
Impact of cataract screening integrated into establishment of resident health record on surgical output in a rural area of south China
Introduction
According to the World Health Organization (WHO) report in 2017, it was estimated that 253 million people lived with visual impairment, and 36 million were blind (1). Unoperated cataract is the leading cause of blindness and the second cause of moderate and severe visual impairment (MSVI), especially in the low to middle-income developing countries, accounting for 51% cases of blindness and 33% cases of MSVI (2-4). Provision of sufficient, successful, and sustainable cataract surgical services was endorsed as a priority in all countries by the WHO and International Agency for the Prevention of Blindness (IAPB) since 1999 (5,6).
The cataract surgical rate (CSR) is a critical indicator to evaluate the accessibility to cataract services in a country (7). China is the largest developing country in the world; however, the CSR of China (370/million/y in 2000 and 800/million/y in 2009) (8) was used to be far behind other countries, including America (11,000/million/y) (9), Sweden (9,000/million/y) (10), and India (5,300/million/y) (11). With the development of social economy, application of Universal Medical Insurance and the endeavor of non-governmental organizations (NGOs), the CSR of China is increasing in the past decade (1,782/million/y in 2015, 2,070 in 2016 and 2,205 million/y in 2017) (12). However, the numbers of incident cataract and visually impaired cataract patients are still growing in China. The 2014 Nine-Province Survey in rural China showed that 16.4%-56.6% of patients with cataract-related severe visual impairment or blindness had not received cataract surgery (13). Furthermore, CSR is seriously imbalanced between different areas, which is significantly lower in rural area than urban area due to the poor socioeconomic status and lack of eye-care infrastructure (14,15). Hence it is crucial to increase the surgical output and improve the access to eye-care service in rural China.
Cataract screening was considered to be the most beneficial method for increasing CSR in rural area (16-18). A variety number of programs have been implemented in some rural areas of China, including free cataract screening (16,18,19) and low-priced surgery (20-22). However, these programs were executed by public hospitals or research groups, and intermittently sponsored by NGOs, government or research funds (16,18,19,21). These approaches suffered limited sustainability and efficiency, which necessitates the development of novel screening models (17).
Private sectors have increased dramatically in the past decades, and contributed to the prevention of blindness in China. However, their role and efficacy in increasing the output of cataract surgery remain elusive. In addition, the Chinese Ministry of Health (MOH) issued the guidance on standardizing the management of health records of urban and rural residents in 2009 (23), which appeals annually health physical examinations for all residents in community health service centers. In the rural area of Zhaoqing prefecture, a novel cataract screening model was constructed by combining private hospital screening with establishment of resident health record. Therefore, the aim of this study was (I) to investigate the impact of this new cataract screening model on the output of cataract surgery, (II) to assess the accessibility to eye-care services and barriers to cataract surgery in rural China. We present the following article in accordance with the MDAR checklist and STROBE reporting checklist (available at http://dx.doi.org/10.21037/atm-20-396).
Methods
Study design and ethics
This was a prospective observational study and a STROBE checklist is provided in the Supplementary file. Participants aged 50 years and older who received cataract screening from January 2015 to December 2017 in rural area of Zhaoqing prefecture were enrolled. Demographic information, economic and education status, CSR and outcome of the screening population were recorded. Accessibility to eye-care service and barriers to cataract surgery were evaluated in a subgroup of 500 patients who underwent surgery by questionnaire interview in 2015 and 2018, respectively. Those who refused to respond or failed to understand the question were excluded. This study was consistent with the tenets of the Declaration of Helsinki (as revised in 2013) and was approved by the ethics committee of Zhongshan Ophthalmic Center, Sun Yat-sen University and Zhaoqing Minsheng Eye Hospital (2014MEKY032). Oral informed consent was obtained from each participant (provision of written consent was exempted by the IRB-ZOC-SYSU).
