Direct anterior approach for revision total hip arthroplasty
Introduction
The prevalence of revision total hip arthroplasty (THA) has significantly increased over the past few years, in direct proportion to the increasing number of primary THA cases (1-3). Revision THA rates have increased to 3.7 procedures per 100,000 persons per decade, and is estimated to increase by 137% with 97,000 cases per year by 2030 (2-4). The increase in revisions may be due to THAs being performed in younger and more active patients.
Indications for revision THA vary within literature and include loosening, instability, infection and periprosthetic fractures. In a review of the National Inpatient Sample database, the reasons for revision were as follows: instability 22.5%, mechanical loosening 19.7% and infection 14.8% (1). In another series, reasons for revision THA included aseptic loosening 55%, instability 14%, osteolysis 13%, infection 7% and periprosthetic fractures 5% (3). The first study found that isolated acetabular revision accounted for approximately two-thirds of revision THA cases. Thus, appropriate exposure and placement of components in THA are of utmost importance, no matter what surgical approach is employed.
Performing revisions through surgical approaches, such as the posterior, modified Hardinge and modified Watson-Jones, have been described. The direct anterior (DA) approach through the Smith-Petersen interval has been gaining popularity, and few papers have described revisions through this approach. Thus, the purpose of this paper is to describe surgical pearls and pitfalls for performing acetabular and femoral revisions through the DA approach, supplementing the descriptions with videos.
DA approach
The Smith-Petersen approach has commonly been used in orthopaedics, ranging from pediatric orthopaedics (developmental hip dysplasia) to adult reconstruction, surgical management of femoroacetabular impingement and treatment of hip fractures. The first written description of the DA approach was dated in 1881, and is attributed to Carl Heuter who was a physician with a special interest in anatomy (5). In 1917, Marius N. Smith-Petersen popularized this approach and became the eponym for this approach.
Anatomy
The DA approach goes through an internervous plane in its superficial and deep interval. The superficial interval is between the tensor fasciae lata (TFL) and the sartorious. The deep interval resides between the gluteus medius and the rectus femoris. The TFL originates from the anterior superior iliac spine (ASIS) and the outer lip of the anterior iliac crest and inserts into the iliotibial band. Its main actions are to stabilize the hip and knee joints by putting tension on the iliotibial band that serves as an accessory abductor muscle. It is innervated by the superior gluteal nerve that derives from the L4, L5 and S1 roots. The sartorius has a common origin with the TFL, as it runs from the ASIS and travels obliquely through the thigh to insert by the tibial tuberosity to form part of the pes anserinus. It contributes to hip flexion, lateral rotation of the hip and knee flexion. The sartorius is innervated by the femoral nerve, and is the only true internervous interval used to access the hip (6). By operating through these internervous plans, there may be less soft tissue damage that may be correlated with less muscle weakness and less loss of proprioception (4,7). For the second interval, the gluteus medius, or the main hip abductor, is commonly retracted laterally while the rectus femoralis muscle that originates from the superior acetabulum zone is retracted medially.
Indications and contraindications
There are no absolute indications for performing revision THA through the DA approach, as this approach can virtually be used in every case. One may consider performing revision THA if the primary approach was through the same interval. It is important that an experienced surgeon in the DA approach performed revision THA with a trained and efficient surgical team. The ideal patient for the DA approach in the primary and revision setting is a less muscular person with a body mass index less than 30 kg/m2 with adequate femoral offset (4,8). Patients with skin folds or fat that overlies the surgical incision may have increased risk of wound healing complications, but this can be minimized with appropriate wound dressings. A contraindication to this approach is the lack of appropriate instruments, as using curved and angulated instruments specific for this surgical approach is crucial (7).
Technique for DA revision THA
The most important aspect of the DA approach for primary and revision THA is to obtain adequate exposure. Thus, careful detail must be paid to every step of the process, as described below.
Setup
Patients are placed supine on the operating table. Judet (9) initially described that the DA approach for THA should be performed using an orthopaedic, traction table (5). A standard operative table can be used for this approach that can be flexed at the midpoint of the table if required to increase femoral exposure (Figure 1) (4,10). An arm board can be placed distally on the table contralateral to the operative side, which supports the abducted non-operative leg when exposing the femur. Draping can be performed to either expose one or both legs. Draping out both extremities may have the advantage of allowing the operated leg to be placed under the other to improve adduction of the hip. Some authors describe the use and of fluoroscopy for acetabular component positioning (10,11).
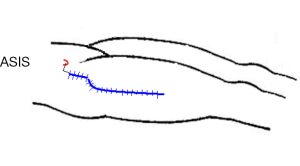
The skin incision for a revision direct anterior (DA) total hip arthroplasty (THA) can be carried out posteriorly and distally to adequately achieve distal femoral exposure. The proximal mark is the anterior superior iliac spine (ASIS).
