
Transesophageal echocardiography instead or in addition to transthoracic echocardiography in evaluating haemodynamic problems in intubated critically ill patients
Introduction
Patients with hemodynamic instability are universally observed in the intensive care unit (ICU). Over one-third of critically ill patients experience hypotension or shock (1), and the ratio can be as high as one-half in patients with organ dysfunction (2). However, only one-third of patients live through these serious attacks (3). Furthermore, common examinations used in the clinic do not provide sufficient information in life-threatening situations. Therefore, it is imperative to find a way to obtain valuable information immediately at the patient’s bedside. Echocardiography is a useful procedure that simultaneously yields morphologic and hemodynamic information (4).
Transthoracic echocardiography (TTE) has proven to be of great value in the critical care setting because of its portability, widespread availability, and instantaneous diagnostic capability (5,6). However, TTE requires a good acoustic “window” to allow accurate analysis. Unfortunately, numerous restrictions on the imaging ability of TTE are commonly present in critically ill surgical patients. TTE has a high failure rate in those who are supported with positive end-expiratory pressure (PEEP) and in those with surgical incisions (7). Less hampered by these limitations, transesophageal echocardiography (TEE) overcomes these problems and yields better quality images because the position of the probe is closer to the posterior aspect of the heart (8,9). Early research has demonstrated the feasibility of TEE, as comfort and facility with TTE has been steadily actualized across a large number of providers (10-12), and there is now renewed and expanding interest in TEE at many centers. A recent study (13) from the U.S. performed a descriptive observation in a medical ICU and found that TEE could confirm the original diagnosis in more than 70% of studies and identify novel findings in approximately 30% of studies that led to changes in clinical decisions. However, most of these studies were performed in medical or general ICUs and TEE was usually not the preferred monitoring tool, especially when TTE appeared to have addressed the clinical problems. As a result, it remains largely unknown whether TEE is a clinically valuable replacement or supplement for TTE as a primary tool in evaluating haemodynamic problems in critically ill surgical patients.
We designed this study to prospectively assess the diagnostic and therapeutic value of TEE instead or in addition to TTE in critically ill surgical patients by analyzing the major clinical conditions in the surgical ICU, namely, hemodynamic instability and mechanical ventilation.
Methods
Patients
This prospective observational study included consecutive intubated patients receiving mechanical ventilation with hemodynamic instability in a surgical ICU at a tertiary teaching hospital (Guangzhou, China) from December 2016 to February 2018. Hemodynamic instability was defined as sustained hypotension requiring vasopressors to maintain systolic arterial pressure >90 mmHg or mean arterial pressure >65 mmHg (14). The exclusion criteria included unrepaired tracheoesophageal fistula, history of prior esophageal surgery, esophageal obstruction or stricture, esophageal varix or diverticulum, gastric or esophageal bleeding, oropharyngeal pathology, and severe coagulopathy. The Medical Ethics Committee of the First Affiliated Hospital of Sun Yat-sen University approved the protocol (No. 2015-120). The study was registered at the Chinese Clinical Trial Registry (ChiCTR1900022172). All patients or their next of kin signed consent forms to participate in this study.
Echocardiography protocol
Echocardiographic examinations were performed using commercially available ultrasound scanners (M-Turbo, SonoSite). A standard 2.5-MHz ultrasound transducer was used for the transthoracic studies, and a multiplane 5-MHz transesophageal probe was used for the transesophageal examinations. Both TTE and TEE were performed. Unless the patients were previously sedated, midazolam or propofol was administered intravenously before introduction of the TEE probe. A transesophageal probe was introduced “blindly” by simply directing the tip into the posterior part of the pharynx, maintaining a midline position and gently allowing the transducer to flex passively. We never had to deflate the cuff of the endotracheal tube or introduce the transducer under direct vision by direct laryngoscopy. The nasogastric/orogastric tube was removed if it appeared to degrade the TEE image. No antimicrobial prophylaxis was administered. Throughout the examination, electrocardiography (ECG), blood pressure, heart rate, and oxygen saturation were monitored.
