Angiomyolipoma of the adrenal gland: clinical experience and literature review
Introduction
Angiomyolipoma, a benign form of tumor of mesenchymal origin, is characterized by smooth muscle cells, thick-walled blood vessels, and adipose tissue. Angiomyolipoma is most commonly found in the kidney and in the extra-renal area in the liver. It is rarely reported that angiomyolipoma is found in the retroperitoneum, spleen, bone, lung, ovary and so on (1). Adrenal angiomyolipomas are extremely rare and usually asymptomatic. Patients with adrenal angiomyolipoma may present with nonspecific symptoms, such as abdominal pain. The detection of adrenal angiomyolipoma is usually incidental, arising from a physical examination or routine ultrasound (US) and computed tomography (CT) examination for another unrelated disease (2). Little is known about the disease, and in cases of primary malignancies with adrenal spread, such as lung cancer, distinguishing adrenal incidentalomas from metastasis presents a considerable diagnostic challenge (3,4). Herein, we describe the case of a patient with adrenal angiomyolipoma who had previously undergone lung cancer resection, with the aim of sharing the clinical experience and CT imaging distinctions between adrenal angiolipoma and tumor metastasis. Finally, we carried out a review of the relevant literature, and the information is summarized in Table 1. We present the following case in accordance with the CARE reporting checklist (available at http://dx.doi.org/10.21037/atm-20-3147).
Full table
Case presentation
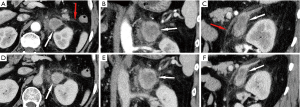
A 62-year-old man presented at our hospital with a small oval-bounded mass in the left adrenal gland. The mass was first discovered during a routine follow-up CT examination after the patient received lung cancer resection in 2016. During a two-year follow-up period, the mass increased from 1 to 3.5 cm (the maximum cross section) (Figures 1,2). Consequently, the patient was referred to our hospital for more complete evaluation and management.
The patient exhibited no symptoms, and a physical examination of the patient’s abdomen proved unremarkable. A history of lung cancer resection was recorded. The laboratory tests revealed that the patient’s epinephrine, 24-hour urinary catecholamine, aldosterone and plasma cortisol levels were all within the normal range.
On dual-phase enhanced CT scan, the mass displayed ring enhancement surrounded by unenhanced flocculent exudate (Figure 2). A diagnosis of adrenal metastases was made based on the CT imaging findings and the patient’s history of lung cancer.
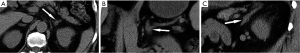
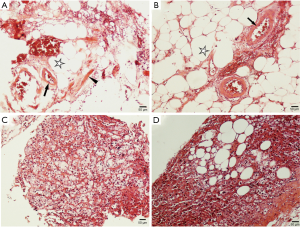
Subsequently, the patient underwent retroperitoneal laparoscopic partial resection of the left adrenal gland under general anesthesia. Postoperative pathology indicated left adrenal adipose tissue and hemangiomatous hyperplasia (Figure 3); thus, the diagnosis of adrenal angiomyolipoma was reached. After seven days, the patient recovered with no surgery-related complications and was discharged. At three months follow-up, the patient was alive and had experienced no recurrence after the operation.
Literature review
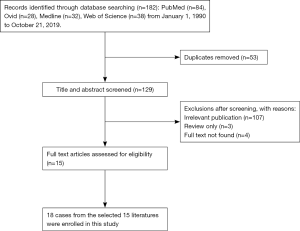
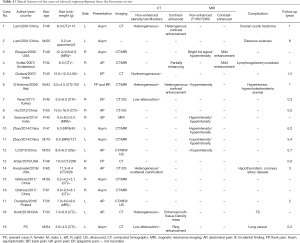
The PubMed, Medline, Web of Science, and Ovid databases were searched for English-language case reports and case series of adrenal angiomyolipoma published between January 1, 1990 and March 31, 2019. The following key words were used: (Adrenal Glands or Adrenal Gland or Gland Adrenal or Glands Adrenal) and (Angiomyolipoma or Angiomyolipomas). The flow chart of the literature screening process is set out in Figure S1. A total of 15 full-text articles involving 18 cases were included for analysis. For each case, the first author, publication year, and country were documented, along with the patient’s age, sex, size, weight, affected side, symptoms, imaging characteristics, complications, and follow-up results (Table 1).
