
Statistical analysis plan for aggressive hydraTion in patients with ST-elevation myocardial infarction undergoing primary percutaneous coronary intervention to prevenT contrast-induced nephropathy (ATTEMPT) study
Introduction
Patients who have ST-segment elevation myocardial infarction (STEMI) carry a high-risk of contrast-induced acute kidney injury (CI-AKI) following primary percutaneous coronary intervention (pPCI) (1). However, for this high-risk group, the extent of the effects of optimal hydration strategy is yet to be fully established (2,3). The aggressive hydraTion in patients with ST-Elevation Myocardial infarction undergoing Primary percutaneous coronary intervention to prevenT contrast-induced nephropathy (ATTEMPT) study is the first study to evaluate the peri-procedural aggressive hydration in STEMI patients undergoing pPCI (4). Here, we describe the statistical analysis plan (SAP) for the ATTEMPT study, prior to patient enrollment being completed (this was completed in June 2018) and the locking of the database for analysis.
This SAP was written by the study statistician and the principal investigator, both of whom were kept blind to the course of treatment allocated to the patients. We prospectively defined each analysis described in this SAP.
Methods
Overview of design
The ATTEMPT study is a multicenter, randomized controlled trial which is investigator-based and open label in nature. A total of 560 patients with STEMI undergoing pPCI will be randomized (1:1) to undergo treatment either by peri-procedural aggressive hydration (treatment group) or general hydration (control group). The ATTEMPT study could prove valuable for the possible identification of optimal hydration regimens for STEMI patients undergoing pPCI (4).
Inclusion criteria
All consecutive patients with STEMI who were at least 18 years of age and were prepared for pPCI were taken into consideration for enrollment in the study.
Exclusion criteria
- Contrast medium administration within the 2 weeks prior to the procedure or the following 3 days;
- End-stage renal failure or renal transplantation, and refusal of pPCI or death while the procedure is taking place;
- Heart failure-induced cardiac shock or New York Heart Association class IV (these patients were excluded because intravenous hydration administration could potentially prove harmful);
- A recent acute kidney injury, which was considered to be an absolute increase of 0.5 mg/dL in serum creatinine (SCr) over baseline in the 24 hours prior;
- The existence of lactation, pregnancy;
- A tumor of a malignant nature or a predicted life expectancy of 1 year or less;
- An allergic reaction induced by contrast medium, peri-procedural receipt of metformin, or non-steroidal anti-inflammatory drugs in the 2 days prior and while the study is taking place;
- Planned renal catheterization or heart valvular surgery.
Randomization
All patients meeting the eligibility criteria and provided informed consent will be randomized into two study groups. A computer will carry out randomization of eligible patients by producing numbers at random at a 1:1 ratio. Randomization will be accomplished with using a block random method with 8 units in each group. Some offset or variability will be inserted to prevent anticipation of the next treatment. Randomization will be stratified based on age (<60, 60–75, >75 years), sex (male or female), and STEMI location (anterior wall or no-anterior wall). Study coordinators at each site will be responsible for obtaining a randomized treatment assignment for each eligible patient. Study sites will be provided with a web-based randomization program for this purpose. This web-based http://crdms.echobelt.org program will be tested at each site prior to the start of the trial and will be reviewed. Since this is an open-label study, the procedure of blinding will not take place.
Sample size
The total sample size of 560 patients was calculated based on our previous findings. The incidence of primary end point was estimated to decrease to 11.5% (50% relative reduction) in the aggressive hydration group from 23% in the control group with general hydration (5). We established a sample size according to nQuery + nTerim 3.0 (Statistical Solutions Ltd, Ireland) by employing a 2-sided χ2 test, a power of 90%, a significance level of 0.05, and a dropout rate <20%.
The formal statement of the null hypothesis
We fully describe the CI-AKI outcome based on the aggressive hydration versus general hydration intervention. The null hypothesis is that the two treatment groups (aggressive hydration and control) do not differ in terms of the proportion of subjects who experience CI-AKI. The alternative hypothesis is that the absolute difference in the incidence of CI-AKI between the aggressive hydration group and the control group.