All enrolled patients underwent successively TTE and TEE examinations. Images and video loops from both examinations were stored and disclosed to two different primary physicians of critical care. TTE was performed with five major views described previously (15,16), including parasternal long-axis and short-axis views, apical four-chamber views, subcostal four-chamber view and subcostal inferior vena cava view. The physicians were asked to independently provide an initial diagnosis and therapy based on the TTE information, and a consensus had to be reached between the two physicians if there was disagreement. In addition to TTE, TEE was also performed with the intent of obtaining a set of twenty views according to the recommendations of a consensus statement by the American Society of Echocardiography (ASE) and the Society of Cardiovascular Anesthesiologists (SCA), including mid esophageal four(two) chamber/mitral commissural/long axis/right ventricle inflow-outflow/aortic valve long(short) axis/ bicaval/ascending aortic long(short) axis/descending aorta long(short) axis, transgastric basal(mid) short axis/two-chamber/long axis/right ventricle inflow, upper esophageal aortic arch long(short) axis, and deep transgastric long axis (17). The two physicians then independently re-evaluated the diagnosis and therapy in light of the TEE findings. Whether TEE changed the course of the current diagnosis or therapy compared with TTE was noted. This finding was further classified into four categories: class 1, TEE confirmed the initial TTE diagnosis and therapy; class 2, TEE revealed a new diagnosis but did not result in a change in therapy compared with TTE; class 3, TEE revealed a new diagnosis requiring a change in therapy; class 4, TEE determined the diagnosis and therapeutic decisions because TTE failed. A consensus had to be reached between the two physicians for TEE to be accepted as altering the diagnosis and therapy; otherwise, this finding was rejected. This finding was rejected if no explanation was provided or no consensus reached.
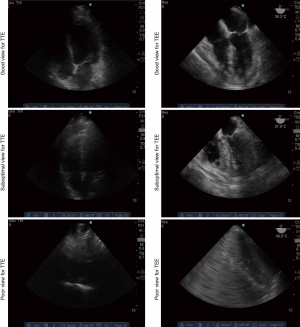
The image quality of TEE images was compared with that of TTE images. When the protocol was completed, the quality of stored images and video loops were evaluated by two different cardiac ultrasound experts. The image quality was classified as a good (score 2), suboptimal (score 1) or poor view (score 0) (Figure S1). According to the scores of TTE images, the patients were divided into two groups: patients with adequate TTE views (score ≥6) and inadequate TTE views (score <6).
Statistical analysis
Descriptive statistics were utilized to analyze demographic, clinical, and outcome parameters. Continuous data are presented as the means and standard deviations (SDs) or medians and interquartile (1st–3rd quartile) ranges. Categorical data are summarized as a total number and percentage of the cohort. All continuous variables were compared using Student’s t-test or the Wilcoxon signed-rank test in the absence of a normal distribution. Categorical variables were compared using the chi-squared test. A P value <0.05 was considered statistically significant with 95% confidence intervals (CIs) also reported. These statistical analyses were performed using SPSS 19.0 software (SPSS, Chicago, IL, USA).
Results
Patient characteristics
During the study period, 70 patients were screened and 2 patients were excluded because of incomplete TEE intubation. A total of 68 intubated patients who were hemodynamically unstable were included in the study. The demographic and clinical characteristics of these patients are shown in Table 1. All patients received intubation and vasoactive agents. The mean age was 59.7±16.7 years, and 52.9% were male. The mean acute physiology and chronic health evaluation (APACHE) II score was 17.1±8.4 and ranged from 5 to 45. The median norepinephrine dose was 0.3 (0.15 to 0.60) µg/kg/min, with a median lactate level of 3.1 (2.0 to 5.8) mmol/L. More than half (51.4%) of the patients suffered from sepsis and the ICU mortality was 22.1%.
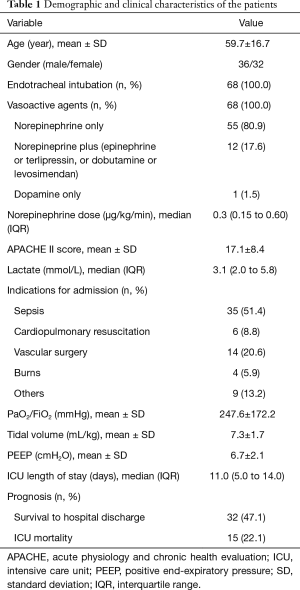
Full table
Examination feasibility, safety and quality
All patients underwent TTE and TEE examination successively. There was no significant difference in the vital signs for patients when performing TTE and TEE (Table S1). However, eight patients failed to have effective TTE examination because an acoustic window was not available and/or was unrecognized. TTE could not be performed in 4 patients with severe burns and 1 patient in a prone position; 3 other patients did not have adequate visualization because of surgical dressings, tape, or tubing, air distribution due to mechanical ventilation and/or subcutaneous emphysema, and/or obesity or chronic obstructive pulmonary disease (COPD). During the implementation of TEE, no severe complications occurred. Only two patients experienced dysrhythmias temporally at TEE intubation and resolved spontaneously without any treatment.

