
Intracytoplasmic sperm injection outcomes in patients with orgasmic dysfunction and anejaculation by percutaneous epididymal sperm aspiration (PESA)
Introduction
Ejaculation is a complex process accomplished by a synergy of sensory receptors, afferent pathways, cerebral sensory/motor areas, and efferent pathways. Ejaculatory disorders include orgasmic dysfunction, anejaculation, retrograde ejaculation, premature ejaculation, and delayed ejaculation (1). The etiology of ejaculatory disorders is complex and not completely understood. Orgasmic dysfunction refers to the difficult or absent orgasm after sufficient sexual stimulation, while anejaculation is the failure of antegrade or retrograde ejaculation during orgasm (1).
Orgasmic dysfunction and anejaculation can be treated with prostate massage, penile vibratory stimulation (PVS), rectal electrical stimulation, and surgical sperm retrieval to obtain sperm for assisted reproduction (2). Prostate massage and PVS are only effective in achieving ejaculation in a minority of patients (3-5). Electroejaculation (EEJ) can realize successful sperm retrieval in 90% of patients, but the quality of semen gathered from this method is often poor (6-9). Through surgical sperm retrieval, a relatively large quantity and high quality of sperm can be easily retrieved from the epididymis and used for intracytoplasmic sperm injection (ICSI) (10).
However, few studies have reported the outcomes of ICSI in patients undergoing percutaneous epididymal sperm aspiration (PESA) for severe orgasmic dysfunction or anejaculation. Our study aimed to analyze ICSI outcomes using sperm collected via PESA. To compare the ICSI outcomes of epididymal sperm, we established a control group containing patients with congenital bilateral absence of the vas deferens (CBAVD) who underwent PESA. For these patients, spermatozoa can only be obtained from the epididymis or testis. Sub-group analyses of patients with severe ejaculatory disorders (orgasmic dysfunction and anejaculation, frozen and fresh epididymal sperm, diabetic, and non-diabetic) were also conducted. We present the following article following the Strengthening The Reporting of Observational Studies in Epidemiology (STROBE) reporting checklist (available at http://dx.doi.org/10.21037/atm-20-1121a).
Methods
Patients
We retrospectively analyzed patients with orgasmic dysfunction and anejaculation who had received surgical sperm retrieval for ICSI between January 2013 and December 2018 in the Reproductive Medicine Center, the First Affiliated Hospital of Nanjing Medical University. Variables included in our analysis were male age, female age, metaphase II (MII) oocytes, fertilization rate (2PN), good embryos rate, clinical pregnancy rate, early pregnancy loss, and live birth rate. The clinical pregnancy rate, early pregnancy loss, and live birth rate of only the first fresh embryo transfer were included for statistics. The ICSI outcomes of CBAVD were set as control. The study was conducted following the tenets of the Declaration of Helsinki (as revised in 2013). The ethics committee of the First Affiliated Hospital of Nanjing Medical University approved this study (No. 2019-SR-128) and informed consent was taken from all the patients.
Exclusion criteria included the inability to reach orgasm via vaginal intercourse with ability via masturbation, and drug-related ejaculatory disorders (e.g., antipsychotics and antidepressants). An experienced male urologist evaluated all patients with a detailed case history, physical examination, and laboratory testing (e.g., post-ejaculatory urinalysis, hormone evaluation, fasting blood glucose, and transrectal ultrasonography). Only patients with a normal range of sex hormone levels, especially testosterone, prolactin, and follicle-stimulating hormone, were included. All participants and their partners were informed of the potential risks (pain, bleeding, and infection) of PESA, testicular sperm aspiration (TESA), and ICSI.
Retrieval techniques
Either PESA or TESA was performed under local anesthesia by the same surgeon (Yang XY). All patients received a spermatic cord block with 1% lidocaine hydrochloride injection, typically 5 mL was injected into the spermatic cord. After fixing the caput or cauda of the epididymis with the fingers, a 5.5 mm angiocatheter needle was directed through the skin into the caput or cauda of the epididymis. The needle was withdrawn, and the angiocatheter was retained in place. Next, a 10 mL syringe containing 1 mL of sperm buffer was attached to the angiocatheter. Negative pressure was created, and the angiocatheter was gently withdrawn and then pushed back into the caput or cauda epididymis until epididymal fluid appeared in the angiocatheter needle. The specimen was immediately examined under the microscope to confirm the presence of spermatozoa. If no spermatozoa were found, the same procedure was performed on the contralateral side. If no spermatozoa were retrieved from the second side, TESA was performed (11). Under a 400× phase-contrast microscope, 10 µL of epididymal fluid containing culture (0.5–1 mL) was dropped onto slides for analysis. If more than one progressively motile sperm could be observed in 10 visual fields, freezing was applicable; if one progressively motile sperm could be seen on the whole slide, the sperm would meet the ICSI standard.