Intervention
A pre-procedural loading dose 250 mL of normal saline for 30 minutes (125 mL for patients with congestive heart failure, Killip II/III or NYHA III) will be administered to the patients in the treatment group in an emergency department or cardiac catheterization lab over 30-minutes prior to the pPCI. After this, the patients will receive intravenous hydration at a general rate (1 or 0.5 mL/kg/h for patients with congestive heart failure, Killip II/III or NYHA III) until LVEDP measurement.
Patients will then undergo 4 hours of post-procedural aggressive hydration guided by LVEDP [5 mL/kg/h (LVEDP <13 mmHg), 3 mL/kg/h (LVEDP 13–18 mmHg), 1.5mL/kg/h (LVEDP >18 mmHg), and 0.5 mL/kg/h (LVEDP >20 mmHg)] and continuous intravascular hydration at the normal rate for the 24 hours following PCI. Control group patients will receive peri-procedural general hydration with ≤500 mL normal saline (within 6 hours) at a normal rate (0.5 or 1 mL/kg/h).
Interim analysis
According to the study design, interim analysis to determine if either intervention shows a substantial beneficial effect will not be carried out.
Timing of analysis
At the end of the study, the final audit should be performed usually within four to six weeks of the end of the last follow-up of the last subject in the study center. The preparations and procedures for the study of closed visits are generally the same as for a regular supervisory visit. The last patient was enrolled on 10th June 2018.
Analysis principles
- Analysis is to be conducted based on adjusted intention-to-treat (ITT) (randomization must be finished before emergency surgery, and we will not include the patients who need to be excluded from the final analysis).
- We will not impute missing values, unless specified. The number of subjects included in an analysis will be reported if there is a substantial amount of missing data. The last observations will not be carried forward. Multiple imputation will be used if >5% of patients have missing data on the primary outcome.
- Each of the tests will be two-tailed, and a P value of less than 0.05 will be considered to be statistically significant.
- Only analyses conducted up to 1 year after randomization will feature in this analysis plan and in the primary manuscript.
- Pre-specified subgroup analyses will be conducted whether or not a statistically significant treatment effect on the primary outcome is seen across the total sample.
- We use the t-test for normally distributed continuous variables and expressed as mean ± SD, and the Wilcoxon rank-sum test was used in non-normal distribution variables and presented as median and interquartile range.
- For categorical variables, we used Pearson χ2 or Fisher’s exact tests to compare baseline characteristics and study’s endpoints between the aggressive and general hydration groups; these will be expressed as percentages.
- Logistic regression testing to assess whether the recorded treatment effect was consistent across random stratified variable (age, gender, STEMI location). Odds ratios will be reported alongside their related 95% CIs.
- Risk ratio (RR) and absolute risk difference (ARD) with their corresponding 95% confidence interval (CIs) are used to describe the interaction effect (primary, second, and safe events). The number needed to treat (NNT) for preventing one CI-AKI-related event was calculated by inverse of the ARD.
Analysis of primary outcome
The primary analysis will be based on adjusted intention to treat principles. Since the intervention is given and the primary outcome is observed for a very short duration (72 hours), we expect only a few dropouts or crossovers.
As ATTEMPT study’s protocol pointed out primary outcome would use multivariable logistic regression with (age, sex, creatinine clearance, and left ventricular ejection fraction). However, basic on principal component analysis, we have changed to use multivariable logistic regression to evaluate the intervention effect with random stratified variable [e.g., age (<60, 60–75, >75 years), gender, STEMI location]. The analysis for each variable will be performed by OR with their corresponding 95% CIs to describe the intervention effect. All tests will be two-tailed, and a P value less than 0.05 will be considered statistically significant.