Full table
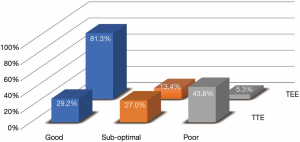
A total of 315 views from TTE and 1,360 views from TEE were stored. Among the TTE procedures, imaging quality was good in 92 views (29.2%), suboptimal in 85 views (27.0%), and poor in 138 views (43.8%). However, among TEE procedures, imaging quality was good in 1,105 views (81.3%), suboptimal in 182 views (13.4%), and poor in 73 views (5.4%). TEE yielded significantly higher-quality images with more good views and fewer poor views than TTE (P=0.000) (Figure 1).
Assessment of diagnostic and therapeutic value
Compared to TTE findings, the additional TEE examination provided no more information about the initial diagnosis and therapy (class 1) in 26 patients (38.2%).
Of the remaining 42 patients (61.8%), TEE instead of or in addition to TTE revealed new findings or led to significant changes in therapy, as TTE supplied inadequate information. TEE used in addition to TTE led to a new diagnosis without therapeutic implications (class 2) in 11 patients (16.2%) and made a major clinical contribution leading to a therapeutic change (class 3) in 23 patients (33.8%). Moreover, TEE used instead of TTE determined the diagnosis and therapy in 8 patients (11.8%) whose haemodynamic problems could not be addressed by TTE (class 4). In total, TEE had critical therapeutic benefits (class 3 and 4) that was not provided by TTE in 31 patients (45.6%) (Table 2).

Full table
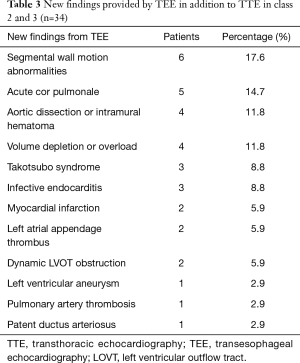
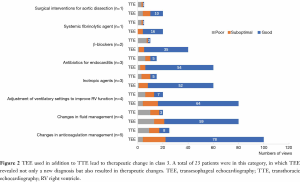
In 34 patients (class 2 and 3), TEE in addition to TTE revealed new findings. The main new findings from TEE indicated problems of the respiratory system (n=5) and circulatory system, involving cardiac motion or dynamic abnormalities (n=13), main artery disease (n=6), improper volume (n=4) and valvular disease (n=3). A detailed summary of the additional TEE findings is presented in Table 3. In 23 patients (class 3), TEE revealed not only a new diagnosis but also resulted in therapeutic changes (Figure 2). Five patients received anticoagulant therapy because of myocardial infarction (n=2), left atrial appendage thrombus (n=2) (Video 1) and left ventricular aneurysm (n=1) (Video 2). Four patients had altered fluid treatment regimens because of improper volume evaluation, 3 patients had therapy with inotropic agents initiated because of left ventricular dysfunction (Video 3), and 2 patients received β-blockers because of dynamic left ventricular outflow tract (LVOT) obstruction (Video 4). Four patients underwent adjustments in PEEP to improve right ventricular (RV) function because of acute cor pulmonale (ACP) (Video 5). Three patients received a new antibiotic regimen because of the vegetation of the mitral valve in 2 patients (Video 6) and a large vegetation on the tricuspid valve in 1 patient (Video 7). One patient had intravenous thrombolysis initiated because a thrombus was detected in the right pulmonary artery (Video 8). One patient received surgical intervention because type A dissection of the aorta was detected (Video 9).
Full table
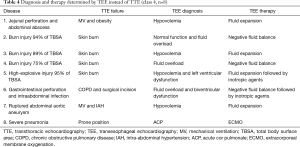
In 8 of 68 patients (class 4), TEE instead of TTE determined the diagnosis and therapy. The reasons for TTE examination failure were severe burn injuries (n=4), dynamic pulmonary hyperinflation or obesity (n=3) and a prone position in one patient (Table 4). However, TEE determined diagnosis in these patients and led to valuable treatments, including fluid expansion/reduction, inotropic agent administration (n=7) and further interventions, such as extracorporeal membrane oxygenation (ECMO, n=1).