Incision and surgical approach
If a prior DA incision is present, the same incision should be used. The starting point of the incision is located approximately 2 cm distally and 2 cm laterally to the ASIS (4). The incision is carried out distally along the axis of the TFL for approximately 10 cm; if additional exposure is needed, the incision can be extended proximally and distally. In the revision setting, there may be excessive scar tissue present, so care must be taken to identify the interval between the TFL and sartorius carefully. As the TFL fascia is incised, the split should be performed in line with the muscle fibers and be made slightly lateral to the true interval but in the medial third of the muscle. This is aimed to protect fibers of the lateral femoral cutaneous nerve but at the same allow proper exposure with less chance of TFL damage. A sharp Hohman retractor should placed just distal and lateral to the vastus ridge on the femur to retract the TFL laterally. A blunt, long handled Hohman retractor should be placed around the superior femor neck and a Hibbs retractor should be used to retract the sartorious and rectus medially. The fascia overlying the vastus lateralis should be incised from lateral to medial, and the vessels should be identified and cauterized. The capsule should be exposed, and an adequate capsular excision must be performed; failure to excise enough capsules is the most common reason for improper visualization of structures (6).
Acetabular component management
Once the hip has been dislocated and the femoral head component has been removed, the femur should be placed in a soft tissue pocket posterior to the acetabulum. If the femoral component is not removed, flexion of the hip will allow retractors to move the femoral component posteriorly and allow visualization of the acetabulum. The retractors must be placed appropriately to achieve adequate visualization. The first sharp retractor should be placed on the posterolateral acetabulum to expose the posterior column. The second sharp, lighted retractor may need to be repositioned over the anterior column to provide adequate visualization of the acetabulum. In most revision cases, this pocket has already been developed. Attention should be paid to potential vessels inferior to the medial acetabular cup that may need to be cauterized. If the inferomedial capsule has not been excised from the previous surgery, use electrocautery to make an opening in the capsule to place a blunt retractor and expose the medial portion of the acetabulum. These three retractors should all be placed at 90º angles to each other. If additional acetabular exposure is needed, a double footed or double angled retractor can be placed on the ischium, but it must be removed prior to placement of a new implant.
Once exposed, the cup can be appropriately inspected. If the acetabular component does not need to be removed, one may consider placing an inclined acetabular liner within the existing cup, depending on the existing placement of the cup.
If the acetabular cup requires revision, it can be successfully removed with the use of various instruments, such as curved osteotomes or dedicated cup explant instruments. These instruments minimize the amount of bone that is removed. Once the cup is removed, one must assess the remaining bone stock. When positioning acetabular components, special attention must be placed on cup orientation. In the case of the DA approach, an angled cup impactor must be used and a flexible screwdriver must be available if supplementary screw fixation is required. Positioning of reconstruction devices such as cages or cup-cages can successfully be placed using this approach.
Femoral component management
When addressing the femur through the DA approach, there are many surgical pearls that are helpful for achieving adequate exposure. The first and most important point is to understand that hip extension is not the most important element of femoral component exposure for primary and revision surgery. A simple gel bump can be placed under the pelvis/sacrum, such that the middle of the gel is at the level of the ASIS, thus increasing hip extension enough to perform most femoral revisions. Occasionally, further extension is required, so a table that can be placed in further extension is helpful. The most important elements of femoral exposure for the DA approach are external rotation and adduction of the hip. Externally rotating the limb allows access to the posterior capsule and external rotators that may need to be released to allow for proper femoral elevation. Once the femur is elevated, adduction of the leg while maintaining external rotation allows for access to the femur.
To achieve distal femoral exposure (Figure 1), the skin incision should be directed posteriorly towards the midline of the femur. The goal of this dissection is to reflect the TFL posteriorly and then to dissect through the vastus lateralis distally. The vastus lateralis can then be split as far distal as required for the revision surgery. This exposure can be used when a cerclage wire is needed around the femur or a femoral extended trochanteric osteotomy (ETO) must be performed.
ETOs are of great utility in revision THA, as an osteotomy is performed on the lateral aspect of the femur. As described by Younger et al., an ETO is aimed to access and achieve easier removal of distally fixed cemented and cementless femoral components. This osteotomy is carried out distally from the greater trochanter. One of the key aspects is to maintain an intact muscle-osseous sleeve which is composed mainly of the gluteus medius, greater trochanter, vastus lateralis and femoral diaphysis fragment (12). One should measure the length of the osteotomy site preoperatively so that the femoral stem may be removed and that there is sufficient space to allow secure attachment of hardware to allow for adequate fixation. Various techniques have been described for femoral fixation, ranging from wires, cables to sutures, as secure fixation is required to prevent nonunion and to restore the abductor mechanism (13).
As seen in Figure 2, the femoral osteotomy is performed to open the femur fragment posteriorly. A template of the cut is first drawn using a marker. A saw is used to cut the anterior lateral aspect of the cortical bone. During the initial approach, the aim is to create a single bony cut (an episiotomy) that may be adequate to remove the femoral component. This technique has been successful in our practice and avoids completing the total osteotomy. If this initial step is not sufficient, a complete osteotomy should be carried out. The use of a high speed burr is preferred to avoid creating a potential stress riser at the junction of the vertical and the horizontal cuts. The posterior cut is marked out with a drill bit, with multiple perforations being made through the bone. A posterior hinge is created and the osteotomy is opened using two osteotomes. Fracturing the fragment must be avoided and leaving a periosteal sleeve around one edge (anterior or posterior) is preferable (Figure 3). This technique is an anterior to the posterior ETO technique in contradistinction to that described by Younger et al.