According to the literature, angiomyolipomas are most commonly found in the kidneys and are rare in the adrenal gland. Prior to our case, only 18 cases of adrenal angiomyolipoma had been documented, among which none of the patients were reported to have a history of cancer.
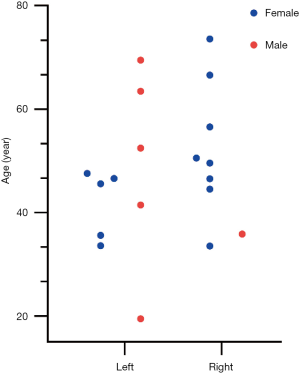
The 19 reported cases (including of our case) of adrenal angiomyolipoma comprise 13 women and 6 men, with a female to male ratio of 2.2 to 1. Remarkably, as shown in Figure S2, the age distribution of the female patients was mainly between 30 and 50 years old, and these patients predominantly suffered from abdominal back pain, with lesions mostly located on the right side. However, the ages of the male patients were more scattered and most of the lesions were located on the left side. All of the adrenal angiomyolipomas reported in the literature were nonfunctional (5), and ranged in size from 0.2 to 16 cm, with 95% of the masses exceeding 4 cm.
Discussion
In this case report, we reported a case of a 62-year-old man who developed an enlarged mass in the left adrenal gland after lung cancer resection. Due to the patient’s history of lung cancer, clinicians were highly concerned about whether the adrenal mass was a metastasis. As mentioned in the literature, adrenal metastasis is the second most common tumor after adrenal adenoma, especially in people with a history of primary tumors, and solitary adrenal metastasis is common in patients with lung cancer with adrenal spread (6). The diagnosis of adrenal metastases was supported by the imaging features and the patient’s clinical history of lung cancer. Consequently, we provided a diagnosis of adrenal metastasis; however, the pathological results after the operation confirmed that the mass was in fact an adrenal angiomyolipoma.
Angiomyolipoma, a benign mesenchymal tumor originating from perivascular epithelioid cells, is composed of mature adipose tissue, smooth muscle, and thick-walled vessels (3). Angiomyolipoma is commonly found in the kidneys and liver but rarely appears in other places. Adrenal angiomyolipoma is typically asymptomatic and found incidentally during physical examination or routine US and CT examinations for another unrelated disease. Imaging examinations, such as US, CT, and magnetic resonance imaging (MRI), serve an important role in the diagnosis of adrenal angiomyolipoma, and the findings vary depending on the proportion of the components. Adrenal angiomyolipoma usually appears on imaging as round or ovoid with clear borders, low density, and no or mild enhancement. If the tumor is large (>4 cm) and inhomogeneous or has scattered calcifications, it is often misdiagnosed as a malignant tumor (7-10). One reported case of adrenal angiomyolipoma presented on US as a hyperechoic mass (11). Originating from perivascular epithelial cells, angiomyolipoma has a unique immunohistochemical and morphological structure (1). The immunohistochemical characteristics of the tumor are the positive expression of melanocyte markers (HMB-45, Melan-A, and Desmin) and smooth muscle actin (SMA) with negative expression of cytokeratin. The positive expression of HBM-45 in epithelioid or fusiform tumor cells is a diagnostic clue and is helpful in distinguishing this tumor from other similar lesions (4).
Based on large autopsy studies, the percentage of malignant tumors that progress to metastases in the adrenal glands is approximately 58% for breast cancer, 42% for lung cancer, 10.3% for esophageal cancer, 16% for gastric cancer, 50% for malignant melanoma, and 14% for colorectal cancer. Despite their small size, the adrenal glands are considered as the most common location for the metastatic spread of multiple malignant tumors (12). In the majority of cases, patients are asymptomatic, and the metastases are discovered incidentally during the follow-up of antecedent malignant disease. CT and MRI, as well as the evaluation of tumor characteristics, play a key role in the diagnosis of adrenal angiomyolipoma. In contrast to lipid-poor metastatic tumors, benign adrenal lesions contain abundant intracytoplasmic fat (an attenuation value of <10 Hounsfield units suggests a lipid-containing benign lesions). Small metastases are often homogeneous analogues of benign tumors, whereas large metastases frequently represent heterogeneous metastases as a result of hemorrhages and necroses within the lesions. Meanwhile, calcifications in metastases are rare (13). It should be emphasized that the CT features of adrenal metastases are nonspecific, and metastasis cannot be discriminated from benign lesions based on size alone (12). On MRI, the T2 signal of metastasis is higher than that of hormonally inactive and benign lesions. According to several authors, dynamic gadolinium-enhanced MRI and chemical-shift MRI may be helpful for distinguishing between metastatic tumors and benign lesions (13).