Study sites
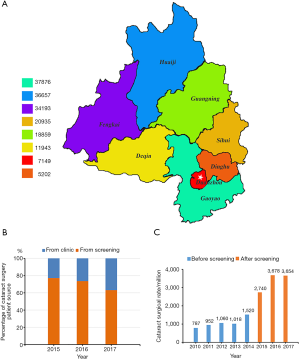
Zhaoqing prefecture, with an area of 14,900 km2, is located in midwest of Guangdong Province in south China. It is comprised of three districts (Dinghu, Duanzhou and Gaoyao) and five counties (Sihui, Deqing, Guangning, Huaiji and Fengkai). It was estimated that the population in Zhaoqing was 4,151,700, and 52.24% lived in rural areas in 2018 (24). Mountainous areas, mostly in Huaiji, Guangning, Fengkai and Deqing, account for 81 percent area of Zhaoqing, resulting in a relatively poor and underdeveloped economic status. According to the Statistical Bureau of Guangdong Province, the annual per capita disposable income was 24,071 RMB (3,408 US dollar) for all residents and 17,696 RMB (2,505 US dollar) for rural residents in Zhaoqing in 2018, which was much lower than the average level of 35,810 RMB (5,070 US dollar) of Guangdong Province in the same year (24,25). The low socioeconomic status of rural residents in Zhaoqing, especially those in mountainous areas, may represent the underdeveloped areas in rural China.
Cataract screening
Previous cataract screening models were based on public hospital or research group targeting specific population. While this novel screening model was based on private hospital and screening team which was incorporated into the project of resident health record of MOH, targeting all people in the area. Cataract screening was conducted by the Zhaoqing Minsheng Eye Hospital, a private hospital established in 2015. Cataract screening was carried out from January 2015 to December 2017, in collaboration with the local health administration department. Three outreach teams were set up to carry out cataract screening in different township hospitals and village clinics, at the same time when the annually health examination was conducted to establish the resident health record. Every outreach screening team includes 1 ophthalmologist, 1 nurse, and 1 coordinator. After physical examination and laboratory test were conducted by physicians from local hospitals, visual acuity, slit-lamp microscopy and fundoscopy were examined by the screening team for participants aged 50 years and older. The presenting visual acuity (PVA) was measured for each eye separately, and pin hole visual acuity was measured when PVA is less than 20/40 at a distance of 4 m in a well-lighted area by a nurse using an EDTRS tumbling-E chart. Patients with pin hole visual acuity less than 20/63 due to cataract were recommended to have further examination or surgery in the eye hospital and free transportations were provided. Patients with referable vision threatening conditions such as keratopathy, glaucoma, and retinopathy were also referred to the eye hospital.
Cataract surgery and follow up
Patients with a best corrected visual acuity (BCVA) less than 20/63 due to cataract were recommended for cataract surgery. All cataract surgeries were performed in the Zhaoqing Minsheng Eye Hospital by experienced cataract surgeons. Two surgery options, manual small-incision cataract surgery (MSICS) or phacoemulsification, were provided. MSICS was performed on patients with grade 4 or higher lens nucleus hardness according to the Emery-Little classification (13), corneal endothelial cell density low than 1,000/mm2, or cataract in hypermature stage. Patients selected the type of intraocular lens (IOL) according to their economic status. Unfoldable IOLs were provided with 500 RMB (71 US dollar), while foldable IOLs charged 1,000–3,000 RMB (142–425 US dollar). The cataract surgery fee was subsidized by the New Rural Cooperative Medical System. All patients received ophthalmic examinations at 1 week, 1 month, 3 months, 6 months, and 1 year after the surgery, including BCVA test, intraocular pressure (IOP), slit-lamp microscopy, and fundoscopy examination.
Questionnaire and data collection
A customized questionnaire was administered to investigate the accessibility to eye-care service and barriers to cataract surgery (Supplementary file). It comprises 9 questions, including 2 questions regarding demographic information (occupation and education), 2 regarding income (personal income source and annual household income), 1 regarding family member numbers and 4 regarding eye-care accessibility and barriers to cataract surgery. The reliability and validity of the questionnaire was approved by statistical experts, and was tested in the pilot interview on 50 participants. Consistency of the same participant’s responses at different time points was checked on all questions and the α index is above 0.8. A trained nurse (HHF) surveyed 500 consecutive patients using the questionnaire at the initiation of this cataract screening program in January 2015 and again in January 2018. All data were entered into Microsoft Excel 2016 spreadsheets (Microsoft Corp., Redmond, Washington, USA), sorted and analyzed by two researchers (XHT and XZQ), and mutually checked. Double entry was conducted to avoid input errors.
Statistical analysis
Descriptive analysis was used to summarize the demographic information, economic and education status of the screening population, the cataract surgical output and outcome, the accessibility to eye-care service and barriers to cataract surgery. The CSRs of Zhaoqing area were calculated by dividing the total annual cataract surgical volume for the catchment area, as obtained from the local health bureau, by the area population. The Chi-squared test and ordinal logistic regression were used for categorical variables. Spearman correlation analysis was used to assess the relationship between the number of eye examination and education status or annual household income. A P value of <0.05 was considered to be statistically significant. Analysis of data was performed using SPSS 16.0 (SPSS Inc., Chicago, IL, USA).