Subgroup analyses
We will undertake analysis of five pre-specified subgroups defined by the following baseline criteria: age (<60, 60–75, >75 years), gender (Male or female), STEMI location (anterior wall or no-anterior wall), and LVEF (≥40% or <40%), eGFR (≥90 or <90 mL/minute/1.73 m2). eGFR formula (Modified relative dose response) = [186 × serum Cr (mg/dL)]^− 1.154 × age (yr) ^− 0.203 × (multiply by 0.742 for women).
Within each subgroup, summary measures will include raw counts and percentages within each treatment arm. The analysis for each subgroup will be performed by RR with their corresponding 95% CIs to describe the interaction effect. The results will be shown on a forest plot including the P-value for heterogeneity corresponding to the interaction term between the intervention and the subgroup variable.
Analysis of secondary outcomes
Our secondary objectives will be tested using χ2 tests, and the 95% CI of the rate difference of RR and ARD will be calculated using the method described by Altman et al (reported in Newcombe and recommended by the Food and Drug Administration and Clinical and Laboratory Standards Institute. The secondary end-points will be analyzed based on the adjusted ITT principle.
Sensitive analyses
To evaluate the stability of primary outcome, we will use logistic regression to analyze the influence of compliance and use baseline value comparison to assess the differences between the two groups of excluded cases. It will be performed by OR with their corresponding 95% CIs. All tests will be two-tailed, and a P value less than 0.05 will be considered statistically significant.
For patients: the volumes of urine and oral hydration (water in milliliters) in the 24 hours following the procedure will be recorded.
For medical staff: intravenous hydration information will be gathered in the 24 hours following the procedure. A preoperative renal function test and details on postoperative SCr, failure to hydrate according to protocol, and the absence of SCr will be obtained in the follow-up. All of this information, laboratory tests and vital signs will be carefully collected by the research staff.
Central effect analysis
To evaluate the central effect, we will use One-way analysis of primary outcome with different centers. We describe the central effect by OR with their corresponding 95% CIs. All tests will be two-tailed, and a P value less than 0.05 will be considered statistically significant.
Analysis of safety outcomes
One of the important adverse reactions to aggressive hydration is the increased risk of heart failure. We will record all information relating to acute heart failure: acute pulmonary edema, cardiogenic shock, and further auxiliary examination such as ECG, chest X-ray, laboratory assessment (with specific biomarkers), and echocardiography.
The Clinical Event Committee (CEC) will be responsible for determining the endpoints in clinical studies and avoiding deviations in event determination between centers in order to achieve a more accurate assessment of the test results. We will use RR and ARD with their corresponding 95% CIs to describe the safety endpoint.
Treatment of missing data
We conservatively estimate that up to 20% of subjects may be lost to follow-up SCr within 72 hours and exclusive patients. The site coordinators will make every effort to identify such subjects including at least two laboratory tests of SCr after pPCI. Multiple imputation will be used if >5% of patients have missing data on the primary outcome.
Statistical software
All data analyses will be performed using SAS version 9.4 (SAS Institute, Cary, NC, USA) and R soft-ware (version 3.6.1; R Core Team, Vienna, Austria).
Protocol deviation
Any program deviations need to be recorded, and the Guangdong Provincial Key Laboratory of Coronary Heart Disease will create a program deviation table to ensure that events are tracked correctly. The efficacy of the deviation basis will be determined. If sub-centers still experience serious program deviation after remedial training, the Data Monitoring Committee (DMC) may recommend the termination of the center in question. After consulting with the Executive Committee, subjects have the right to withdraw from this study, and the program will be reported to the main research unit Institutional Review Board as required.
Results
Flowchart of recruitment
The patient sorting processes throughout the different stages of the trial will be shown in the form of a Consolidated Standards of Reporting Trials diagram (Figure 1) (6-8).
The diagram will show the total numbers for eligible patients from those screened, patients included in the study, and explanations for those patients who were not included. Consent status will be outlined in a second diagram (Figure 2).
Patient characteristics and baseline comparisons
Comparisons of patients’ baseline characteristics will be set out according to treatment group, as shown in the tables (see Table S1-S4).
