
An interventional implementation project: hand hygiene improvement
Introduction
Healthcare-associated infections (HAIs) are associated with significant morbidity and mortality as well as increased medical costs (1). However, HAIs are preventable. Hand hygiene is a fundamental prevention strategy (2,3) and the cornerstone of infection prevention. A considerable number of studies have focused on reducing the incidence of HAIs by improving hand hygiene compliance among healthcare professionals (4-11). Studies have revealed a low level of hand hygiene compliance among HCWs (12); the rates of hand hygiene compliance have consistently been reported to be 50% for HCWs and 20% for the public (13). This study aimed to evaluate the efforts of a general teaching hospital in Zhejiang, China, to improve the compliance rate of hand hygiene among its staff. The project was implemented through planning, implementation, summary, and evaluation, as well as other measures to improve hand hygiene among the hospital staff, prevent and reduce the occurrence of hospital-acquired infections, enhance patient rehabilitation, and ensure the quality safety of medical care.
Hand hygiene alone can significantly reduce the risk of cross-transmission of infection in healthcare facilities (HCFs) (11,14,15). The results of hand hygiene monitoring previously carried out by the teaching hospital in our study were not significant. Since 2017, all staff at the hospital have participated in a hand hygiene project to improve the compliance rate of hand hygiene and, through this, improve the quality and safety of medical care. The first phase of the project included facility improvement, training, and baseline data collection. A monitoring software system was adjusted, and employees of all departments were encouraged to log in to the system and input hand hygiene-related data. Additionally, hand hygiene supplies and hand washing facilities were checked to ensure they were sufficient and complete. In line with the hand hygiene guidelines issued by the World Health Organisation (WHO) in 2009, the WHO hand hygiene questionnaire and five hand hygiene time points were adopted to unify the investigation methods being utilized across the entire hospital in order to facilitate improved hand hygiene knowledge and the training of hand hygiene investigators in various departments. The investigators randomly observed the hand hygiene practices of staff, entered the investigation data into the system, and established baseline data.
In the second and third phases, various planned improvement measures were continuously implemented. The investigators in various departments strengthened supervision and inspection, and published data for each department to be known to the entire staff. The hospital’s infection prevention and control department strengthened its efforts with supervision and inspection by conducting random spot checks and unannounced visits. In addition, training lectures were held, awareness posters were displayed, and feedback on hand hygiene data from across the hospital was published regularly to encourage employees’ active participation and implementation.
In the third phase of the project, communication was conducted with the relevant management departments to incorporate hand hygiene assessment into the department’s quality control inspection and employee assessment. Annual education and training plans of the hospital management department will include hand hygiene. Improving hand hygiene requires multi-department assistance and joint management.
We present the following article in accordance with the MDAR reporting checklist (available at http://dx.doi.org/10.21037/atm-20-5480).
Methods
Study design
In 2017, the 2,500-bed First Affiliated Hospital of College Medicine, Zhejiang University, in Hangzhou, China, introduced a longitudinal single-centre hand hygiene improvement project with repeated measurements. The project involves all hospital employees, including doctors, nurses, interns, and other workers.
Samples and ethical considerations
The hand hygiene improvement project involved the entire hospital staff. The research participants comprised over 5,000 doctors, nurses, workers, interns, and managers. The study adhered to the guidelines of China’s National Measures for Ethical Review of Biomedical Research Involving Humans (issued in 2007). Because the study focused on hospital HCWs, approval from the local ethics committee or written informed consent from the participants before the study was not necessary. The study complied with the ethical principles of the Declaration of Helsinki, as amended in 2013.
Specific intervention and study protocol
The intervention was carried out in three phases. The first phase involved facility preparation and the collection of baseline information. The second and third phases saw the implementation and continuous improvement of the measures. The project plan was devised according to the five factors of systematic evaluation: (I) make a plan and carry out evaluation. The target of evaluation is to ensure an ideal plan and basic practical measures, such as ensuring there are sufficient hand hygiene products and software monitoring. are in place to achieve effective intervention. (II) Regularly supervise and inspect the participation of the personnel in the plan’s implementation. (III) Periodically report on the outcome and quality evaluation of the intervention. (IV) Regularly check employees’ awareness of the project and investigate their ability to participate and respond. (V) Determine the evaluation elements of the improvement project: education and training, supervision and feedback, and the management system. The WHO-specified model was adopted. The main evaluation index in this study was data on changes in the hand hygiene compliance rate.
Statistical analysis
SPSS version 19.0 for Windows (SPSS Inc., Chicago, IL, USA) was used to analyze the hand hygiene compliance rates of different professionals during different research periods. Hand hygiene methods include hand washing in seven step or using quick drying disinfectant as well. The data were obtained in various departments at different time points through random investigation and observation, at times during the day when hand hygiene is required. P<0.05 was considered to be statistically significant.
