
Comparison of iPTH and calcium levels between total thyroidectomy and lobectomy: a prospective study of 840 thyroid cancers with three years of follow-up
Introduction
Hypoparathyroidism is the most common complication following thyroid surgery that can lead to myriad metabolic and physiologic disturbances, prolonged hospitalization, and the need for lifelong supplementation. Temporary hypoparathyroidism occurs in 10% to 15% of patients. Meanwhile, permanent hypoparathyroidism (pHPP) after thyroid surgery occurs in 0.2% to 10% of patients, depending on the center’s experience and the type of surgical procedure (1). These factors can result in manipulation of the parathyroid gland during surgery, devascularization of the parathyroid gland, or from inadvertent removal of the parathyroid gland with the thyroid specimen. The incidence rate of hypoparathyroidism on the first post-operative day was higher in the total thyroidectomy (TT) with the LN dissection group (83%) than in the TT group (39%) (2). It seems thyroidectomy without prophylactic central neck dissection (CND) is appropriate for small (T1 or T2), noninvasive, clinically node-negative PTC (cN0) and for most follicular cancers, which is a strong recommendation from 2015 American Thyroid Association Management Guidelines for Adult Patients with Thyroid Nodules and Differentiated Thyroid Cancer (3). While Chinese management guidelines for Thyroid Nodules and Differentiated Thyroid Cancer recommend performing the ipsilateral CND, in the condition, the parathyroid gland and recurrent laryngeal nerve are effectively retained (4). Since biochemical studies of post-thyroidectomy patients have shown that intact parathyroid hormone (iPTH) sampling is a valid and early predictor of post-operative parathyroid gland state (1). Nevertheless, limited data is available assessing parathyroid state after CND. The purpose of this study is to describe the iPTH early after CND and its relation to age, sex, BMI, Preop PTH, thyroiditis, diameter, and multifocal of PTC, T stage, the surgical procedure of thyroidectomy plus CND or TT plus CND, ipsilateral or bilateral CND, central lymph nodes excised (number and positive for metastases). Wheather total thyroidectomy or lobectomy for papillary thyroid carcinoma patients with clinically uninvolved neck lymph nodes (cN0) who have primary tumors (T1 or T2) could accompany prophylactic CND (ipsilateral or bilateral) to provide clearance of disease and be less complications. We present the following article in accordance with the STROBE reporting checklist (available at http://dx.doi.org/10.21037/atm-20-4554).
Methods
Patients
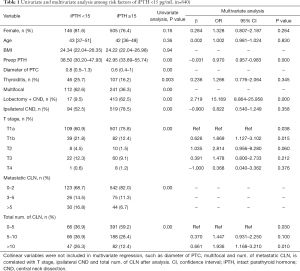
A prospective observational study was performed on patients who underwent thyroidectomy and CND with post-operative iPTH evaluation, from July 2016 to December 2016, at the Division of Thyroid Surgery, China-Japan Union Hospital of Jilin University, China. The preoperative FNA suggested cancer and underwent lobectomy and CND, as well as the total thyroidectomy and CND/lateral dissection, which were included in the iPTH tests. No financial association exists between the authors and the commercial companies whose iPTH determination systems are presented. Thyroidectomy without CND, “berry picking” dissection, re-do surgery, high basal iPTH values (15.00–65.00 pg/mL), concomitant parathyroid disease, renal failure was removed from this analysis. There appear to be 840 cases involved in this research (as Table 1), who evaluate iPTH 15min after CND by blood sampling. The protocol was approved by the Ethics Committee of China-Japan Union Hospital of Jilin University (2015-wjw006). All procedures performed in this study involving human participants were in accordance with the Declaration of Helsinki (as revised in 2013). Informed consent was taken from all the patients.
Full table
The technique of CND
Thyroidectomy and CND procedures have been performed from the same surgical team. Preservation of the parathyroid gland and its blood supply was attempted in all cases. The ATA consensus statement with reference to the terminology and classification of the central neck defines the CND as all perithyroidal and paratracheal soft tissue and lymph nodes with borders extending superiorly to the hyoid bone, inferiorly to the innominate artery, and laterally to the common carotid arteries (5). The technique applied is identical, and the procedure adopted supplies as the first step isolated thyroidectomy, after, as a second step, the CND is accomplished. That is, the CND dissection specimen is not excised en bloc during thyroidectomy. CND is conducted caudal to cranial. The surgical technique for prophylactic nodal dissection includes ipsilateral CND.