Angiomyolipomas are mainly composed of mature adipocytes, which facilitate an easy, accurate diagnosis based on the imaging and pathology results and distinction from metastasis. However, some angiomyolipomas mainly comprise epithelial smooth muscle, which makes it difficult to make a true diagnosis based on the imaging or pathology findings known to pathologists. At this time, the differential diagnoses of adrenal metastatic carcinoma, adrenal carcinoma, and renal cell carcinoma are challenging because of their epithelial morphology, especially in people with a history of cancer (3). Careful examination of the adipocytes and abnormal blood vessels is helpful for diagnosis (14). Two of the reported cases of adrenal angiomyolipoma were misdiagnosed as malignant tumors, one of which was diagnosed as an adrenal malignant tumor because of scattered calcifications in the adrenal mass (9). The other cases featured adrenal masses that were diagnosed as adrenal metastases because of the high uptake in the adrenal masses during systemic 18F-FDG PET/CT (15).
In the case we reported, the patient was misdiagnosed with adrenal metastasis based on his history of lung cancer and the findings for imaging examination (the mass significantly increased in size during the 2-year follow-up and showed obvious ring enhancement in the enhanced CT scan). The patient was asymptomatic, and the adrenal mass also showed unenhanced exudation-like changes on contrast-enhanced CT, which we suspect was caused by vascular rupture and bleeding caused by a lack of elastic fibers in the vascular wall of the angiomyolipoma. However, the appearance of adrenal metastases varies on CT, and they are usually asymptomatic. Metastasis can also manifest as bleeding and peripheral invasion (16). In addition, some adrenal metastases, such as renal clear cell carcinoma and hepatocellular carcinoma, contain lipids (17), and in these cases, it is difficult to distinguish adrenal metastases from angiomyolipoma. In summary, adrenal metastases usually have a high unenhanced density (>10 HU) and delayed contrast medium washout compared to adrenal angiomyolipoma (precontrast HU less than 10, no enhancement or mild enhancement). Local invasion, central necrosis, and irregular borders are predictors of adrenal metastasis. However, if the main component of the angiomyolipoma is epithelial smooth muscle, there is a lack of adipose tissue (as in our case), which makes it difficult to correctly distinguish from metastasis. Therefore, despite its rarity, adrenal angiomyolipoma should be considered in the differential diagnosis when an adrenal mass is incidentally found in a patient with a history of primary tumors.
Finally, if the tumor is smaller than 4 cm and the patient has no symptoms, routine US or CT examination should be recommended every 3–6 months (18). Surgical treatment or selective arterial embolization should be performed if the tumor is symptomatic or measures more than 4 cm (19), as large angiomyolipomas have a tendency to rupture spontaneously and there is a risk of local recurrence (14) and increased spontaneous bleeding (20). All of the patients reported with adrenal angiomyolipoma underwent surgery. In recent years, laparoscopic adrenalectomies have been primarily considered over open surgery because laparoscopic surgery is less invasive, has fewer complications and a lower mortality rate than open surgery (12,15).
Conclusions
In conclusion, metastatic tumors are the second most common adrenal tumor after adrenal adenoma, especially in patients with a history of primary tumors. Because of the rapid progression and highly invasive nature of metastatic tumors, an accurate diagnosis is of great significance for the follow-up treatment and prognosis of these patients. Although adrenal angiomyolipoma is uncommon, it should be considered as one of the differential diagnoses of adrenal metastasis.
Acknowledgments
Funding: This work was supported by the National Natural Science Foundation of China (grant No. 81760309), Science and Technology Foundation of Health and Family Planning Commission of Guizhou Province (grant No. gzwjkj2017-1-013).