Full table
Comparison of patients with adequate TTE views and inadequate TTE views
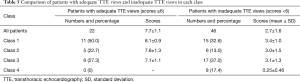
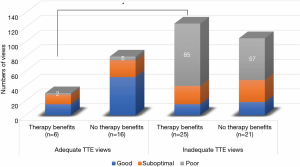
Of the 68 patients, 22 had adequate TTE views with scores 7.7±1.1, which was significantly higher than the remaining 46 patients, with a TTE score of only 2.7±1.6 (P=0.000). The scores in adequate TTE views group was significantly higher than that in inadequate TTE views group for all classes, with the exception of class 4 enrolling no patient in adequate TTE group. Owing to the clearer images in adequate TTE views group, there were more patients in class 1 (50.0% vs. 32.6%) and fewer patients in class 3 (27.3% vs. 37.0%), but no significant difference was observed (Table 5). Nevertheless, when considering the benefits of treatment, a high proportion (54.3%) of patients with inadequate TTE views could benefit from additional TEE examination, and even in patients with adequate TTE images, more than a quarter (27.3%) of patients could benefit from TEE. In other words, TEE had a significantly higher proportion of therapeutic benefits to patients with inadequate TTE views than those with adequate TTE views (54.3% vs. 27.3%, P=0.036) (Figure 3). Furthermore, the mortality in inadequate TTE views group was slightly lower than that in adequate TTE views group [19.6% (9/46) vs. 27.3% (6/22)], however, the difference is not statistically significant (P=0.473).
Full table
Discussion
Our study shows that TEE instead or in addition to TTE is useful for critical ill surgical patients with hemodynamic instability, especially for the patients with inadequate TTE views. First, more than half (61.7%) of hemodynamically unstable surgical patients could obtain additional diagnostic information from TEE examinations. Second, nearly half of patients (45.6%) received critical therapeutic benefits due to TEE findings that were not obtained by TTE. Third, patients with inadequate TTE views could benefit more from additional TEE examination, demonstrated by the significantly higher proportion of therapeutic benefits comparing with the patients with adequate TTE views.
Ultrasound image quality is the basis for an accurate clinical diagnosis. Image acquisition via a transthoracic approach can be challenging in critically ill patients, especially those who are mechanically ventilated and in the postoperative state. Hyperinflated lungs and surgical incisions or dressings can seriously affect the image quality of TTE. Our results indicate that imaging quality was good in 29.2% of views during TTE, which is consistent with the results of a study performed by Vignon et al. (10) who showed that only 24% of patients on mechanical ventilation could have good TTE images obtained. In contrast, image acquisition via the transesophageal approach is almost universally associated with easily obtained high-quality images. Vignon et al. reported that 72% of patients could have good TEE images obtained; in our study, imaging quality was good in 81.3% of views. The most common views with poor images were the main pulmonary artery and the aortic arch views. In general, significantly more high-quality images were obtained with TEE (P=0.000), which was essential to provide more important findings.
In our study, TEE instead or in addition to TTE provided an important diagnostic contribution in hemodynamically unstable patients on mechanical ventilation. Our results highlighted that TEE can reveal new findings regarding hemodynamics and cardiac structure. More than half of these findings were related to hemodynamic changes, including segmental wall motion abnormalities (17.6%), ACP (14.7%), Takotsubo syndrome (8.8%), myocardial infarction (5.9%) and volume evaluation (11.8%). Less cases of ACP were identified in our study than in the study performed by Garcia et al. (13), who reported a proportion of ACP as high as 27%. This finding may be because our research was carried out in a surgical ICU, and the study performed by Garcia et al. was carried out in a medical ICU where more patients had chronic cor pulmonale. Additionally, structural findings, such as endocarditis, a cardiac source of embolism, shunt, thoracic aorta, or valvular assessment were observed in more than one-third of examinations.