Results
Hand hygiene during different time periods (phase I, phase II, and phase III)
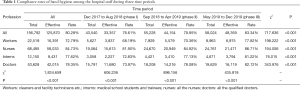
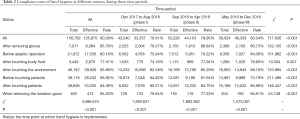
Differences in the compliance rates of hand hygiene among the staff during the three phases of the project were compared. The hand hygiene compliance rates for phases I, II, and III were 76.61%, 79.95%, and 83.34%, respectively (see Tables 1 and 2). The results showed that through continuous intervention, the compliance rate of hand hygiene gradually increased with time (P<0.001).
Full table
Full table
Hand hygiene for different professions
The compliance rates of hand hygiene among different professions were compared. The participants were classified into the following categories: doctors, nurses, other hospital workers, and interns. The results showed that nurses had the highest rate of compliance with hand hygiene, while workers had the lowest. The compliance rates of hand hygiene for the different professions were 84.73% for nurses, 78.35% for doctors, 77.62% for interns, and 72.79% for workers (Table 1).
At each period, the compliance rates of hand hygiene were significantly different between the different professions (P<0.001, the compliance rate of hand hygiene for nurses was the highest and lowest for the workers).
Hand hygiene for different statuses
The hand hygiene compliance rates were compared at different time points. The results showed that hand hygiene was practiced at the following time points (from high to low): after contact with the surrounding environment, such as the patient’s bedside table (85.86%); after removing gloves (85.76%); before and after putting on and removing the isolation gown (85.30%); after contact with patients (84.06%); before aseptic operation (80.18%); after contact with blood or body fluids (77.41%); and before contact with patients (68.82%) (Table 2).
Discussion
For the hand hygiene improvement project, we referred to the five descriptive factors for the systematic evaluation of interventional measures to formulate the implementation plan. Ensuring fidelity is crucial because it allows for the replication, evaluation, comparison, and dissemination of interventions (16-18). Implementation fidelity of an intervention has five domains: (I) adherence to the program; (II) exposure or dose (i.e., the proportion of the programme delivered); (III) quality of intervention delivery; (IV) participant responsiveness; and (V) program differentiation (i.e., the presence of distinguishing features of the intervention).
Formulating a detailed hand hygiene implementation improvement plan
The hospital management meeting agreed that “improving the compliance rate of hand hygiene among staff” through a hospital-wide improvement project should be included in the hospital quality management monitoring indicators and medical safety management system. The hospital’s infection prevention and control (IPC) department is responsible for the management of the hand hygiene project. Detailed plans were established and special personnel were assigned to take charge of the project’s management. The quality management plan-do-check act (PDCA) procedures were implemented continuously. Hand hygiene awareness was promoted in the hospital, hand hygiene facilities were improved, staff hand hygiene knowledge training was enhanced, regular inspections were carried out, inspection data were published, and the hand hygiene situation was regularly reported to the hospital management.
Supervising and inspecting the implementation of good practice in hand hygiene in each department
Part-time infection control personnel implemented the specific work in different departments. The hospital has more than 80 wards, and every department has part-time infection control personnel. The IPC carried out centralized hand hygiene investigation training for infection control personnel, familiarized and unified hand hygiene investigation methods, and conducted field investigation training for small groups. The infection control personnel were capable of obtaining more than 90% consistent investigation results. After completing the training, the part-time infection control personnel carried out random investigations in the departments. The investigations were conducted as follows. The WHO hand hygiene investigation record form (according to the five time points of hand hygiene) was adopted for random hand hygiene investigations in each department. The results were uploaded to the software system, which meant that the hospital could monitor all data. The part-time infection control personnel were also responsible for overseeing knowledge training in their wards. Knowledge training should cover all individuals in the ward, including doctors, nurses, workers, medical students and interns, family members, and patient attendants. The training content was uniformly provided via the hospital intranet. The IPC could check and evaluate the staff at any time during the inspection.
Timely intervention outcomes and quality of delivery were regularly published and reported to the entire hospital
The IPC could check the implementation status of each department using the monitoring software system at any time to remind departments that had not completed the investigation on time. The hand hygiene situation throughout the hospital was analyzed quarterly. The report forms were published on the hospital’s intranet and reported to the hospital management. Meanwhile, regular spot checks and unannounced visits were regularly conducted to check that hand hygiene was being implemented. If the hand hygiene results of an unannounced visit were significantly lower than those reported, the monitoring frequency would be increased for the department. Each department produced quarterly self-evaluation and summary reports. The improvement outcomes were discussed in the department meeting to make it known to the staff on the ward.