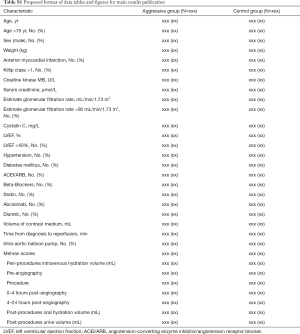
Full table
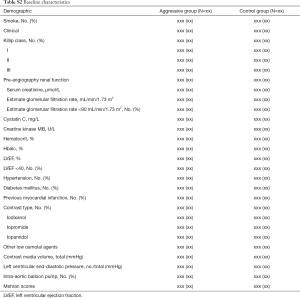
Full table

Full table
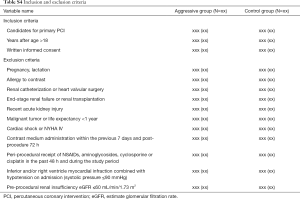
Full table
Study outcomes
The primary endpoint is CI-AKI, which is considered to be a >25% or 0.5 mg/dL increase in SCr from baseline in the 48–72 hours immediately following the procedure (Table 1, Tables S5,S6) (9).
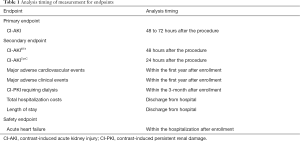
Full table

Full table

Full table
The secondary outcomes consist of: (I) CI-AKI, defined as a >50% or 0.3-mg/dL absolute increase in SCr from baseline in the 48 hours immediately after the procedure; (II) CI-AKI, defined as a >10% or 0.3-mg/dL absolute increase in serum cystatin-C during the 24 hours immediately following the procedure (9); (III) persistent renal damage, which is considered to be residual impairment of renal function demonstrated by a >25% reduction in creatinine clearance at 3 months compared with baseline (10); (IV) major adverse cardiovascular events, which include all-cause mortality, target vascular revascularization, and non-fatal myocardial infarction; (V) major adverse clinical events which take place in hospital following the procedure, including acute pulmonary edema, cardiogenic shock, stroke, clinically significant arrhythmias, and bleeding; (VI) total hospitalization costs; (VII) length of stay.
The safe outcome is Acute heart failure (AHF) during hospitalization, defined as signs/symptoms of heart congestion and/or hypoperfusion by physical examination and further auxiliary examination such as ECG, chest X-ray, laboratory assessment (with specific biomarkers), and echocardiography (11).
Primary outcome analysis
All consented and randomized subjects will be accounted for and reported in the CONSORT diagram for the study; however, only those randomized subjects who have started either intravenous hydration intervention or have finished test for SCr at least once on pre-procedure and 72 hours post-procedure (i.e., did not drop out or withdraw prior to the start of the allocated intervention) will be considered as an adjusted ITT subject to be included in the DMC reports and primary efficacy analysis.
Conclusions
The ATTEMPT study will investigate the efficacy and safety of adequate hydration during the perioperative period among patients who require pPCI treatment. This SAP is intended to minimize the analysis bias of the study.
Supplementary
Monitoring committee charter
Our study set up a data and safety monitoring committee (DSMB) to independently monitor the clinical trial process, data safety. DSMB consists of relevant field of experts who regularly evaluate the cumulative data from ongoing clinical trials. This charter outlines the roles and responsibilities of DSMB.
Clinical trial data and safety monitoring committee
DSMB member selection rules
To guarantee the integrity of the trial statistics, investigator or sponsor employees cannot join DSMB. In regard to to FDA requirements on DSMB composition, we have the following rules for member selection: (I) potential conflicts of interest for recommended DSMB members must be assessed; (II) people with significant conflicts of interest cannot join DSMB; (III) the information sent to DSMB members should not hinder objectivity or potential opposition to DSMB's appointment; (IV) this study’s DSMB members cannot be on the other related or competing products’ DSMB .
DSMB member composition
The DSMB of this study consists of three people (including the chairman of DSMB), including: biostatisticians, medical ethics experts, and toxicologists. The DSMB members of this study will remain in their positions until the end of the study.