After thyroidectomy or CND, a rapid intraoperative pathological examination will guide whether the total thyroidectomy is performed. However, before submitting specimens, it is necessary to examine whether or not the samples contain parathyroid glands carefully. If they exist, it should be finely dissected along the parathyroid gland’s membrane, cut into small pieces as soon as possible, and auto planted. When the iPTH is low, even more, the careful examination must avoid the remains of parathyroid glands in pathological exam samples.
iPTH determinations
A peripheral blood sample for iPTH measurement was offered by the chemiluminescent immunometric method via the STAT-IntraOperative-Intact-PTH system (Roche’s automatic electrochemical luminous immune analyzer e602). The preoperative calcium and iPTH were assessed. Postoperatively, iPTH was sampled 15 minutes after CND. Post-operative serum calcium level (2.10–2.65 mmol/L) was sequentially measured per day during hospitalization despite the symptoms and periodically tested every six months until recovery of the parathyroid function or permanent hypocalcemia was diagnosed during three years follow-up. The symptoms of hypocalcemia include perioral or digital paresthesia, muscle cramping, or anxiety. Chvostek sign, facial twitching when the facial nerve is tapped, and Trousseau sign, ischemia-induced carpal spasm, highlight the state neuromuscular excitability during hypocalcemia (6,7). Patients with iPTH <15 pg/mL, are treated via calcium gluconate, intravenous injection, oral supplementation with calcium carbonate and calcitriol, under the serum calcium monitor. Asymptomatic patients presenting iPTH ≥15 pg/mL are treated via oral therapy with calcium carbonate. Patients were discharged when the serum calcium level >2.10 mmol/L and without signs and symptoms of hypocalcemia. Only oral calcium supplements without vitamin D analog (calcitriol, rocartrol) was started in patients during the follow-up period.
The primary outcome
IPTH after CND was considered as the primary endpoint, and it was compared to several variables. The following variables are considered: age, sex, BMI, Preop PTH, thyroiditis, diameter, and multifocal of PTC, T stage, the surgical procedure of thyroidectomy plus CND or TT plus CND, ipsilateral or bilateral CND, central lymph nodes excised (number and positive for metastases).
Statistics
The SPSS (Version 20.0) was used to perform statistical calculations. Quantitative variables were expressed as the median, 25 percentile, and 75 percentile. The patients were divided into two groups according to whether the post-operative iPTH <15 pg/mL and the non-parametric test was performed with the dependent variable indicators between the two groups. After considering P<0.05 in multivariate logistic regression, the independent variables predicting iPTH <15 pg/mL were screened by backward stepwise regression. In the logistics model, a Novo predictive value was assessed using the ROC curve, and the sensitivity, specificity, was determined. The area under the curve was used to stand for the accuracy of the predictions.
Results
Descriptive characteristics of the study population
840 PTC patients underwent thyroidectomy and CND with post-operative iPTH evaluation and were investigated. There were 189 men and 651 women; ages ranged from 20 to 82 years; median age, 42 years; BMI ranged from 15.60 to 51.42; median 24.22; diameter of PTC ranged from 0.10 to 5.00 cm; median 0.60 cm; preop PTH ranges from 15.15 to 145.20 pg/mL; median 42.95 pg/mL.
Of these PTCs, 487 (58%) were unifocal; 153 (18.2%) with thyroiditis; 610 (72.6%) stage T1a, 121 (14.4%) stage T1b, 18 (2.1%) stage T2, 82 (9.8%) stage T3, 9 (1.1%) stage T4; and 374 (44.52%) coexisting CLN metastasis. Overall, 430 lobectomies plus CND and 410 TT plus CND constituted this investigation. In all, 227 bilateral CND and 613 ipsilateral CND were performed. Of these CNDs, the No. of metastatic CLN was 0–2 in 665 (79.2%), 3–5 in 101 (12.0%), >5 in 74 (8.8%); the total No. of CLN was 0–5 in 457 (54.4%), 5–10 in 254 (30.2%), >10 in 129 (15.4%). During three years follow up, all patients have monitored the serum calcium level, and only one patient (0.12%) with constant hypocalcemia, <2.10 mmol/L, without perioral or digital paresthesias, and only an oral calcium supplement and vitamin D analog (calcitriol, rocartrol).