Results
Demographic characteristics of participants
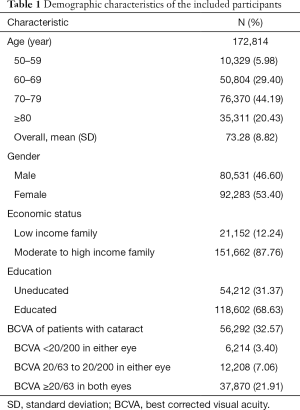
A total of 172,814 people aged ≥50 years from 135 towns and 1,385 villages in the Zhaoqing prefecture were screened. The participants’ distribution information is shown in Figure 1A. Participants in this study aged 50–119 years (73.28±8.82 years old), 92,283 (53.40%) were female, 21,152 (12.24%) were from low income families, and 54,212 (31.37%) were uneducated. The demographic characteristics of participants are listed in Table 1.
Full table
Output of cataract screening
In total, 56,292 (32.57%) people were diagnosed with age-related cataract, among whom 18,422 (10.66%) with BCVA less than 20/63 were recommended for cataract surgery. Cataract surgery was performed on 11,105 (60.28%) recommended patients (13,053 eyes), among whom 9,408 (84.72%) were from villages, 1,697 (15.28%) were from towns, and 1,001 (9.01%) were from low-income families. Cataract surgical coverage by person in this screening population is 60.28% for participants with BCVA <20/63.
In total, 18,860 cataract surgeries were performed in the Zhaoqing Minsheng Eye Hospital from January 1, 2015 to December 31, 2017, and the patients from this cataract screening program accounted for 69.21%. The percentage of cataract surgery patients from screening decreased from 2015 to 2017 (Figure 1B).
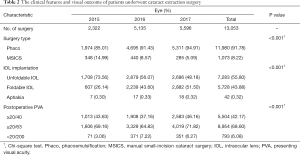
Outcome of cataract surgery
Among all the operated patients, 1,948 (17.54%) received bilateral surgery and 9,157 (82.46%) received unilateral surgery. Phacoemulsification was performed on 11,980 (91.78%) eyes, and 1,073 (8.22%) eyes received MSICS. Unfoldable IOLs were implanted in 7,283 (55.80%) eyes, and foldable IOLs were implanted in 5,728 (43.88%) eyes. Forty-two (0.32%) eyes did not receive IOL implantation because of operative complications or ocular comorbidities (Table 2). The percentage of phacoemulsification increased with time, while unfoldable IOLs remained the predominant intraocular implants in this rural area. A total of 8,954 (68.60%) eyes had a PVA of 20/63 or better and 5,504 (42.17%) had a PVA of 20/40 or better at 1 month after the surgery. In addition, 793 (6.08%) eyes had poor surgical outcome with a PVA of worse than 20/200 due to surgical complications or comorbidities (Table 2). The outcome of cataract surgery improved with time.
Full table
CSR
The CSR of the Zhaoqing area was 1,060/million/y, 1,018/million/y and 1,519/million/y in 2012, 2013 and 2014, respectively. However, it dramatically increased to 2,739/million/y (1.8 folds) in 2015, 3,678/million/y (2.4 folds) in 2016, and 3,654/million/y (2.4 folds) in 2017 after the implementation of this cataract screening model. Figure 1C shows the CSRs trends in Zhaoqing from 2010 to 2017.
Accessibility to eye-care service
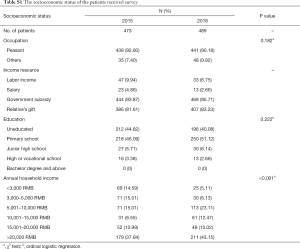
Among the 500 surveyed patients, 27 patients (5.40%) in 2015 and 11 patients (2.20%) in 2018 refused to respond or failed to understand the question, leaving 473 patients in 2015 and 489 patients in 2018 for statistical analysis. The socioeconomic status of patients who received questionnaire interview was listed in Table S1. There was no significant difference in the occupation or the education status of patients who received survey between 2015 and 2018 (P>0.05). The annual household income of patients who received survey in 2018 was higher than in 2015 (P<0.001) due to the increasing government subsidy in old people and the development of social economy in rural China.
