
The reduction of vertical food impact using adjacent surface retaining zirconium crowns preparation technique: a 1-year follow-up prospective clinical study
Introduction
When chewing food, the occlusal force could wedge food into interproximal periodontal tissue called food impact, which could be classified into vertical or horizontal. Compare to horizontal food impact. The vertical ones may cause a more uncomfortable experience in patients from long-term clinical observation. Full crown, half-crown, and inlay are often used to repair the defect of grinding teeth, or after root canal treatment to protect the teeth (1). However, those repairing methods may end up with food impact because of the loss of adjacent contact. Then subsequently cause caries of the adjacent teeth (63%), caries of abutment teeth (41%), pocket formation (55%), and interdental bone loss (48%) (2). Heat-pressed glass-ceramic material, which low presenting strength, elevated risk of fractures for this brittle property, mostly made the semi-crown or inlay. Food impact resulting from faulty constructed restoration could be best avoided if suitable precautions are taken while designing the prosthesis (2). Considering those problems during clinical practice, we conducted a partial full zirconium crown preparation method, which designedly leaves adjacent openings to keep the original normal adjacent contact area of molars and then followed the patients for 1 year. We present the following article in accordance with the STROBE reporting checklist (available at http://dx.doi.org/10.21037/atm-20-5582).
Methods
Materials
Zirconia blocks (Altron, China); Silicone rubber (DMG, Germany); Glass ion cement bonding joint (Fuji I, Japan); Silicone rubber grinding head (Songfeng, Japan).
Study methods
Dental preparation
Occlusal surface and buccal/lingual wall: the preparation thickness is greater than 1.0 mm to ensure the thickness of the zirconium crown is more than 0.7 mm.
Margin placement: using shallow concave or round right-angled burs to prepare shoulder. A supragingival position of the margin was chosen in this study.
Proximal walls:
❖ Treatment group: for those with no defect in the adjacent tooth body, all adjacent areas were retained. Only adjacent buccal/lingual abductor tooth body tissues were prepared, and the buccal and lingual axial wall was formed a parallel, as shown in Figure 1.
❖ Partial defect of adjacent teeth: since the crown adjacent area of partial defect has been repaired with photocured resin, conventional preparation is made to the gingival autogenous tooth tissue, and the adjacent area of the gingival part is retained. The gap of adjacent preparation is greater than 1 mm, as shown in Figure 1.
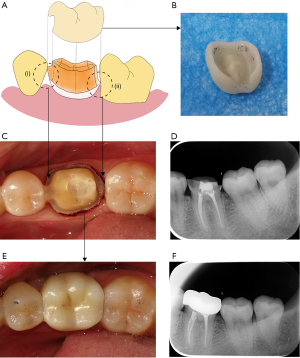
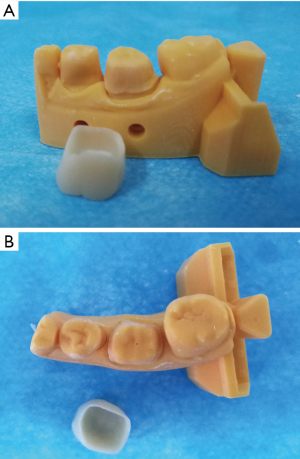
Control Group: for all-ceramic restorations, a smooth internal geometry has been an accepted doctrine for many years. The tooth structure was removed for all the surfaces to form around and blunt shape, then fully polished (Figure 2).
Impression
The gingival retraction conducted the double string technique. An extra-thin cord (Ultrapack no.00) was prepacked into the entire crevice. Then a thin kitted cord (Ultrapack no.0) was packed into the crevice and would be removed to allow the impression material into it. The silicone rubber was used to take the impression, which cast with die stone to ensure a clear cervical margin line of the teeth.
Manufacturing requirements of the technician
All molars are repaired with non-glazed zirconium crowns. In the treatment group, only the adjacent area of the crown should be restored, and the normal abduction gap of a buccal, lingual, and occlusal square should be formed.
In the control group, if the adjacent teeth were healthy, the adjacent area was reconstructed. If abutment or adjacent teeth were loose, or were the last teeth in the dental arch, besides the reconstruction of the adjacent area, it is necessary to increase the area of the contact area to form a concave and convex adjacent relation.