Stimulation, ICSI, embryo culture, and pregnancy
Routine stimulation was adopted according to the patients’ partners’ case requirements. Transvaginal ultrasound was used to monitor the follicles continuously. Oocyte maturation was triggered by human chorionic gonadotropin (hCG) 5,000–7,500 IU or gonadotropin-releasing hormone agonist (GnRHa) 0.2 mg. Oocytes were retrieved 34–36 h later by vaginal ultrasound-guided follicular puncture. The conduction of ICSI, embryo culture, embryo transfer, embryo cryopreservation, and assessment were as previously described (12). Fresh embryo freezing or transfer was performed 3 or 5 days after fertilization. Whole embryo cryopreservation was carried out when the risk of ovarian hyperstimulation was high, and when the endometrium (thickness <7 mm) was not suitable for transplantation (13). Routine progesterone was given, and β-hCG was tested 2 weeks later to assess the pregnancy outcome. Clinical pregnancy was defined as a gestational sac with or without a fetal heartbeat, early pregnancy loss as spontaneous abortion within 12 weeks of gestation, and live birth as the number of live birth events (>24 weeks gestation).
Statistical analysis
Data were analyzed and expressed as mean ± SD using SPSS version 18.0 (IBM Corp., USA). The independent t-test or nonparametric test was used for comparisons between groups. To compare proportions between two groups (fertilization, transferable embryo rate, high-quality embryo rate, early pregnancy loss, clinical pregnancy, and live birth rates), the chi-square (χ2) test or Fisher’s exact test was used. Statistical significance was considered as P<0.05.
Results
Among the 96 participants with severe ejaculatory disorders, the majority were idiopathic, and 41 had orgasmic dysfunction, including 36 cases of primary and 5 cases of secondary dysfunction. There was 1 case of orgasmic disorder secondary to severe brain injury. Right cryptorchidism orchiopexy had been performed during preadolescence on 2 of the participants with adult orgasmic dysfunction, but the causal relationship could not be confirmed.
Among the 55 patients with anejaculation, 11 presented idiopathically and 44 with clear etiology, including diabetes mellitus (DM) (n=28), paraplegia (n=4), pelvic surgery (n=6), postoperative pituitary adenoma (n=2), congenital bilateral absence of the vas deferens (n=2), multiple sclerosis (n=1), and genitourinary tuberculosis (n=1). The sexual hormone levels of the 2 cases with postoperative pituitary adenoma had been normal for more than six months.
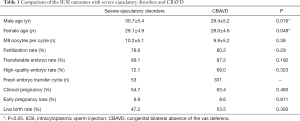
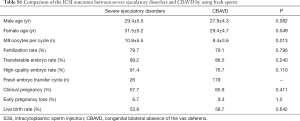
Of the 96 participants with severe ejaculatory disorders, 91 (94.8%) underwent PESA and ICSI. Of these 91 patients, sperm could be obtained from the cauda of the epididymis by PESA in 90 patients, and the caput of the epididymis in 1 patient. Compared to the CBAVD control group, no statistical difference was observed in MII oocytes (10.2±5.1 vs. 9.8±5.2, P=0.38), fertilization rate (78.6% vs. 80.2%, P=0.29), transferable embryo rate (89.1% vs. 87.2%, P=0.192), or high-quality embryo rate (72.1% vs. 69.0%, P=0.38). Age comparison with the control group showed statistical significance (male 30.7±5.4 vs. 29.4±5.2, P=0.016, female 29.1±4.9 vs. 28.0±4.6, P=0.048). We then compared the pregnancy rate of fresh embryo transfer between the two groups. No statistical difference was observed in the clinical pregnancy rate (54.7% vs. 63.4%, P=0.483), early pregnancy loss (6.9% vs. 8.6%, P=0.811), or live birth rate (47.2 vs. 53.5, P=0.393) (Table 1).