Full table
The eye-care accessibility of surveyed patients is listed in Table 3. The results indicated that 262 (55.39%) patients did not receive any ophthalmic examinations in the past 5 years, and 243 (51.37%) patients were unaware of cataracts in 2015. After 3 years of screening, only 108 (22.09%) patients did not receive any ophthalmic examinations in the past 5 years, and 154 (31.49%) patients were unaware of cataracts in 2018. There was significant difference in the number of eye examination and the awareness of cataract between 2015 and 2018 (P<0.001). The correlation analysis showed that the number of eye examination in the past 5 years was positively correlated with the education status (R=0.174, P=0.032) and annual household income (R=0.190, P=0.019) in 2015. However, there were no correlation between the number of eye examination and education status (R=−0.047, P=0.488) or annual household income (R=−0.037, P=0.582) in 2018. The main cataract diagnosis site changed from county-lever hospital in 2015 to cataract screening site in 2018 (Table 3). The rate of cataract diagnosis during cataract screening increased from 18.69% in 2015 to 78.80% in 2018 (P<0.001).
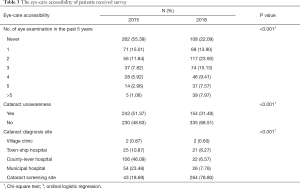
Full table
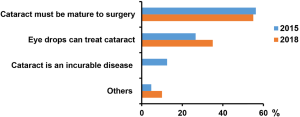
Barriers to cataract surgery
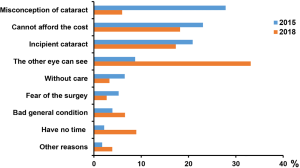
The main reason for not receiving cataract surgery changed from having misconception of cataract in 2015 to having good vision in the fellow eye in 2018 (Table 4 and Figure S1). There was significant difference in the reasons for not receiving cataract surgery between 2015 and 2018 (P<0.001). The misconception of cataract was classified in Table 4 and Figure S2.
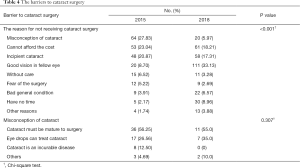
Full table
Discussion
Here, we for the first time reported the performance of a novel cataract screening model integrated into the project of resident health record by MOH. During the study period, 172,814 people aged ≥50 years were screened and cataract surgery was performed on 11,105 recommended patients (13,053 eyes), accounting for 69.21% of the three-year cataract surgery volume in Minsheng Eye Hospital. CSR of the Zhaoqing area dramatically increased by 1.8 folds in 2015 and 2.4 folds in 2016 and 2017 compared with that in 2014. These results showed that this screening model can effectively improve the screening efficiencies and surgical output.
WHO suggested that private eye-care services should be encouraged to be actively involved in cataract outreach program (26). However, the efficacy and approach of private hospital in screening cataract remain unclear. This study demonstrated that our model by incorporating private hospital to the MOH project increased the output of cataract surgery. The cataract surgical coverage by person was 60.28% for participants with BCVA <20/63 in our study, which was higher than the China Nine-Province Survey in 2014 (30.6%) and another study by Zhang et al. in the Chaonan region of south China (47.5%) (13,27). Besides the output, the surgery outcome is also an important performance indicator of cataract services (28). The visual outcomes of the patients were excellent and improved with time in this novel model. Percentage of patients who acquired PVA ≥20/63 was 68.60% and <20/200 was 6.08% at 1 month postoperatively in this program, which was better than previous reports (13,27-29). Therefore, the cataract screening model we reported is a successful case in which private eye-care service actively collaborates with the governmental health administration department to deliver high-quality, low-cost cataract surgical services in rural China.
Various barriers to cataract surgery in developing countries have been reported, including the unaffordable costs of surgery and IOL, misconceptions about cataract and treatment, fear of surgery, lack of eye-care infrastructure, long distances from surgical centers and lack of family support (19,20,27,30). The free transportation and low-priced unfoldable IOLs were provided in this screening program to address some barriers. Our questionnaire results showed that three years of widespread cataract screening integrated into establishment of resident health record appeared to be able to increase the accessibility to eye-care service and disseminate cataract knowledge in rural China. The main reason for not receiving cataract surgery changed from misconception of cataract in 2015 to having good vision in the fellow eye in 2018. Although the awareness of the cataract was improved, many patients still conceived that they did not need cataract surgery as long as the vision of the fellow eye was good. Therefore, it is necessary to further enhancing the eye disease education.