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at http://dx.doi.org/10.21037/atm-20-3147
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/atm-20-3147). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. This study was approved by the ethics committee of The Affiliated Hospital of Zunyi Medical University, and written informed consent was obtained from the parents of the participant for the publication of this manuscript and any potentially-identifying images/information.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Martignoni G, Pea M, Reghellin D, et al. PEComas: the past, the present and the future. Virchows Arch 2008;452:119-32. [Crossref] [PubMed]
- Talwalkar SS, Shaheen SP 2nd. Extra-adrenal myelolipoma in the renal hilum: a case report and review of the literature. Arch Pathol Lab Med 2006;130:1049-52. [PubMed]
- D'Antonio A, Caleo A, Caleo O, et al. Monotypic epithelioid angiomyolipoma of the adrenal gland: an unusual site for a rare extrarenal tumor. Ann Diagn Pathol 2009;13:347-50. [Crossref] [PubMed]
- Goswami A, Sharma A, Khullar R, et al. Adrenal angiomyolipoma: A case report and review of literature. J Minim Access Surg 2014;10:213-5. [Crossref] [PubMed]
- Lam AK. Lipomatous tumours in adrenal gland: WHO updates and clinical implications. Endocr Relat Cancer 2017;24:R65-R79. [Crossref] [PubMed]
- Kim SH, Brennan MF, Russo P, et al. The role of surgery in the treatment of clinically isolated adrenal metastasis. Cancer 1998;82:389-94. [Crossref] [PubMed]
- Yener O, Ozcelik A. Angiomyolipoma of the right adrenal gland. ISRN Surg 2011;2011:102743. [Crossref] [PubMed]
- Hu H, Xi X. Giant adrenal angiomyolipoma. J Clin Endocrinol Metab 2012;97:3835-6. [Crossref] [PubMed]
- Kwazneski Ii D, Merrill M, Young J, et al. Angiomyolipoma and Malignant PEComa: Discussion of Two Rare Adrenal Tumors. Case Rep Oncol Med 2016;2016:5204092. [Crossref] [PubMed]
- Hafeez Bhatti AB, Dar FS, Pervez M. Adrenal angiomyolipoma. J Coll Physicians Surg Pak 2013;23:663-4. [PubMed]
- Kumar S. A rare case of adrenal angiomyolipoma. The European Society of Radiology (ESR) 2009. ()https://www.researchgate.net/publication/278020740
- Spartalis E, Drikos I, Ioannidis A, et al. Metastatic Carcinomas of the Adrenal Glands: From Diagnosis to Treatment. Anticancer Res 2019;39:2699-710. [Crossref] [PubMed]
- Wagnerova H, Lazurova I, Felsoci M. Adrenal metastases. Bratisl Lek Listy 2013;114:237-40. [PubMed]
- Godara R, Vashist MG, Singla SL, et al. Adrenal angiomyolipoma: A rare entity. Indian J Urol 2007;23:319-20. [Crossref] [PubMed]
- Li W, Pang H, Cao Y, et al. High 18F-Fluorodeoxyglucose Uptake in Adrenal Angiomyolipoma: Case Report and Review of Literature. Medicine (Baltimore) 2015;94:e900. [Crossref] [PubMed]
- Elsayes KM, Elmohr MM, Javadi S, et al. Mimics, pitfalls, and misdiagnoses of adrenal masses on CT and MRI. Abdom Radiol (NY) 2020;45:982-1000. [PubMed]
- Choi YA, Kim CK, Park BK, et al. Evaluation of adrenal metastases from renal cell carcinoma and hepatocellular carcinoma: use of delayed contrast-enhanced CT. Radiology 2013;266:514-20. [Crossref] [PubMed]
- Zhao J, Sun F, Jing X, et al. The diagnosis and treatment of primary adrenal lipomatous tumours in Chinese patients: A 31-year follow-up study. Can Urol Assoc J 2014;8:E132-6. [Crossref] [PubMed]
- Sutter R, Boehler A, Willmann JK. Adrenal angiomyolipoma in lymphangioleiomyomatosis. Eur Radiol 2007;17:565-6. [Crossref] [PubMed]
- Ghimire O, Wenzheng L, Huaping L, et al. Angiomyolipoma of the Adrenal Gland: A Report of Two Cases and Review of the Literature. Am J Case Rep 2017;18:989-94. [Crossref] [PubMed]