
Timing of frozen-thawed embryo transfers—does it really matter?
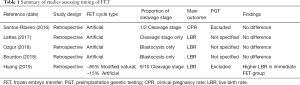
In a recent publication in Annals of Translational Medicine, Huang et al. investigated the timing of frozen-thawed embryo transfers after controlled ovarian stimulation (COS) (1). Specifically, the authors were interested in whether outcomes were improved when frozen embryo transfer (FET) occurred in the cycle immediately following COS versus delaying FET to subsequent cycles. In an era where freeze-all policies are becoming increasingly utilized, this question of optimal timing has arisen. This study by Huang et al. is relevant as it adds to the limited data available regarding timing of FET after COS (Table 1).
Full table
This study utilized a retrospective cohort design comparing patients who underwent FET within the first menstrual cycle after oocyte retrieval versus those patients that underwent FET after one or more additional menses. Patients with regular menses underwent a modified natural cycle, and those patients with irregular menses underwent artificially induced cycles. Due to significant differences in baseline characteristics between the two groups the authors opted to perform a one-to-one propensity score matching model. They identified key confounding variables and very elegantly adjusted the two groups for these variables in order to reduce potential selection bias.
The authors found that cycles with delayed FET had a significantly lower live birth rate (LBR) compared to those with immediate FET. These findings remained significant after application of the propensity score matching model. The authors’ definition of delayed FET cycle was approximately 90 days following an oocyte retrieval. This is in accordance with how previous studies defined delayed FET (2-5). We commend the authors’ use of LBR as their primary outcome. It has been advised that LBR should be the preferred outcome for reproductive medicine studies (6). The authors’ data is notable for differing from the previously cited literature which were not able to detect a significant difference between delayed versus immediate FET.
The vast majority of patients included in this study underwent modified natural cycles for endometrial preparation while the remainder underwent an artificial cycle. As evidenced by Table 1, previous studies reported only on artificial FET cycles. Considering that artificial cycles make up only approximately 15% of the cycles in the current study, it would be of interest to compare these two groups’ outcomes in the future. Given that there is no data on timing of FETs utilizing modified natural cycles, outcomes for that subgroup are essentially unknown. Separating the data based on which type of FET cycle patients underwent may help to ascertain if the difference detected between the two groups was driven primarily by the modified natural cycles. This would offer an explanation for the difference in outcomes in this study compared to previous studies.
It is noteworthy that most of the embryos that were transferred were at cleavage stage (~93%). Cleavage stage embryos yield lower implantation and live birth rates compared to blastocysts (7,8). Most IVF centers perform blastocyst stage embryo transfers predominantly or exclusively. On a parallel note, possibly in part due to the lower implantation rates of cleavage stage embryos, almost 90% of the transfers in this study were double embryo transfers (DET), a practice that has been abandoned by most contemporary IVF centers. The inclusion of cleavage stage embryos and DETs limits the wide clinical application of this data.
In addition, this study did not include any patients that underwent preimplantation genetic testing for aneuploidy (PGT-A). The reason for this is unknown. Without PGT-A it is difficult to ascertain whether aneuploidy significantly differed between the two groups.
In general, it is important for authors to convey to readers limitations of their studies. We commend the authors for declaring that this study was not sufficiently powered to detect a difference between the two groups. They were diligent to include the actual number of patients per arm that would have been required for an adequately powered study. The authors also indicated an uneven distribution between the two groups, with many more patients included in the delayed group. One possible reason for this is that patients with failed endometrial proliferation in the immediate cycle group were ultimately included in the delayed group. This presents a potential bias as patients with poor proliferation were more likely to be in the delayed group.
Overall, timing of FETs following COS is an important intervention to investigate. Most clinics that have adopted a non-elective freeze all program allow patients to undergo FET whenever is most convenient for them. Most practitioners would agree that as long as baseline laboratory and ultrasound criteria have been fulfilled it should make little difference whether the FET is performed in the immediate cycle versus a delayed cycle. This is partly because there is no hypothesized physiologic reason why performing a FET in the immediate cycle following COS would offer any benefit. Therefore, in the absence of a well-delineated mechanism and due to the contradicting results reported in Table 1, we would encourage more clinics to investigate their internal data to outline differences in outcomes based on timing prior to adopting new changes in their own clinics. Specifically, if their clinic practices with fundamental differences from this study clinic including preference for single embryo transfers, blastocyst embryo transfers, and use of PGT-A. Ultimately, a randomized controlled trial, preferably using single (euploid) blastocyst transfers, would offer the most reliable evidence regarding whether performing a FET in the cycle immediately following COS improves outcomes.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/atm.2020.03.223). ES reports grants and personal fees from Foundation for Embryonic Competence, outside the submitted work. AK has no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Huang J, Lu X, Xie Q, et al. Timing of frozen-thawed embryo transfer after controlled ovarian stimulation in a non-elective freeze-all policy. Ann Transl Med 2019;7:752. [Crossref] [PubMed]
- Santos-Ribeiro S, Polyzos NP, Lan VT, et al. The effect of an immediate frozen embryo transfer following a freeze-all protocol: a retrospective analysis from two centres. Hum Reprod 2016;31:2541-8. [Crossref] [PubMed]
- Lattes K, Checa MA, Vassena R, et al. There is no evidence that the time from egg retrieval to embryo transfer affects live birth rates in a freeze-all strategy. Hum Reprod 2017;32:368-74. [Crossref] [PubMed]
- Ozgur K, Bulut H, Berkkanoglu M, et al. Frozen embryo transfer can be performed in the cycle immediately following the freeze-all cycle. J Assist Reprod Genet 2018;35:135-42. [Crossref] [PubMed]
- Bourdon M, Santulli P, Maignien C, et al. The interval between oocyte retrieval and frozen-thawed blastocyst transfer does not affect the live birth rate and obstetrical outcomes. PLoS One 2018;13:e0206067. [Crossref] [PubMed]
- Barnhart KT. Live birth is the correct outcome for clinical trials evaluating therapy for the infertile couple. Fertil Steril 2014;101:1205-8. [Crossref] [PubMed]
- Kontopoulos G, Simopoulou M, Zervomanolakis I, et al. Cleavage Stage versus Blastocyst Stage Embryo Transfer in Oocyte Donation Cycles. Medicina (Kaunas) 2019. [Crossref] [PubMed]
- Glujovsky D, Farquhar C, Quinteiro Retamar AM, et al. Cleavage stage versus blastocyst stage embryo transfer in assisted reproductive technology. Cochrane Database Syst Rev 2016.CD002118. [PubMed]