Full table
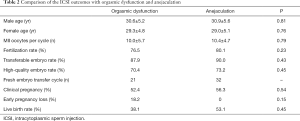
The outcomes of PESA and ICSI were further compared between participants with orgasmic dysfunction and anejaculation. No between-group difference was observed neither in age, nor in MII oocytes (10.0±5.7 vs. 10.4±4.7, P=0.43), fertilization rate (76.5% vs. 80.1%, P=0.23), transferable embryo rate (87.9% vs. 90.0%, P=0.43), high-quality embryo rate (70.4% vs. 73.2%, P=0.45), clinical pregnancy rate (52.4% vs. 56.3%, P=0.54), and live birth rate (38.1% vs. 53.1%, P=0.45) (P>0.05) (Table 2).
Full table
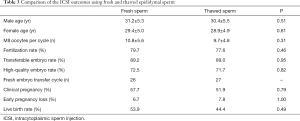
The outcomes of PESA and ICSI using fresh and thawed sperm were compared. Similar to what was observed above, no statistical differences were observed in MII oocytes per cycle (10.8±5.6 vs. 9.7±4.8, P=0.31), fertilization rate (79.7% vs. 77.6%, P=0.46), transferable embryo rate (89.2% vs. 89.0%, P=0.95), high-quality embryo rate (72.5% vs. 71.7%, P=0.82), clinical pregnancy rate (57.7% vs. 51.9%, P=0.79), the spontaneous abortion rate (6.7% vs. 7.8%, P=1.0), and live birth rate (53.9% vs. 44.4%, P=0.49) (Table 3).
Full table
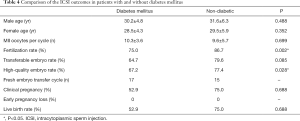
Of the patients receiving PESA and ICSI for anejaculation, 28 cases showed DM (diabetic group), and the other 25 cases were non-diabetic (non-diabetic group); we also compared the ICSI outcomes between these two groups. No statistical difference was observed in the couple ages, nor in MII oocytes (10.3±3.6 vs. 9.6±5.7, P=0.699), transferrable embryo rate (64.7% vs. 79.6%, P=0.085), high-quality embryo rate (50.4% vs. 77.4%, P=0.028), clinical pregnancy rate (52.9% vs. 75.0%, P=0.688), or live birth rate (52.9% vs. 75.0%, P=0.688). However, the fertilization rate and high-quality embryo rate in DM patients were lower than those in patients without DM (75.0% vs. 86.7%, P=0.002; 50.4% vs. 77.4%, P=0.028, respectively) (Table 4).
Full table
Discussion
Orgasmic dysfunction and anejaculation are two uncommon but powerful factors of male infertility. Ejaculatory disorders may be caused by congenital, endocrine, medicinal, and neurogenic or psychological factors. However, the exact cause of some ejaculatory disorders, especially orgasmic dysfunction, is not clear, which poses a great challenge to the treatment.
Orgasmic dysfunction and anejaculation can be treated through psychological counseling, pharmacotherapy (levodopa and ephedrine), PVS, and EEJ (14). In patients with ejaculatory disorders, PVS can be used for the retrieval of semen as it is less invasive than EEJ and surgical sperm retrieval, but it may not be effective for all patients (15). Patients with anejaculation caused by a spinal cord injury or orgasmic dysfunction can provide semen through EEJ, but spermatozoa with low motility are not optimal for assisted reproductive technology (16). Surgical sperm retrieval, by either PESA or TESA, can be used as an alternative in patients with severe ejaculatory disorders, or when PVS and EEJ have previously been unsuccessful (17).
The invention of ICSI was first reported by Palermo et al. in 1992, and concurrently new treatment options for severe ejaculatory disorders emerged, namely PESA or TESA (18). The spermatozoa collected by PESA are more motile than those retrieved by TESA, and laboratory processing of epididymal sperm is easier than that of testicular sperm. Furthermore, Shih et al. reported that TESA and PESA yielded similar pregnancy and miscarriage rates (19). For these reasons, we believe that PESA, like TESA, is an appropriate and convenient way to obtain sperm for ICSI in cases of patients with orgasmic dysfunction and anejaculation.
In the present study, the clinical pregnancy rate of PESA-based ICSI was 54.7% (28/53) in the fresh embryo transfer cycle (53 of 91). There was one case of ectopic gestation and two cases of spontaneous abortion, which meant the live birth rate was 47.2% (25/53). These results are similar to those reported by Soeterik et al. (16). Compared to the CBAVD group, sperm from the epididymis achieved similar clinical pregnancy and live birth rates in ICSI using either fresh or frozen sperm (Tables S1 and S2). In the subgroup analysis, no statistical difference was observed in fertilization rate, transferrable embryo rate, high-quality embryo rate, clinical pregnancy rate, and live birth rate (P>0.05). Frozen and fresh epididymal sperm achieved similar outcomes, which is consistent with the results reported previously (20,21).