DSMB members are required to support the clinical trial objectives and methods being monitored. If they do not agree with the research method, they should explain this to the sponsor and refuse the invitation.
Responsibility of DSMB
Purpose of DSMB
The main purpose of DSMB is to monitor data on treatment interventions to ensure the safety, efficacy, and integrity of clinical trials. In addition, DSMB assesses the progress of participant recruitment and makes recommendations to the sponsors, which are taken forward in the planning, modification or termination of studies.
DSMB general duties
- Reviewing research documents, informed consent, statistical analysis plans, and interim analysis plans.
- Safety assessments of the cumulative data of ongoing clinical trials to ensure subject safety.
- Evaluating the efficacy of the test cumulative data (if appropriate) according to pre-defined statistical principles.
- Monitoring the implementation of the study, including center patients’ enrollment, program violations, and shedding.
- Monitoring the accuracy, completeness, and timeliness of the data.
- Monitoring the compliance of researchers and subjects with the program.
- Reviewing all related files for DSMB.
- Studying the consistency of the evaluation of events by the centers.
- Maintaining equilibrium between groups of important prognostic variables.
- Overseeing the entry of important subgroups.
- In the course of the trial, considering the impact of external information on the study: if the results of other published studies or treatment progress could have an impact on the safety of the subject or the ethics of the study (It is provided by the researcher, DSMB members are not responsible for collecting this information).
- Advising the sponsor to continue, modify, suspend or terminate the study.
Furthermore, only DSMB members can review non-blind clinical data and participate in closed-door discussions on non-blind data. Discussions on clinical trial data and DSMB are confidential.
DSMB chairman duties
- Voting.
- Organizing meetings, assisting with the planning agenda, and ensuring that documents such as meeting minutes and recommendations are properly filed.
- Summarizing and promoting discussion, and making a casting vote when there is disagreement.
- Acting as the main contact for DSMB.
- Reviewing and approving DSMB regulations.
- Ensuring that the DSMB voting process excludes research-related managers.
- Discussing DSMB suggestions with sponsors and project team members.
The sponsor’s responsibility
The following are the responsibilities of the sponsor:
- Choosing and approving the DSMB chairman and members.
- Reviewing and approving DSMB regulations.
- Reviewing and implementing DSMB recommendations (if appropriate).
- The sponsor’s staff, such as project leaders, researchers and other relevant staff, can attend public meetings. All sponsor participants are only attend as observers, and project leaders can comment on project content and government regulatory issues.
- Communicating DSMB recommendations to researchers or relevant personnel, and notifying regulatory authorities and other agencies as necessary.
- Reviewing information about conflicts of interest and having the authority to take action on conflicts of interest identified.
- Consulting and arranging for a DSMB conference call (or sponsorship).
- Sending relevant information to DSMB members (or the sponsor).
- Writing a summary of the DSMB public meeting (or the sponsor's appointment).
- Sending the minutes of the public meeting to DSMB members (or the sponsor).
- Providing data and reports to DSMB one week before the scheduled meeting (non-blind reports are sent directly by the non-blind statistician to the DSMB chairman to ensure that confidential data is not disclosed to any of the sponsors).
- Timely coordination of reports providing DSMB temporary application requirements.
- Paying for DSMB members’ accommodation and travel expenses, and the conference fee is recorded in
. - Sponsors must not participate in closed meetings or discuss data with non-blind members.
Test statistician responsibility
Participation in DSMB’s open and closed meetings, participating in the discussion, but without voting rights, he/she is in addition to DSMB members. As the only person who can access the uncovered data, they must also sign a confidentiality agreement.
Independence of DSMB
DSMB members are not affected by other factors and always need to prioritize the safety of the maintenance subject and the integrity of the research. Anyone who has economic and intellectual property rights or other interests with the study drug, device, or procedure is not able to become a DSMB member or participate in the evaluation of the project. Independence is the most important aspect in ensuring that DSMB members are objective and can make a fair assessment of the research security and data validity. The following measures ensure the independence of DSMB:
DSMB members are not supervised by any of the researchers currently on the project being monitored, and the sponsor and researcher cannot be the DSMB members for the project under study.