The relationship between the risk factors with the patterns of iPTH <15 pg/mL
Table 1 presents the univariate and multivariate analysis among risk factors of iPTH <15 pg/mL after thyroidectomy plus CND of the 840 patients. According to the results of univariate analysis, only age, sex and BMI showed no statistically significant difference between iPTH <15 pg/mL and iPTH ≥15. Collinear variables are not included in multivariate regression, such as the diameter of PTC (T stage), multifocal of PTC (ipsilateral or bilateral CND), metastatic CLN (total number of CLN). Thus, all other variables are considered in the multivariate logistic regression model. The backward stepwise method for the choice of variables was used in the model. However, only the Preop PTH (P<0.01) and type of surgical procedure (P<0.01) were significant variables for prediction of iPTH <15 pg/mL in PTC operation, the T stage (P=0.04) and the total number of CLN (P=0.03) were variables but not included in the final logistic model. The risk of iPTH, <15 pg/mL after TT plus CND, is 17 times that of lobectomy plus CND (OR =17.648, 95% confidence interval: 10.011–31.110).
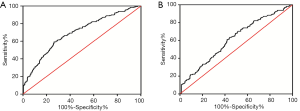
Since preop PTH and type of surgical procedure were the most important predictors for iPTH level 15 min after CND and the formulae were fitted by logistic regression and further simplified from 840 patients who underwent thyroidectomy plus CND: New Index =10 × type of surgical procedure (lobectomy =0, TT =1)-preop PTH-17. Based on the ROC curve, to predict the presence of iPTH <15 pg/mL was set up a cut-off point of New Index >−50. Of the 410 patients who underwent TT plus CND, preop PTH became the independent predictors for iPTH level 15 min after CND. Based on the ROC curve, to predict the absence of iPTH <15 pg/mL was set up a cut-off point preop PTH >42.16. As shown in Figure 1, the sensitivity (64.2%) and specificity value (67%) for prediction of thyroidectomy and sensitivity (63%) and specificity value (56%) for prediction of TT in separating patients who are going to be iPTH <15 pg/mL 15 min after CND. The biological index showed an area under the ROC curve of 0.697 and 0.613 separately.
Discussion
Hypocalcemia is undoubtedly the most frequent event after thyroidectomy, presenting an incidence between 0.3% and 43.0% for transient hypocalcemia and between 0 and 13.0% for permanent hypocalcemia (1,8,9). Even this was the most often observed complication more than recurrent laryngeal nerve injury. Other complications, as bleeding and recurrent nerve injury, usually occur in the immediate post-operative period. For this reason, hypocalcemia is the only complication that affects hospital discharge timing (10). Therefore, there is increased interest in the accurate description of morbidity related procedures. We choose to implement the selective use of PA, although several authors proposed reimplantation of at least one gland routinely in case of thyroid or neck surgery as a tool to reduce pHPP, which resulted in a range of 0 to 1.8% in their series (11). The procedure was performed only in case of clear damage to the vascular supply of parathyroid even after no obvious relief from scissors or punctures to the dark parathyroid, or evidence of intrathyroidal position or modification in gland color, that appears to be due to ischemia or insufficient venous drain. As well as when we find parathyroid from the tissue we attend to do the intraoperative pathological test, it is necessary to check before sending the sample routinely. The intraoperative serum PTH level monitoring is a guide to determine the need for selective PA (12). The technique of parathyroid tissue preparation for the graft is a minced gland with saline solution, fragmentation of the gland by scissors or scalpel, and direct reimplantation in intramuscular space 2–3 pocket(s). Also, we could intraoperative percutaneous injection of carbon nanoparticles (CNPs) for CNP-stained central compartment lymph nodes (CLNs) and passive display of parathyroid gland by CNP-stained thyroid (13). To give oral supply(calcium without vitamin D, analog) is enough for all symptomatic patients and asymptomatic patients with serum calcium <2.0 mmol/L during follow up.
PTH measurement also present important limitations to consider: (I) patient medical history. For example, the upper limit of the reference range for serum PTH should be well evaluated. Factors to be considered in analysis of serum PTH values in the upper reference range in patients with normocalcemia include obesity, race, 25-OHD levels, advanced age, serum creatinine, and dietary calcium intake. There are significant variation in theses subsets. (II) Standardization. Unfortunately, there are manufacturer’s reference ranges for serum PTH with use of different radioimmunometric assay, thus this establishes differences between centers. (III) Definitions. Lack of endocrine surgery guidelines and definition for transient or permeant hypocalcemia related to PTH values. (IV) Availability. PTH laboratories are not available in all hospitals, as well as PTH measurement is not available every day in some Hospitals. (V) Second vs. third generation PTH. PTH assay also measures fragments other than full-length PTH. (VI) Protocols. Lack of consensus consequences for treating supposed hypocalcemia related to PTH values. We need to establish panel for defined normal PTH or abnormal PTH. (VII) Sampling and storage conditions influencing the measurement of parathyroid hormone in blood samples are well described in the literature.