To achieve proximal exposure from the Smith-Petersen approach, the approach can be modified by performing a proximal extension through the TFL fascia, similar to an extension of the iliofemoral approach. The TFL should be incised near the ASIS, being careful to protect the lateral femoral cutaneous nerve. Proximal mobilization of the TFL allows access to the gluteus medius and a subperiosteal dissection carried out underneath the gluteus minimus leads to the interspinous crest. This extended incision can then be used to access the anterior and posterior column. If greater posterior exposure is needed, the TFL can be detached (10). During wound closure, the TFL can be repaired and closed as one sleeve.
Complications of DA revision THA
As with every hip approach, there are potential complications. In both primary and revision DA approach, the lateral femoral cutaneous nerve can become injured. This nerve has various anatomic variations in relation to the number of branches from which it divides. Occasionally, some branches are stretched on irritated and numbness around the surgical site may result. When the nerve itself gets injured, patients may develop painful meralgia paresthetica, but this is very rare (16).
Given the location of the incision, DA THA patients may have higher rates of wound complication, especially in obese patients or patients with pannus overlapping the surgical site. Special occlusive dressings can be utilized to eliminate this problem. To our knowledge there is no published data in regards to complications using the DA for revision arthroplasty.
Conclusions
Revision THA can be successfully performed through the DA approach. The DA approach does not split muscles, as in other approaches, and studies have demonstrated improved strength, proprioception and healing in the postoperative period. Acetabular and femoral exposure are crucial for achieving correct component positioning, which requires appropriate retractor positioning, specific instrumentation for the DA approach, correct patient positioning and a well-trained team. Femoral exposure can be enhanced by extending the existing incision proximally or distally and by performing an ETO. When applying the surgical pearls provided in this paper and video, revision THA through the DA approach can become a replicable procedure with great clinical results.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Bozic KJ, Kurtz SM, Lau E, et al. The epidemiology of revision total hip arthroplasty in the United States. J Bone Joint Surg Am 2009;91:128-33. [PubMed]
- Kurtz S, Ong K, Lau E, et al. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am 2007;89:780-5. [PubMed]
- Kurtz S, Mowat F, Ong K, et al. Prevalence of primary and revision total hip and knee arthroplasty in the United States from 1990 through 2002. J Bone Joint Surg Am 2005;87:1487-97. [PubMed]
- Bender B, Nogler M, Hozack WJ. Direct anterior approach for total hip arthroplasty. Orthop Clin North Am 2009;40:321-8. [PubMed]
- Rachbauer F, Kain MS, Leunig M. The history of the anterior approach to the hip. Orthop Clin North Am 2009;40:311-20. [PubMed]
- Kennon R, Keggi J, Zatorski LE, et al. Anterior approach for total hip arthroplasty: beyond the minimally invasive technique. J Bone Joint Surg Am 2004;86-A Suppl 2:91-7. [PubMed]
- Vail TP, Callaghan JJ. Minimal incision total hip arthroplasty. J Am Acad Orthop Surg 2007;15:707-15. [PubMed]
- Nogler M, Mayr E, Krismer M. The direct anterior approach to the hip revision. Oper Orthop Traumatol 2012;24:153-64. [PubMed]
- Judet J, Judet H. Anterior approach in total hiparthroplasty. Presse Med 1985;14:1031-3. [PubMed]
- Mast NH, Laude F. Revision total hip arthroplasty performed through the Hueter interval. J Bone Joint Surg Am 2011;93 Suppl 2:143-8. [PubMed]
- Foster DE, Hunter JR. The direct lateral approach to the hip for arthroplasty. Advantages and complications. Orthopedics 1987;10:274-80. [PubMed]
- Younger TI, Bradford MS, Magnus RE, et al. Extended proximal femoral osteotomy. A new technique for femoral revision arthroplasty. J Arthroplasty 1995;10:329-38. [PubMed]
- Kuruvalli RR, Landsmeer R, Debnath UK, et al. A new technique to reattach an extended trochanteric osteotomy in revision THA using suture cord. Clin Orthop Relat Res 2008;466:1444-8. [PubMed]
- Manrique J, Chen AF, Heller S, et al. Partial extended trochanteric osteotomy. Asvide 2014;1:286. Available online: http://www.asvide.com/articles/299
- Manrique J, Chen AF, Heller S, et al. Full extended trochanteric osteotomy. Asvide 2014;1:287. Available online: http://www.asvide.com/articles/300
- Goulding K, Beaulé PE, Kim PR, et al. Incidence of lateral femoral cutaneous nerve neuropraxia after anterior approach hip arthroplasty. Clin Orthop Relat Res 2010;468:2397-404. [PubMed]