Full table

Full table
Among the 55 anejaculation patients, 28 patients (50.9%) showed DM, a progressive condition that requires close attention. There are an estimated 113.9 million adults with DM in China, and this number is expected to increase with time (22-24). Neuropathy is most commonly caused by DM (25), and diabetic neuropathy may impair reproductive function in males. Agbaje et al. reported that the rate of sperm apoptosis and the damage of spermatozoon ultrastructure were more obvious in diabetic patients than in healthy males (26). In this study, the fertilization rate and high-quality embryo rate of patients with DM were lower than those in non-diabetic patients.
Other causes of anejaculation include paraplegia, extirpative pelvic surgery, postoperative pituitary adenoma, multiple sclerosis, and genitourinary tuberculosis. In paraplegic patients, PVS could be used to induce ejaculation because of the integrity of the reflex arc in the spinal cord. In patients with spinal cord injury above T10, the stimulation may achieve a better result than in those with cord injury in the lower levels. In EEJ, rectal electrodes are used to stimulate the peripheral nerves of the prostate to induce ejaculation, but anesthesia is required, and rectal injury may occur as a consequence. The success rate of EEJ was more than 90%, but one-third of them required ICSI on account of poor sperm quality (16).
Compared with EEJ, PESA is more manipulatable. In the absence of ejaculation, spermatozoa accumulate in the epididymis, especially in the area of the cauda. Logically, the cauda epididymis is often chosen as the puncture site for patients with orgasmic dysfunction and anejaculation. Puncture of the vas deferens has previously been used for retrieving sperm (27); however, the vas deferens is relatively hard, and piercing it requires specialized needles.
Our study had some limitations that should be noted, with a small sample size being the first obvious constraint. The second is the lack of appropriate control groups involving electro-ejaculated sperm, testicular sperm, or penile vibratory stimulation sperm. Additionally, the retrospective nature of the study may have also restricted the quality and richness of the data.
In conclusion, PESA, like TESA, is an appropriate and convenient way to obtain sperm for ICSI for patients with orgasmic dysfunction and anejaculation. Using sperm from the cauda epididymis, ICSI can achieve favorable clinical pregnancy and live birth rates in patients with orgasmic dysfunction and anejaculation.
Acknowledgments
Funding: This study was supported by the National Natural Science Foundation of China (81971374, 81370754) and a project of State Key Laboratory of Reproductive Medicine China (SKLRM-KA201703).
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at http://dx.doi.org/10.21037/atm-20-1121a
Data Sharing Statement: Available at http://dx.doi.org/10.21037/atm-20-1121a
Peer Review File: Available at http://dx.doi.org/10.21037/atm-20-1121a
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/atm-20-1121a). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The ethics committee of the First Affiliated Hospital of Nanjing Medical University has approved this study (No. 2019-SR-128) and informed consent was taken from all the patients.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Colpi G, Weidner W, Jungwirth A, et al. EAU Working Party on Male Infertility. EAU guidelines on ejaculatory dysfunction. Eur Urol 2004;46:555-8. [Crossref] [PubMed]
- Dohle GR, Colpi GM, Hargreave TB, et al. EAU guidelines on male infertility. Eur Urol 2005;48:703-11. [Crossref] [PubMed]
- Castle SM, Jenkins LC, Ibrahim E, et al. Safety and efficacy of a new device for inducing ejaculation in men with spinal cord injuries. Spinal Cord 2014;52:S27-9. [Crossref] [PubMed]
- Brackett NL, Ferrell SM, Aballa TC, et al. An analysis of 653 trials of penile vibratory stimulation in men with spinal cord injury. J Urol 1998;159:1931-4. [Crossref] [PubMed]