The use of TEE instead of or in addition to TTE not only provided new diagnostic information but also influenced major decisions. Garcia et al. (13) found that over 70% of TEE examinations confirmed the initial diagnosis, and the findings from TEE resulted in a change in clinical management in 38% of patients. Other studies have indicated that clinical management changes due to the information provided by TEE in the ICU occurred in 20% (12) and 32% of patients (18). In our study, only 38.2% of patients had the initial diagnosis confirmed, and 61.7% of patients received a new diagnosis from the additional TEE. More importantly, our data highlighted a high proportion of therapeutic impact from TEE findings. Specifically, 45.6% of patients (n=31) benefited from the additional TEE. The most common therapeutic changes were fluid management and the use of vasoactive agents (n=16). This finding might be because our study focused on hemodynamically unstable patients who received vasopressors. Furthermore, for these 31 patients who benefited, the majority of patients had inadequate TTE images (n=25). More than half (54.3%) of the patients with inadequate TTE views could benefited from additional TEE examination, which was significantly higher than the proportion of patients with adequate TTE. This finding emphasizes the potential utility of TEE for patients with inadequate TTE views, indicating that TEE as a primary clinical tool is essential in these patients. Particularly in patients with major burns and inflated lungs due to mechanical ventilation or COPD, TTE was failed to answer relevant clinical questions; TEE instead could provide valuable information for diagnosis, which may bring significant therapeutic benefits. It is worth noting that even among patients with adequate TTE images, more than a quarter (27.3%) of patients could benefit from TEE examination, which means TEE is still of value in patients with adequate TTE views.
Echocardiography is an important technique mastered by echocardiologists, however, ICU patients suffer from diseases that are different from traditional heart diseases. Pathophysiological and hemodynamic changes require the development of critical care ultrasound. ICU physicians have a better understanding of the patient’s condition and pathophysiological changes than ultrasound physicians (19). Ultrasound examinations performed by ICU physicians are more targeted and relevant to the disease. Lau et al. showed that TEE performed by experienced intensivists has high accuracy compared with the gold standard of cardiologist-performed TEE (20). Therefore, surgical intensivists can master TEE after enough training, allowing additional patients to benefit from diagnosis and treatment.
The present study has several limitations. First, the overall sample size was small, and this study was performed at a single tertiary care hospital; thus, the results may not be transferable to another clinical environment. Furthermore, although we demonstrated the diagnosis and treatment benefits from the application of TEE instead or in addition to TTE, we did not observe the impact of TEE on mortality; thus, additional large-scale studies must be conducted to evaluate how TEE affects mortality. Finally, we performed twenty TEE views in addition to five TTE views, and the larger number of TEE views may explain the findings. However, this set of twenty views is comprehensive and frequently provides information beyond the concerns of the resuscitative physician. Experts (21) have proposed that the initial mastery of the four views for goal-directed TEE allows the operator to address the most commonly posed questions. Thus, no relevant conclusion can be drawn regarding whether patients can benefit from goal-directed TEE.
Conclusions
The present study showed that TEE as a feasible clinical tool is useful for critically ill surgical patients with hemodynamic instability, especially for the patients with inadequate TTE views. TEE instead or in addition to TTE could provide valuable information for diagnosis, which may bring significant therapeutic benefits.
Acknowledgments
We would like to thank all of the doctors, nurses and patients involved for their dedication to the study. We also thank Yanqiu Liu and Wei Li, from Department of Medical Ultrasonic, for their kind help with the evaluation of the quality of stored images and video loops.
Funding: This work was funded by grants from the Wu Jieping Medical Foundation (grant no. 320.6750.18037, grant no. 320.6750.18068).