Participant responsiveness
The hospital’s senior management decided that all staff should participate in the hand hygiene improvement project and that the project should be permanently implemented. To ensure that all employees were aware and actively participating in the project: the hospital quality safety meetings should regularly report hand hygiene conditions; hand hygiene awareness should be promoted through various means; hand hygiene should be included in the training of new employees, the assessment of tutors and interns in the teaching hospital, and the management and assessment of interns to effectively facilitate awareness of and participation in good hand hygiene practice across the entire hospital; part-time IPC personnel of each department should clearly announce their hand hygiene results monthly, and each department should carry out continuous quality improvement; and the IPC personnel should use the inspection and spot checks to check the hand hygiene awareness of department staff and enquire about their degree of active participation.
Program differentiation
Implementation of this project included a detailed plan, including implementation measures, methods of evaluation, and feedback. Specialised management departments and persons-in-charge and a hospital supervision and management system were used. The project also adhered to the WHO hand hygiene investigation method model standards, and the quality management PDCA improvement procedures were also followed. Timely evaluation of the effect and quality of hand hygiene was performed.
We carried out online questionnaire survey to evaluate the relevant importance of each improvement measure. By using Likert 5-level score method, the questionnaire assigns the score of 5, 4, 3, 2 and 1 respectively to the options of very important, important, generally important, less important, unimportant. Scores greater than or equal to 3 are counted in the recognition rate of each improvement measure. We received 70 feedback questionnaires. The questionnaire consists of two parts. In the first part of the five factors of systematic evaluation, the average score of the five factors is 4.457 and the recognition rates were all 100%. According to the score, the five factors from high to low are (I) make a plan and carry out evaluation, (II) supervise and inspect, (III) regularly check employees’ awareness of the project and investigate their ability to participate and respond, (IV) determine the evaluation elements of the improvement project, (V) periodically report on the outcome and quality evaluation of the intervention. The scores were 4.529, 4.486, 4.471, 4.414, 4.386 respectively. The second part evaluated 15 improvement measures, with an average score of 4.617 and an average recognition rate of 99.52%. The 6 measures with the greatest score in order were: (I) enough hand hygiene products such as hand sanitizer and disposable paper towels (4.871, 100%), (II) adequate quick drying hand disinfectant (4.843, 100%), (III) hand hygiene knowledge training (4.786, 100%), (IV) improvement of hand hygiene monitoring system (4.743, 100%), (V) regular supervision and inspection in the department (4.657, 100%), (VI) inclusion in the safety target of hospital management (4.643, 100%). In the implementation stage of the improvement measures nosocomial infections in our hospital include lower respiratory tract infection, bacteremia, urinary tract infection, surgical site (superficial incision/deep incision/lacunae) infection, infectious diarrhea, etc. The incidence of nosocomial infection in the three stages was 0.68%, 0.81% and 0.70%, respectively. Infections caused by multidrug-resistant bacteria (MRSA, CRE, CRKP, CRAB, CRPA) accounted for 49.13%, 29.77%, and 25.02%, respectively, The utilization rates of antibiotics were 41.77%, 41.09% and 38.55%, respectively, in the three stages.
Limitations
The hand hygiene research programme achieved gradual improvements using the method complying with the WHO’s hand hygiene model and systematic evaluation of the five aspects of intervention. This was a cohort and cross-sectional study. The results showed that the overall compliance rate of hand hygiene gradually increased as the project advanced. Different groups of professionals showed great differences in compliance, which is similar to the results of hand hygiene research in other regions. In a previous study, nurses (83.5%) had the highest rate of compliance, while that for doctors was moderate (45.2%) (19). Although the hand hygiene data of the hospital improved after the improvement project was implemented, some factors that influence the manual observation of hand hygiene mean that considerable bias, known as the Hawthorne effect, has to be taken into account when interpreting such data (20,21).
In addition to using the World Health Organization hand hygiene survey record sheet (five time points of hand hygiene) to evaluate the compliance rate. We also check validity of hand hygiene using the seven step or spot check the hand sampling pathogen culture by sterile cotton swab monthly.
Ongoing efforts with hand hygiene are needed to prevent nosocomial infections in the future, random control blinded methods will be adopted to study hand hygiene in individual departments and wards, various facilities such as electronic monitoring and voice reminders will be used (22-25), the consumption and use of hand hygiene articles will be investigated (26,27), hand hygiene research in patients will be studied (28), comprehensive evaluation and analysis incorporating the incidence of infections will be conducted, and the effect of hand hygiene improvement on the prevention and control of hospital-acquired infections will be evaluated.