- Sønksen J, Biering-Sorensen F, Kristensen JK. Ejaculation induced by penile vibratory stimulation in menwith spinal cord injuries. The importance of the vibratory amplitude. Paraplegia 1994;32:651-60. [PubMed]
- Gat I, Maman E, Yerushalmi G, et al. Electroejaculation combined with intracytoplasmic sperm injection in patients with psychogenic anejaculation yields comparable results to patients with spinal cord injuries. Fertil Steril 2012;97:1056-60. [Crossref] [PubMed]
- Fan LCH, Liu H. Penile Vibratory stimulation and electroejaculation in the treatment of ejaculatory dysfunction . Zhonghua Nan Ke Xue 2005;11:219-22. [PubMed]
- Schatte EC, Orejuela FJ, Lipshultz LI, et al. Treatment of infertility due to anejaculation in the male with electroejaculation and intracytoplasmic sperm injection. J Urol 2000;163:1717-20. [Crossref] [PubMed]
- Hovav Y, Shotland Y, Yaffe H, et al. Electroejaculation and assisted fertility in men with psychogenicanejaculation. Fertil Steril 1996;66:620-3. [Crossref] [PubMed]
- Fode M, Ohl DA, Sønksen J. A step-wise approach to sperm retrieval in men with neurogenic anejaculation. Nat Rev Urol 2015;12:607-16. [Crossref] [PubMed]
- Iwahata T, Shin T, Shimomura Y, et al. Testicular sperm extraction for patients with spinal cord injury-related anejaculation: A single-center experience. Int J Urol 2016;23:1024-7. [Crossref] [PubMed]
- Wu W, Zhou ZM, Lin M, et al. Ychromosome microdeletions do not affect the outcomes of ICSI for infertile males. Zhonghua Nan Ke Xue 2011;17:771-4. [PubMed]
- Shu L, Xu Q, Meng Q, et al. Clinical outcomes following long GnRHa ovarian stimulation with highly purified human menopausal gonadotropin plus rFSH or rFSH in patients undergoing in vitro fertilization-embryo transfer: a multi-center randomized controlled trial. Ann Transl Med 2019;7:146. [Crossref] [PubMed]
- Mehta A, Sigman M. Management of the dry ejaculate: a systematic review of aspermia and retrograde jaculation. Fertil Steril 2015;104:1074-81. [Crossref] [PubMed]
- Soeterik TF, Veenboer PW, Lock TM. Electroejaculation in psychogenic anejaculation. Fertil Steril 2014;101:1604-8. [Crossref] [PubMed]
- Soeterik TF, Veenboer PW, Oude-Ophuis RJ, et al. Electroejaculation in patients with spinal cord injuries: A 21-year, single-center experience. Int J Urol 2017;24:157-61. [Crossref] [PubMed]
- Raviv G, Madgar I, Elizur S, et al. Testicular sperm retrieval and intra cytoplasmic sperm injection provide favorable outcome in spinal cord injury patients, failing conservative reproductive treatment. Spinal Cord 2013;51:642-44. [Crossref] [PubMed]
- Palermo G, Joris H, Devroey P, et al. Pregnancies after intracytoplasmic injection of single spermatozoon into an oocyte. Lancet 1992;340:17-8. [Crossref] [PubMed]
- Shih KW, Shen PY, Wu CC, et al. Testicular versus percutaneous epididymal sperm aspiration for patients with obstructive azoospermia: a systematic review and meta-analysis. Transl Androl Urol 2019;8:631-40. [Crossref] [PubMed]
- Ishikawa T, Shiotani M, Izumi Y, et al. Fertilization and pregnancy using cryopreserved testicular sperm for intracytoplasmic sperm injection with azoospermia. Fertil Steril 2009;92:174-9. [Crossref] [PubMed]
- Sun Y, Teng XM, Li WP, et al. Fertilization and pregnancy outcome with intracytoplasmic sperm injection using ejaculate sperm, surgically retrieved sperm and frozen-thawed sperm. Reprod Contracept 2006;26:294-8.
- International Diabetes Federation. IDF Dabetes Atlas. December 6, 2019; 9th Edition. Available online: http://www.diabetesatlas.org/.
- Xu Y, Wang L, He J, et al. Prevalence and control of diabetes in Chinese adults. JAMA 2013;310:948-59. [Crossref] [PubMed]
- Shih KC, Lam KS, Tong L. A systematic review on the impact of diabetes mellitus on the ocular surface. Nutr Diabetes 2017;7:e251. [Crossref] [PubMed]
- National prevention and control plan of diabetes mellitus in China. Chinese J Prevention and Control of Chronic Dieases 1996;4:49-50.
- Agbaje IM, Rogers DA, McVicar CM, et al. Insulin dependant diabetes mellitus: implications for male reproductive function. Hum Reprod 2007;22:1871-7. [Crossref] [PubMed]
- Shin DH, Turek PJ. Sperm retrieval techniques. Nat Rev Urol 2013;10:723-30. [Crossref] [PubMed]