Increased surgical output and outcome were achieved in this cataract screening model in rural area of Zhaoqing prefecture. However, challenges remain. Firstly, due to the shortage of funds and manpower, the Minsheng Eye Hospital cannot take part in all the annual health screening in collaboration with the local health administration department. In the future, more eye-care services, including public and private hospitals, are expected to participate in this screening program. Secondly, the slit-lamp microscopy and fundoscopy are expected to be added into the resident health record as a required item in China in the future. Furthermore, the portable slit-lamp and fundoscopy should be equipped in the grass-roots hospitals and clinics. Thus, the leading causes of blindness and visual impairment, such as cataract, refraction error and retinal diseases, can be identified timely. Thirdly, the poor awareness of cataract and treatment is still one of the barriers of cataract surgery in rural China. Diversified eye disease education, such as lectures, consultation, phone-interviews and outreach screenings, should be further implemented. Fourth, it is important to improve the eye-care capacity for township and village doctors and to establish the screening and referral network in rural areas.
This study has limitations. Firstly, the inherent observational design prevented cause-inference. Secondly, only three years data were available. The long-term benefit of this novel model is needed for further validation. Thirdly, the study was performed in rural area in south China, and the generalization of the findings to other population such as Indians should be taken cautions.
Conclusions
In summary, this study documented the benefits of a novel cataract screening model integrated into establishment of resident health record in rural China, which may serve as a cost-effective, practicable and sustainable cataract screening model. This screening model could offer regional integrated collaborative service based on public health platform, solve information and service isolation problems, and save medical resources. This may be an optimal strategy to disseminate cataract knowledge and eliminate cataract blindness in rural areas and provide a successful model for other regions in China and other developing countries to increase the cataract surgical output.
Acknowledgments
Funding: This study is supported by the Construction Project of High-Level Hospitals in Guangdong Province (303020102) and the Medical Research Funds of Guangdong province (A2020086). We acknowledge the support and cooperation of colleagues at the Zhaoqing Minsheng Eye Hospital, without whom the study would have been impossible.
Footnote
Reporting Checklist: The authors have completed the MDAR checklist and STROBE reporting checklist. Available at http://dx.doi.org/10.21037/atm-20-396
Data Sharing Statement: Available at http://dx.doi.org/10.21037/atm-20-396
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/atm-20-396). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. This study was consistent with the tenets of the Declaration of Helsinki (as revised in 2013) and was approved by the ethics committee of Zhongshan Ophthalmic Center, Sun Yat-sen University and Zhaoqing Minsheng Eye Hospital (2014MEKY032). Oral informed consent was obtained from each participant (provision of written consent was exempted by the IRB-ZOC-SYSU).
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Bourne RRA, Flaxman SR, Braithwaite T, et al. Magnitude, temporal trends, and projections of the global prevalence of blindness and distance and near vision impairment: a systematic review and meta-analysis. Lancet Glob Health 2017;5:e888-e897. [Crossref] [PubMed]
- Khairallah M, Kahloun R, Bourne R, et al. Number of People Blind or Visually Impaired by Cataract Worldwide and in World Regions, 1990 to 2010. Invest Ophthalmol Vis Sci 2015;56:6762-9. [Crossref] [PubMed]
- Prokofyeva E, Wegener A, Zrenner E. Cataract prevalence and prevention in Europe: a literature review. Acta Ophthalmol 2013;91:395-405. [Crossref] [PubMed]
- Pascolini D, Mariotti SP. Global estimates of visual impairment: 2010. Br J Ophthalmol 2012;96:614-8. [Crossref] [PubMed]
- World Health Organization. Blindness: Vision 2020-The Global Initiative for the Elimination of Avoidable Blindness. Available online: http://www.who.int/mediacentre/factsheets/fs213/en/. Accessed March 1, 2019.
- Foster A. Cataract and "Vision 2020-the right to sight" initiative. Br J Ophthalmol 2001;85:635-7. [Crossref] [PubMed]
- World Health Organization. Universal eye health: a global action plan 2014–2019. Geneva, Switzerland: WHO; 2013. Available online: www.who.int/blindness/actionplan/en/. Accessed March 1, 2019.