There is no direct relationship of interest between the DSMB members and the test results, and there are no economic or intellectual property interests in the research results of the monitored projects.
Members of DSMB must disclose their economic interests and advisory relationships (directly or indirectly) with pharmaceutical companies, biotechnology companies, and contract research organizations.
DSMB members are required to sign a confidentiality agreement, which includes interventions, programs, details of the meeting's deliberations, implementation status, information about the study subjects, and related matters.
Program design team members can participate in the DSMB audit program public meetings, but can not participate in the closed meetings of the audit program.
The sponsor is responsible for determining whether the public interest or advisory relationship of the DSMB members has a significant impact on the objectivity of their judgment. If the DSMB member has any interest or advisory relationship with the pharmaceutical company, biotechnology company, or contract research organization, it should be brought to the attention of DSMB, the chairman, and the sponsor report.
DSMB meeting minutes should document potential conflicts of interest and discussion results (e.g., cancelling member voting rights and avoiding discussions). Members of the safety oversight committee with potential or significant conflicts of interest in monitoring projects must resign from DSMB. At the beginning of each DSMB meeting, potential changes in DSMB members’ interests must be checked.
DSMB meeting
Start of the meeting
Before the start of the study, the first start meeting of DSMB was held. This meeting formally established DSMB and introduced the project plan for monitoring. The revised DSMB charter was finalized, and the communication plan was discussed between the DSMB members, project team, and sponsor. Participants included DSMB members and sponsor representatives. At the beginning of the DSMB meeting, the chairman announced the formal establishment of DSMB for this study. The topics of the meeting were as follows:
- Introducing DSMB members.
- Reviewing DSMB regulations.
- Defining the role and responsibility of DSMB.
- The basic rules of DSMB, including how to carry out work (voting rules, quorum requirements, and the attendance system, etc.).
- Briefly discussing the plan and the form and format of the interim report submitted to DSMB.
- Discussing and completing the data and safety monitoring program.
Meeting schedule and form
The DSMB meeting frequency is designed to be 1% and 90% of the study progress. After that, the actual rate of the experiment and the incidence of the event can be adjusted.
The DSMB meeting consists of a closed meeting and public meeting. In an emergency, web conferencing can be considered, but the confidentiality of the meeting must be guaranteed.
DSMB meeting quorum requirement: when the number of participants is less than three, the DSMB meeting cannot be held unless the DSMB chairman and the sponsor reach a consensus in advance: it must be agreed to absently review the meeting materials and give written comments to the chairman. In some cases, members will be asked to submit separate electronic or paper review comments.
If a member misses a meeting, the DSMB chairman needs to confirm with him/her whether he/she can attend the follow-up meeting: if the member misses the second meeting, the chairman needs to contact the absentee to ascertain that he/she is able to continue as a DSMB member; if the member is absent from a meeting for a third time, they will forfeit their membership of DSMB, and a new DSMB member will be appointed by the sponsor.
Public meeting
First, an introduction to the conference: meeting topics, naming (ensuring that the DSMB members reach the legal attendance), a reminder of the confidentiality of the relevant procedures and corresponding documents, and reviewing the conflicts of interest of all DSMB members.
After the introduction, DSMB enters the official part of the public meeting. Participants include DSMB members, main researchers and other relevant researchers, and sponsor representatives. If necessary, representatives of the drug administration department and the clinical trial steering committee may also be invited.
At public meetings, the information in the public report is discussed so that DSMB members are aware of the state of the research. The main investigators report on the status of the research and related findings and other specific security considerations or concerns. The public meeting also provides a platform for information exchange between the various groups of the research team. DSMB members can ask questions of relevant research team members to obtain more information related to data monitoring. Discussions may include research progress, recruitment status, baseline characteristics, violations, adverse events, center conditions, quality control, timeliness, and completeness of follow-up, etc. Only blind data is reviewed and/or discussed at public meetings.