Orthodontic considerations
When the crown was fully in position, the cervical margin needed to fit precisely to the finishing line. Then the occlusion needed to be adjusted to normal or light contact to eliminate the early contact of a non-centric relation position. If the tooth was the ended one in the dental arch, the early contact area near the middle-inclined plane of all tooth tips needed to be eliminated. In the meantime, there was close contact between the adjacent surface, and the dental floss cannot easily pass the interproximal space (Figure 1E). There was moderate friction between the crown and the prepared tooth to ensure the retention force.
Data analysis
The data analysis was conducted by using SPSS17.0 software. Then, a Chi-square test was used to analyze the statistical difference. P<0.05 was considered statistically significant.
All procedures performed in this study involving human participants were in accordance with the Declaration of Helsinki (as revised in 2013). This study was approved by the Ethics Committee of Sichuan Academy of Medical Sciences & Sichuan Provincial People’s Hospital (No. 387.2020) and informed consent was taken from all the patients.
Results
Patients’ feature
Thirty-eight patients aged from 18 to 70, the average age was 45.5 years (21 were male, and 17 were female) were included in this study, who visited in our department from May 2017 to May 2018. They had molar teeth defect or need tooth crown restoration after root canal treatment. Forty-six molars were included in this study, containing the 29 first molar and 17-second molar. The objective adjacent face has been researched was 80.
Inclusion criteria
All molars without loosening or mobility were <I°. Each molar had at least one adjacent tooth tissue without defect or crown defect, and no food impact. A complete root canal treatment for pulp problems was performed.
Restoration evaluation criteria and patients’ management
According to the evaluation standards of the American public health association (3), patients were followed up on 1, 6, 12 months. The data, including a questionnaire, radiography, mobility, and probing, were recorded on regular check-ups.
Restoration evaluation result
Eighty adjacency surfaces of 46 molars, 48 were in the treatment group (T group), and 32 were in the control group (C group). The food impact was identified when a explicit food insertion between the natural teeth and the proximal surface of the crown prosthesis was be found. The food impact occurred in only one patient in the T group, whereas there were 3 cases occurred food impact in the C group at 6 months. In the 12-month follow-up, the number was increased to 5 cases. Compare to the treatment group. The difference was statistically significant. Other inspection results were shown in Table 1.
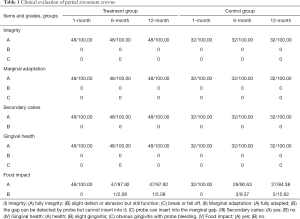
Full table
Discussion
Food impact problem
Food impact was a common side effect that often occurs during crown restoration. It has been reported that food impact accounted for 17.5% of the failed cases of fixed denture restoration, 62.5% of which was caused by poor contact between the full crown prosthesis and adjacent teeth (4).
The natural tooth adjacent contact relation is diverse and complex, and the adjacent area varies with age, tooth arrangement, crowding, and chewing force (5). For the traditional tooth preparation method, the normal contact relationship was reconstructed by the crown, which was challenging to reproduce the original natural tooth contact relation. And the result would be more complex if the adjacent tooth was injured during the preparation or the adjacent relation was not appropriately restored by the technician. All those uncertain factors may increase the probability of the food impact of restoration (6,7).
In this study, we compared the traditional tooth preparation method and an alternative method, which remained in the adjacent area to keep the original contact relationship. The result showed that there was no food impact on the new method group after a one-year follow-up. For those with the adjacent surface already destroyed by caries or other reasons, even if only if they kept a small hard tissue near the gingival would reduce the food impact. These factors may attribute to the explicit direction provided by the adjacent gingival hard tissue, which could help technicians to reconstruct the contact area of the crown.
In the control group, several details were emphasized to avoid the food impact for long term observation, like appropriately increase contact area surface, or adjust to slight tight contact. When dealing with I–II° loosen teeth or second molar (w/o third molar), even though there is a better adjacency relationship of static reconstruction, it is difficult to control the adjacent dynamic changes and occlusive grinding of the chewing movement—thus increased the probability of food impact. Reserving adjacent areas would help to keep the complex adjacent relationship of natural teeth and decrease food impact.
Strength problem
In recent years, heat-pressed glass-ceramic material was wildly used to make restoration. For those who preserved the adjacency relationship between the proximal and distal middle surfaces of teeth, could reduce the occurrence of food impact. For adjacent area reconstruction, compared to the traditional whole-crown restoration, they did not show better results in a good edge close and preventing food impact (8).