Thyroidectomy and CND are evolving into international guidelines (5). Most analyses have reported a small sample size and different results (1,2,5,8-10,14). Even if currently there is not a unanimous consensus on the use of iPTH in routine clinical settings (and in particular on its cut-off value and its sampling timing), this test appears to be a promising solution to this predictive need (15-17). The observation of iPTH starting from 15 minutes to hours after surgery is consistent with the half-life of the iPTH (which is about 4 minutes). Nevertheless, few studies evaluated the kinetics of iPTH levels after thyroidectomy and CND. The data presented may then confirm the hypothesis that CND contributes to hypoparathyroidism via disruption of the feeding arteries of the parathyroid glands and ischemic injury. Therefore, preservation of the vascular supply of the parathyroid glands is more critical in the prevention of post-operative hypoparathyroidism. En bloc resection of thyroid cancer with central compartment node dissection could increase the risk of injury to the blood supply of the parathyroid gland. The 2015 American Thyroid Association Management Guidelines for Adult Patients with Thyroid Nodules and Differentiated Thyroid Cancer gave a strong recommendation that Thyroid lobectomy alone may possibly be sufficient first treatment for low-risk papillary and follicular carcinomas. However, the treatment team may choose total thyroidectomy for enabling RAI therapy or for enhancing follow-up based upon disease features and/or patient preferences (3). While Chinese management guidelines for Thyroid Nodules and Differentiated Thyroid Cancer recommend performing the ipsilateral CND for DTC, in the condition, the parathyroid gland and recurrent laryngeal nerve are effectively retained (4).
This largest prospective study clarifies the kinetics of iPTH after 430 TT plus CND and 410 lobectomies plus CND, suggesting the relevance of perioperative iPTH decline in TT plus CND significantly (P<0.05), which risk of stopping iPTH <15 pg/mL even over 17 times. By the data, there was no difference between TT plus ipsilateral CND and TT plus bilateral CND. It seems no correlation of iPTH profile during the surgical procedure of compartment lymph node dissection (CLND) is significant. Furthermore, we describe a decrease in post-operative iPTH levels significantly related to the preoperative iPTH levels instead of the number of lymph nodes dissected or the metastatic ones. The cut-off value of iPTH resulted in more strongly associated with the preoperative iPTH levels and the type of surgical procedure. If the formulae result >−50 in thyroidectomy plus CND, or preop PTH <42.16 in TT plus CND, it will predict the presence of postop iPTH <15 pg/mL. Therefore, consistently with the literature results, it could possibly be argued that the systematic use of the immediately postoperatively iPTH assay or the following formulae with the type of surgical procedure and preop PTH may identify patients requiring calcium supplements, avoid unnecessary extensions of hospitalization days with direct benefits for both the patient and, in terms of costs, for the institution. Our study clarifies the kinetics of iPTH after 840 consecutive PTC thyroidectomy and lymph node clearance, and the permanent hypocalcemia was 0.12%. Combined with our earlier literature results, the incidence of nerve lesions during CND is lower than that of thyroidectomy (18). Compared to total thyroidectomy, lobectomy for papillary thyroid carcinoma patients with clinically uninvolved neck lymph nodes (cN0) who have primary tumors (T1 or T2) could accompany prophylactic CND (ipsilateral or bilateral) to provide clearance of disease.
Acknowledgments
Funding: The authors have no conflict of interest to disclose, and no other funding or financial relationship with the surgical industry. This study was supported by the National Natural Science Foundation of China (grant 81702652) and the Department of Science and Technology of Jilin Province, China (Grant Number 20200201181JC).
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at http://dx.doi.org/10.21037/atm-20-4554
Data Sharing Statement: Available at http://dx.doi.org/10.21037/atm-20-4554
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/atm-20-4554). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The protocol was approved by the Ethics Committee of China-Japan Union Hospital of Jilin University (2015-wjw006). All procedures performed in this study involving human participants were in accordance with the Declaration of Helsinki (as revised in 2013). Informed consent was taken from all the patients.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Julián MT, Balibrea JM, Granada ML, et al. Intact parathyroid hormone measurement at 24 hours after thyroid surgery as predictor of parathyroid function at long term. Am J Surg 2013;206:783-9. [Crossref] [PubMed]
- Yano Y, Masaki C, Sugino K, et al. Serum intact parathyroid hormone level after total thyroidectomy or total thyroidectomy plus lymph node dissection for thyroid nodules: report from 296 surgical cases. Int J Endocrinol Metab 2012;10:594-8. [Crossref] [PubMed]
- Haugen BR, Alexander EK, Bible KC, et al. 2015 American Thyroid Association Management Guidelines for Adult Patients with Thyroid Nodules and Differentiated Thyroid Cancer: The American Thyroid Association Guidelines Task Force on Thyroid Nodules and Differentiated Thyroid Cancer. Thyroid 2016;26:1-133. [Crossref] [PubMed]
- Chinese Society of Endocrinology, Medical Association; Chinese Society of Surgery, Medical Association; Committee for Head and Neck Oncology, Chinese Anti Cancer Association, et al. Management Guidelines for Thyroid Nodules and Differentiated Thyroid Cancer. Chinese Journal of Clinical Oncology 2012;39:1249-72.