Closed meeting
After the public meeting, only DSMB members and analysts who submit the interim analysis report will participate in closed sessions to monitor non-blind and/or grouped safety and efficacy data, discuss the results, and develop and vote for research recommendations. Participating non-blind statisticians provide guidance and answer statistical questions. After the closed meeting, the interim analysis report is retrieved by the DSMB secretary and stored in a confidential filing cabinet.
After the closed meeting, the DSMB chairman summarizes the proposal submitted to the sponsor to discuss the proposal of DSMB. The chairman of DSMB must summarize the meeting within the 7 working days following, focusing on the various problems found and the safety assessment. DSMB voting decision proposal documents are forwarded to the sponsor representative.
Unplanned meetings/reports
If the study encounters security issues or new information outside of the research, DSMB must increase the number of meetings to ensure the safety of the trial. Any monitoring research member can make a submission to the DSMB chairman, principal investigator or sponsor to request an unscheduled DSMB meeting. The chairman of DSMB cooperates with the sponsor to arrange an unscheduled meeting. DSMB can request the data report from the sponsor as needed. The sponsor informs the test statistician.
Communication and communication
Send DSMB report
In the event of a serious adverse event which may be relevant or related to the research intervention by the investigator, the sponsor shall report to the DSMB chairperson by telephone or fax within 7 calendar days The formal written report shall be submitted within 15 natural days. The serious adverse event report is submitted to the DSMB chairman after the quarterly summary.
Relevant analysis reports include but are not limited to the following: serious adverse events, adverse events, violations or deviations from the program list, research progress reports, shedding subjects list, and/or interim analysis reports (divided into blind public meeting reports and non-blind closures) Door Conference Report). Blind reports are sent to DSMB members 7 working days before each meeting or when requested by DSMB. The non-blind report is printed by the test statistician to the meeting site.
DSMB meeting minutes
In order to compile the minutes of the meeting, the meeting can be recorded. Once the chairman approves the minutes of the meeting, the audio recording is destroyed. The sponsor or its records the minutes of the public meeting. The draft meeting minutes are then issued, and the participants review and submit comments and forward them to the DSMB chairman and the sponsor for review within <7 working days after the meeting.
Closed meeting minutes to record the process of closed meetings. The DSMB executive secretary is responsible for the record. If the discussion regarding non-blind data features in a closed meeting, the meeting minutes including non-blind information will be marked as "confidential" and only sent to DSMB members and statisticians. At the end of the study, the DSMB executive secretary sends a complete set of public and closed meetings to the sponsor.
DSMB recommendations
Following a closed meeting, a brief public meeting between the DSMB members and the sponsor’s representative will be held to discuss the DSMB recommendations. DSMB’s chairman approves the DSMB proposal and forwards it to the sponsor within 7 working days after meeting. The proposal should list the opinions of the minority who voted against the veto. The sponsor reviews the proposal and discusses all recommendations in consultation with the principal investigator. All modifications should be retained
Amendment charter
The closing meeting will be discussed and revised by the sponsor to submit the draft of the DSMB charter. The revised charter will be effective upon approval by the chairman and the sponsor. If necessary, the DSMB charter can be revised after being brought into force. The revised charter will be updated and approved again. The version update content, reason and date will be recorded. The revision needs to retain each modification trace.
Save document
The following documents (including but not limited to) need to be archived: a charter, a member's resume, a signed statement (showing he/she understands his or her responsibilities, as a DSMB member, there is no conflicting with the performance of his or her duties), all income and expenditure records (including compensation and compensation for DSMB members), meeting agenda, meeting minutes, and copies of all materials received by DSMB (including sponsor’s report, copy of DSMB's proposal submitted to sponsor, copy of all official DSMB letters). All files are kept by the DSMB executive secretary in a locked file cabinet in restricted security zones.
Confidentiality
Data submitted for review by the Safety Oversight Committee should be kept blind in the trial group unless the committee considers the characteristics of each group to be necessary for their decision.