Besides, the strength of glass ceramics is low, ranging from 360 to 450 MPa. Fracture and porcelain breakage are common problems. To overcome this problem, the thickness of restoration is usually greater than 1.5–2 mm and even more than 2 mm for inlay crown, which may sacrifice a sizeable amount of dental tissue.
In this study, we used a zirconium crown, in which bending strength could reach 900–1,200 Mpa to reduce the thickness to 0.7 mm. This partial zirconium crown supplied sufficient strength and effectively reduced porcelain collapse, remain tooth tissue as much as possible at the same time, unlike the glass-ceramics that could get sufficient retentive force through bonding technology. Zirconia needs to be paid more attention to strengthen the mechanical friction retentive force. The goal could be achieved by accurate preparation of the parallel axial wall of buccal and lingual surfaces and using supplementary retention form in tooth preparation.
Dental attrition
Whether the zirconium crown can cause excessive wear of maxillary teeth has been a concern of clinicians. Many studies have shown that the wear behavior of ceramics has little correlation with its hardness (9). The wear of highly polished zirconium crown surface on the natural teeth of opposite jaws is slight, and less than that of thermo-die-cast glass ceramics, with a high success rate.
Conclusions
Compare to the traditional tooth preparation method, keep adjacent areas of the tooth to reserve a space for partial zirconium crowns would significantly reduce the food impact for a 1-year follow-up. This method would exploit the advantages of zirconium material to the full, which presented good mechanical strength and biocompatibility, reducing the risk of porcelain breakage, and protected residual dental tissues. It is efficiently conducted in clinical practice. Although the short-term clinical effect is good, the long-term effect needs further observation and research.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at http://dx.doi.org/10.21037/atm-20-5582
Data Sharing Statement: Available at http://dx.doi.org/10.21037/atm-20-5582
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/atm-20-5582). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study involving human participants were in accordance with the Declaration of Helsinki (as revised in 2013). This study was approved by the Ethics Committee of Sichuan Academy of Medical Sciences & Sichuan Provincial People’s Hospital (No. 387.2020) and informed consent was taken from all the patients.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Chen Y, Li MX, Zhang Y. Effect analysis of ceramic onlay to repair serious dental defects in young permanent molars. Hua Xi Kou Qiang Yi Xue Za Zhi 2019;37:299-303. [PubMed]
- Nagarsekar A, Gaunkar R, Aras M. Knowledge, attitude, and practice of dental professionals regarding the effect and management of food impaction associated with fixed partial denture prostheses: A survey. J Indian Prosthodont Soc 2016;16:372-9. [Crossref] [PubMed]
- Rosenblum MA, Schulman A. A review of all-ceramic restorations. J Am Dent Assoc 1997;128:297-307. [Crossref] [PubMed]
- Kebing L, Xiaohong W, Wanning H. Cause of food impaction after fixed denture restoration and therapeutic effect of gap expansion and resin repair. Hua Xi Kou Qiang Yi Xue Za Zhi 2016;34:395-7. [PubMed]
- Li ZL, Wu F, Li LL, et al. Etiology and clinical technology of the food impaction with tight proximal contacts. Zhonghua Kou Qiang Yi Xue Za Zhi 2019;54:278-81. [PubMed]
- Li QL, Ying CC, Xu QJ et al. Atraumatic Restoration of Vertical Food Impaction with an Open Contact Using Flowable Composite Resin Aided by Cerclage Wire under Tension. Scientifica (Cairo) 2016;2016:4127472.
- Al AMD, Kellesarian SV. Crestal Bone Loss Around Adjacent Dental Implants Restored with Splinted and Nonsplinted Fixed Restorations: A Systematic Literature Review. J Prosthodont 2017;26:495-501. [Crossref] [PubMed]
- Kale E, Yilmaz B, Seker E, et al. Effect of fabrication stages and cementation on the marginal fit of CAD-CAM monolithic zirconia crowns. J Prosthet Dent 2017;118:736-41. [Crossref] [PubMed]
- Chopra A, Sivaraman K, Narayan AI, et al. Etiology and classification of food impaction around implants and implant-retained prosthesis. Clin Implant Dent Relat Res 2019;21:391-7. [Crossref] [PubMed]