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Glenn Hernández and Guo-Wei Tu) for the series “Hemodynamic monitoring in critically ill patients” published in Annals of Translational Medicine. The article was sent for external peer review organized by the Guest Editors and the editorial office.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/atm.2020.04.09). The series “Hemodynamic monitoring in critically ill patients” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013) and approved by Medical Ethics Committee of the First Affiliated Hospital of Sun Yat-sen University (No. 2015-120). The study was registered at the Chinese Clinical Trial Registry (ChiCTR1900022172). All patients or their families signed consent forms to participate in this study.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Vincent JL, De Backer D. Circulatory shock. N Engl J Med 2014;370:583. [PubMed]
- Bitker L, Bayle F, Yonis H, et al. Prevalence and risk factors of hypotension associated with preload-dependence during intermittent hemodialysis in critically ill patients. Crit Care 2016;20:44. [Crossref] [PubMed]
- Andrews B, Semler MW, Muchemwa L, et al. Effect of an Early Resuscitation Protocol on In-hospital Mortality Among Adults With Sepsis and Hypotension: A Randomized Clinical Trial. JAMA 2017;318:1233-40. [Crossref] [PubMed]
- Strumwasser A, Frankel H, Murthi S, et al. Hemodynamic monitoring of the injured patient: From central venous pressure to focused echocardiography. J Trauma Acute Care Surg 2016;80:499-510. [Crossref] [PubMed]
- Oren-Grinberg A, Talmor D, Brown SM. Focused critical care echocardiography. Crit Care Med 2013;41:2618-26. [Crossref] [PubMed]
- Ferrada P, Murthi S, Anand RJ, et al. Transthoracic focused rapid echocardiographic examination: real-time evaluation of fluid status in critically ill trauma patients. J Trauma 2011;70:56-62. [Crossref] [PubMed]
- Cook CH, Praba AC, Beery PR, et al. Transthoracic echocardiography is not cost-effective in critically ill surgical patients. J Trauma 2002;52:280-4. [Crossref] [PubMed]
- Mayo PH, Narasimhan M, Koenig S. Critical Care Transesophageal Echocardiography. Chest 2015;148:1323-32. [Crossref] [PubMed]
- Jaidka A, Hobbs H, Koenig S, et al. Better With Ultrasound: Transesophageal Echocardiography. Chest 2019;155:194-201. [Crossref] [PubMed]
- Vignon P, Mentec H, Terre S, et al. Diagnostic accuracy and therapeutic impact of transthoracic and transesophageal echocardiography in mechanically ventilated patients in the ICU. Chest 1994;106:1829-34. [Crossref] [PubMed]
- Poelaert JI, Trouerbach J, De Buyzere M, et al. Evaluation of transesophageal echocardiography as a diagnostic and therapeutic aid in a critical care setting. Chest 1995;107:774-9. [Crossref] [PubMed]
- Slama MA, Novara A, Van de Putte P, et al. Diagnostic and therapeutic implications of transesophageal echocardiography in medical ICU patients with unexplained shock, hypoxemia, or suspected endocarditis. Intensive Care Med 1996;22:916-22. [Crossref] [PubMed]
- Garcia YA, Quintero L, Singh K, et al. Feasibility, Safety, and Utility of Advanced Critical Care Transesophageal Echocardiography Performed by Pulmonary/Critical Care Fellows in a Medical ICU. Chest 2017;152:736-41. [Crossref] [PubMed]
- Michard F, Boussat S, Chemla D, et al. Relation between respiratory changes in arterial pulse pressure and fluid responsiveness in septic patients with acute circulatory failure. Am J Respir Crit Care Med 2000;162:134-8. [Crossref] [PubMed]
- Via G, Hussain A, Wells M, et al. International evidence-based recommendations for focused cardiac ultrasound. J Am Soc Echocardiogr 2014;27:683.e1-33. [Crossref] [PubMed]
- Levitov A, Frankel HL, Blaivas M, et al. Guidelines for the Appropriate Use of Bedside General and Cardiac Ultrasonography in the Evaluation of Critically Ill Patients-Part II: Cardiac Ultrasonography. Crit Care Med 2016;44:1206-27. [Crossref] [PubMed]
- Shanewise JS, Cheung AT, Aronson S, et al. ASE/SCA guidelines for performing a comprehensive intraoperative multiplane transesophageal echocardiography examination: recommendations of the American Society of Echocardiography Council for Intraoperative Echocardiography and the Society of Cardiovascular Anesthesiologists Task Force for Certification in Perioperative Transesophageal Echocardiography. Anesth Analg 1999;89:870-84. [Crossref] [PubMed]
- Liebson PR. Transesophageal echocardiography in critically ill patients: what is the intensivist's role? Crit Care Med 2002;30:1165-6. [Crossref] [PubMed]
- Alherbish A, Priestap F, Arntfield R. The introduction of basic critical care echocardiography reduces the use of diagnostic echocardiography in the intensive care unit. J Crit Care 2015;30:1419.e7-11. [Crossref] [PubMed]
- Lau V, Priestap F, Landry Y, et al. Diagnostic Accuracy of Critical Care Transesophageal Echocardiography vs Cardiology-Led Echocardiography in ICU Patients. Chest 2019;155:491-501. [Crossref] [PubMed]
- Arntfield R, Pace J, McLeod S, et al. Focused transesophageal echocardiography for emergency physicians-description and results from simulation training of a structured four-view examination. Crit Ultrasound J 2015;7:27. [Crossref] [PubMed]