- Zhao JL. To promote "Vision 2020" Initiative under the new situation in China. Zhonghua Yan Ke Za Zhi 2011;47:769-72. [PubMed]
- Gollogly HE, Hodge DO, St Sauver JL, et al. Increasing incidence of cataract surgery: population-based study. J Cataract Refract Surg 2013;39:1383-9. [Crossref] [PubMed]
- Behndig A, Montan P, Stenevi U, et al. One million cataract surgeries: Swedish National Cataract Register 1992-2009. J Cataract Refract Surg 2011;37:1539-45. [Crossref] [PubMed]
- Ackland P. The accomplishments of the global initiative VISION 2020: The Right to Sight and the focus for the next 8 years of the campaign. Indian J Ophthalmol 2012;60:380-6. [Crossref] [PubMed]
- Zhao JL. Review and outlook of the eye health in China. Zhonghua Yan Ke Za Zhi 2018;54:561-4. [PubMed]
- Zhao J, Xu X, Ellwein LB, et al. Cataract Surgical Coverage and Visual Acuity Outcomes in Rural China in 2014 and Comparisons With the 2006 China Nine-Province Survey. Am J Ophthalmol 2018;193:62-70. [Crossref] [PubMed]
- Zhu M, Zhu J, Lu L, et al. Four-year analysis of cataract surgery rates in Shanghai, China: a retrospective cross-sectional study. BMC Ophthalmol 2014;14:3. [Crossref] [PubMed]
- Yan X, Congdon N, He M. Prevention of Cataract Blindness in Rural China. Asia Pac J Ophthalmol (Phila) 2012;1:69-71. [Crossref] [PubMed]
- Chen T, Jin L, Zhou Z, et al. Factors influencing the output of rural cataract surgical facilities in China: the SHARP study. Invest Ophthalmol Vis Sci 2015;56:1283-91. [Crossref] [PubMed]
- Congdon NG, He M. Screening and managing eye disease in 2010: an Asian perspective. Am J Ophthalmol 2010;150:141-3. [Crossref] [PubMed]
- Zhang M, Wu J, Li L, et al. Impact of cataract screening outreach in rural China. Invest Ophthalmol Vis Sci 2010;51:110-4. [Crossref] [PubMed]
- He M, Chan V, Baruwa E, et al. Willingness to pay for cataract surgery in rural Southern China. Ophthalmology 2007;114:411-6. [Crossref] [PubMed]
- Zhang XJ, Liang YB, Liu YP, et al. Implementation of a free cataract surgery program in rural China: a community-based randomized interventional study. Ophthalmology 2013;120:260-5. [Crossref] [PubMed]
- Xu J, Zhu S, Li S, et al. Models for improving cataract surgical rates in southern China. Br J Ophthalmol 2002;86:723-4. [Crossref] [PubMed]
- Ko F, Frick KD, Tzu J, et al. Willingness to pay for potential enhancements to a low-cost cataract surgical package in rural southern China. Acta Ophthalmol 2012;90:e54-60. [Crossref] [PubMed]
- Chinese Ministry of Health. Guidance on standardizing the management of health records of urban and rural residents. Issued December 1, 2009.
- Statistical Bureau of Guangdong Province. Statistical bulletin on national economic and social development of Guangdong Province in 2018. Available online: http://stats.gd.gov.cn/tjgb/content/post_2207563.html. Accessed March 1, 2019.
- People's Government of Zhaoqing Municipality. Statistical bulletin on national economic and social development of Zhaoqing in 2018. Available online: http://zwgk.zhaoqing.gov.cn/zq128/201904/t20190423_945443.html. Accessed March 1, 2019.
- World Health Organization. Programme for the Prevention of Blindness and Deafness. 2000. Global Initiative for the Elimination of Avoidable Blindness. Available online: https://apps.who.int/iris/handle/10665/63748. Accessed March 1, 2019.
- Zhang X, Li EY, Leung CK, et al. Prevalence of visual impairment and outcomes of cataract surgery in Chaonan, South China. PLoS One 2017;12:e0180769. [Crossref] [PubMed]
- Zhao J, Ellwein LB, Cui H, et al. Prevalence and outcomes of cataract surgery in rural China the China nine-province survey. Ophthalmology 2010;117:2120-8. [Crossref] [PubMed]
- Wu M, Yip JL, Kuper H. Rapid assessment of avoidable blindness in Kunming, china. Ophthalmology 2008;115:969-74. [Crossref] [PubMed]
- Yin Q, Hu A, Liang Y, et al. A two-site, population-based study of barriers to cataract surgery in rural china. Invest Ophthalmol Vis Sci 2009;50:1069-75. [Crossref] [PubMed]


