total knee replacement. J Bone Joint Surg Br 1992;74:313-4. [Crossref] [PubMed]
- Sahu RL, Sikdar J. Fracture union in closed interlocking nail in femoral fracture. JNMA J Nepal Med Assoc 2010;49:228-31. [Crossref] [PubMed]
- Dodd AC, Salib CG, Lakomkin N, et al. Increased risk of adverse events in management of femur and tibial shaft fractures with plating: An analysis of NSQIP data. J Clin Orthop Trauma 2016;7:80-5. [Crossref] [PubMed]
- Shah MD, Kapoor CS, Soni RJ, et al. Evaluation of outcome of proximal femur locking compression plate (PFLCP) in unstable proximal femur fractures. J Clin Orthop Trauma 2017;8:308-12. [Crossref] [PubMed]
- Kumar A, Gupta H, Yadav CS, et al. Role of locking plates in treatment of difficult ununited fractures: A clinical study. Chin J Traumatol 2013;16:22-6. [PubMed]
- Kiyono M, Noda T, Nagano H, et al. Clinical outcomes of treatment with locking compression plates for distal femoral fractures in a retrospective cohort. J Orthop Surg Res 2019;14:384. [Crossref] [PubMed]
- El Beaino M, Morris RP, Lindsey RW, et al. Biomechanical evaluation of dual plate configurations for femoral shaft fracture fixation. Biomed Res Int 2019;2019:5958631.
- Kanata S, Anastasiadis A. Open reduction and internal fixation of a proximal femoral shaft fracture in a patient with bilateral congenital hip disease. Case Rep Orthop 2018;2018:2070564.
- Wu D, Mao F, Yuan B, et al. Minimally invasive percutaneous plate osteosynthesis (MIPPO) combined with onionskin-like autologous bone grafting: A new technique for treatment of tibial nonunion. Med Sci Monit 2019;25:5997-6006. [Crossref] [PubMed]
- Henderson CE, Kuhl LL, Fitzpatrick DC, et al. Locking plates for distal femur fractures: Is there a problem with fracture healing? J Orthop Trauma 2011;25 Suppl 1:S8-14. [Crossref] [PubMed]
- Jackson M, Learmonth ID. The treatment of nonunion after intracapsular fracture of the proximal femur. Clin Orthop Relat Res 2002.119-28. [Crossref] [PubMed]
- Glassner PJ, Tejwani NC. Failure of proximal femoral locking compression plate: A case series. J Orthop Trauma 2011;25:76-83. [Crossref] [PubMed]
- Li QJ, Yu T, Liu LH, et al. Combined 3D rapid prototyping and computer navigation facilitate surgical treatment of congenital scoliosis: A case report and description of technique. Medicine (Baltimore) 2018;97:e11701. [Crossref] [PubMed]
- Zou Y, Han Q, Weng XS, et al. The precision and reliability evaluation of 3-dimensional printed damaged bone and prosthesis models by stereo lithography appearance. Medicine (Baltimore) 2018;97:e9797. [Crossref] [PubMed]