- American Thyroid Association Surgery Working Group. American Association of Endocrine Surgeons. American Academy of Otolaryngology-Head and Neck Surgery; Consensus statement on the terminology and classification of central neck dissection for thyroid cancer. Thyroid 2009;19:1153-8. [Crossref]
- Bilezikian JP, Khan A, Potts JT Jr, et al. Hypoparathyroidism in the adult: epidemiology, diagnosis, pathophysiology, target-organ involvement, treatment, and challenges for future research. J Bone Miner Res 2011;26:2317-37. [Crossref] [PubMed]
- De Sanctis V, Soliman A, Fiscina B. Hypoparathyroidism: from diagnosis to treatment. Curr Opin Endocrinol Diabetes Obes 2012;19:435-42. [Crossref] [PubMed]
- Noordzij JP, Lee SL, Bernet VJ, et al. Early prediction of hypocalcemia after thyroidectomy using parathyroid hormone: an analysis of pooled individual patient data from nine observational studies. J Am Coll Surg 2007;205:748-54. [Crossref] [PubMed]
- Payne RJ, Hier MP, Côté V, et al. Postoperative parathyroid hormone levels in conjunction with corrected calcium values as a predictor of post-thyroidectomy hypocalcemia: review of outcomes 1 year after the implementation of a new protocol. J Otolaryngol 2005;34:323-7. [Crossref] [PubMed]
- Payne RJ, Hier MP, Tamilia M, et al. Same-day discharge after total thyroidectomy: the value of 6-hour serum parathyroid hormone and calcium levels. Head Neck 2005;27:1-7. [Crossref] [PubMed]
- Ahmed N, Aurangzeb M, Muslim M, et al. Routine parathyroid autotransplantation during total thyroidectomy: a procedure with predictable outcome. J Pak Med Assoc 2013;63:190-3. [PubMed]
- Promberger R, Ott J, Kober F, et al. Intra- and postoperative parathyroid hormone-kinetics do not advocate for autotransplantation of discolored parathyroid glands during thyroidectomy. Thyroid 2010;20:1371-5. [Crossref] [PubMed]
- Zhang D, Wang T, Dionigi G, et al. Application of Carbon Nanoparticles in Endoscopic Thyroidectomy via Bilateral Areola Approach: Total Thyroidectomy Plus Central Lymph Node Dissection. J Laparoendosc Adv Surg Tech A 2019;29:1038-41. [Crossref] [PubMed]
- Graciano AJ, Chone CT, Fischer CA. Applicability of immediate, late or serial intact parathyroid hormone measurement following total thyroidectomy. Braz J Otorhinolaryngol 2012;78:78-82. [Crossref] [PubMed]
- Vanderlei FA, Vieira JG, Hojaij FC, et al. Parathyroid hormone: an early predictor of symptomatic hypocalcemia after total thyroidectomy. Arq Bras Endocrinol Metabol 2012;56:168-72. [Crossref] [PubMed]
- Kim JP, Park JJ, Son HY, et al. Effectiveness of an i-PTH measurement in predicting post thyroidectomy hypocalcemia: prospective controlled study. Yonsei Med J 2013;54:637-42. [Crossref] [PubMed]
- Lang BH, Yih PC, Ng KK. A prospective evaluation of quick intraoperative parathyroid hormone assay at the time of skin closure in predicting clinically relevant hypocalcemia after thyroidectomy. World J Surg 2012;36:1300-6. [Crossref] [PubMed]
- Liu X, Zhang D, Zhang G, et al. Laryngeal nerve morbidity in 1.273 central node dissections for thyroid cancer. Surg Oncol 2018;27:A21-5. [Crossref] [PubMed]
(English Language Editor: J. Chapnick)