Blind data submitted to DSMB should be provided with a set of coded decryption codes for uncovering at any time.
DSMB’s private meetings must remain confidential.
Every member of DSMB must sign a confidentiality statement and strictly maintain confidentiality of all research-related information provided only to them.
Composition
Membership and size of the DSMB
Membership is national and includes previous expertise in trials of investigational medicinal products, the clinical setting of critical care medicine and previous DSMB membership.
DSMB’s Chairman: Chun Wang, MD, PhD.
Professional emphasis: Clinical Doctor
DSMB’s members:
1. Chunquan Ou,
Professional emphasis: Statistics
2. Xiaoqi Liu,
Professional emphasis: clinical pharmacy
Acknowledgments
Many thanks for useful suggestions given by Prof. Pingyan Chen from Department of statistics, Southern Medical University and Mr. Qiang Li, MS, from George Institute for Global Health.
Funding: National Science Foundation of China (Grant No. 8197021596), Beijing Lisheng Cardiovascular Health Foundation (Grant No. LHJJ20141751), Guangdong Provincial People’s Hospital Foundation (Grant No. 2014dzx02, Grant No. 2017B030314041).
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/atm.2020.03.192). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was approved by the ethics committee of our institution (No. 2014dzx02), and all patients have given written informed consent.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Narula A, Mehran R, Weisz G, et al. Contrast-induced acute kidney injury after primary percutaneous coronary intervention: results from the HORIZONS-AMI substudy. Eur Heart J 2014;35:1533-40. [Crossref] [PubMed]
- Mehran R, Dangas GD, Weisbord SD. Contrast-Associated Acute Kidney Injury. N Engl J Med 2019;380:2146-55. [Crossref] [PubMed]
- Liu Y, Hong D, Wang AY, et al. Effects of intravenous hydration on risk of contrast induced nephropathy and in-hospital mortality in STEMI patients undergoing primary percutaneous coronary intervention: a systematic review and meta-analysis of randomized controlled trials. BMC Cardiovasc Disord 2019;19:87. [Crossref] [PubMed]
- Liu Y, Chen JY, Huo Y, et al. Aggressive hydraTion in patients with ST-Elevation Myocardial infarction undergoing Primary percutaneous coronary intervention to prevenT contrast-induced nephropathy (ATTEMPT): Study design and protocol for the randomized, controlled trial, the ATTEMPT, RESCIND 1 (First study for REduction of contraSt-induCed nephropathy followINg carDiac catheterization) trial. Am Heart J 2016;172:88-95. [Crossref] [PubMed]
- Tan N, Liu Y, Chen JY, et al. Use of the contrast volume or grams of iodine-to-creatinine clearance ratio to predict mortality after percutaneous coronary intervention. Am Heart J 2013;165:600-8. [Crossref] [PubMed]
- Moher D, Schulz KF, Altman D. The CONSORT statement: revised recommendations for improving the quality of reports of parallel-group randomized trials. JAMA 2001;285:1987-91. [Crossref] [PubMed]
- Kahan BC, Morris TP. Improper analysis of trials randomised using stratified blocks or minimisation. Stat Med 2012;31:328-40. [Crossref] [PubMed]
- Moher D, Hopewell S, Schulz KF, et al. CONSORT 2010 explanation and elaboration: updated guidelines for reporting parallel group randomised trials. BMJ 2010;340:c869. [Crossref] [PubMed]
- Briguori C, Visconti G, Rivera NV, et al. Cystatin C and contrast-induced acute kidney injury. Circulation 2010;121:2117-22. [Crossref] [PubMed]
- Maioli M, Toso A, Leoncini M, et al. Persistent renal damage after contrast-induced acute kidney injury: incidence, evolution, risk factors, and prognosis. Circulation 2012;125:3099-107. [Crossref] [PubMed]
- Ponikowski P, Voors AA, Anker SD, et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC)Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J 2016;37:2129-200. [Crossref] [PubMed]