Conclusions
In conclusion, the hospital carried out a hand hygiene improvement project. The plan and implementation measures were reliable. The improvement plan covered all elements and aspects. The research design was relatively comprehensive.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the MDAR reporting checklist. Available at http://dx.doi.org/10.21037/atm-20-5480
Data Sharing Statement: Available at http://dx.doi.org/10.21037/atm-20-5480
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/atm-20-5480). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. Because the study focused on hospital HCWs, the study was approved by the local ethics committee or written informed consent from the participants before the study was not necessary. The study complied with the ethical principles of the Declaration of Helsinki, as amended in 2013.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Chen WS, Zhang WH, Li ZJ, et al. Evaluation of manual and electronic healthcare-associated infections surveillance: a multi-center study with 21 tertiary general hospitals in China. Ann Transl Med 2019;7:444. [Crossref] [PubMed]
- Pong S, Holliday P, Fernie G. Effect of electronic real-time prompting on hand hygiene behaviors in health care workers. Am J Infect Control 2018;46:768-74. [Crossref] [PubMed]
- Thompson D, Bowdey L, Brett M, et al. Using medical student observers of infection prevention, hand hygiene, and injection safety in outpatient settings: A cross-sectional survey. Am J Infect Control 2016;44:374-80. [Crossref] [PubMed]
- Boyce JM, Pittet D. Guideline for Hand Hygiene in Health-Care Settings. Recommendations of the Healthcare Infection Control Practices Advisory Committee and the HICPAC/SHEA/APIC/IDSA Hand Hygiene Task Force. Society for Healthcare Epidemiology of America/Association for Professionals in Infection Control/Infectious Diseases Society of America. MMWR Recomm Rep 2002;51:1. [PubMed]
- Arntz PR, Hopman J, Nillesen M, et al. Effectiveness of a multimodal hand hygiene improvement strategy in the emergency department. Am J Infect Control 2016;44:1203-7. [Crossref] [PubMed]
- Jeanes A, Coen PG, Drey NS, et al. The development of hand hygiene compliance imperatives in an emergency department. Am J Infect Control 2018;46:441-7. [Crossref] [PubMed]
- Gilhooly D, Green SA, McCann C, et al. Barriers and facilitators to the successful development, implementation and evaluation of care bundles in acute care in hospital: a scoping review. Implement Sci 2019;14:47. [Crossref] [PubMed]
- Wiles LL, Roberts C, Schmidt K. Keep it clean: a visual approach to reinforce hand hygiene compliance in the emergency department. J Emerg Nurs 2015;41:119-24. [Crossref] [PubMed]
- Lydon S, Greally C, Tujjar O, et al. Psychometric evaluation of a measure of factors influencing hand hygiene behaviour to inform intervention. J Hosp Infect 2019;102:407-12. [Crossref] [PubMed]
- Seo HJ, Sohng KY, Chang SO, et al. Interventions to improve hand hygiene compliance in emergency departments: a systematic review. J Hosp Infect 2019;102:394-406. [Crossref] [PubMed]
- Chauhan K, Pandey A, Thakuria B. Hand hygiene: An educational intervention targeting grass root level. J Infect Public Health 2019;12:419-23. [Crossref] [PubMed]
- Kingston L, O'Connell NH, Dunne CP. Hand hygiene-related clinical trials reported since 2010: a systematic review. J Hosp Infect 2016;92:309-20. [Crossref] [PubMed]
- Møller-Sørensen H, Korshin A, Mogensen T, et al. New technology markedly improves hand-hygiene performance among healthcare workers after restroom visits. J Hosp Infect 2016;92:337-9. [Crossref] [PubMed]
- Daniels IR, Rees BI. Handwashing: simple, but effective. Ann R Coll Surg Engl 1999;81:117-8. [PubMed]
- WHO Guidelines on Hand Hygiene in Health Care. First global patient safety challenge. Clean care is safer care 2010. Available online: http://www.who.int/ patientsafety/en/. [Accessed 24 August].
- Musuuza JS, Barker A, Ngam C, et al. Assessment of Fidelity in Interventions to Improve Hand Hygiene of Healthcare Workers: A Systematic Review. Infect Control Hosp Epidemiol 2016;37:567-75. [Crossref] [PubMed]
- Dane AV, Schneider BH. Program integrity in primary and early secondary prevention: are implementation effects out of control? Clin Psychol Rev 1998;18:23-45. [Crossref] [PubMed]
- Dusenbury L, Brannigan R, Falco M, et al. A review of research on fidelity of implementation: implications for drug abuse prevention in school settings. Health Educ Res 2003;18:237-56. [Crossref] [PubMed]
- Brühwasser C, Hinterberger G, Mutschlechner W, et al. A point prevalence survey on hand hygiene, with a special focus on Candida species. Am J Infect Control 2016;44:71-3. [Crossref] [PubMed]
- Hagel S, Reischke J, Kesselmeier M, et al. Quantifying the Hawthorne effect in hand hygiene compliance through comparing direct observation with automated hand hygiene monitoring. Infect Control Hosp Epidemiol 2015;36:957-62. [Crossref] [PubMed]
- Magnus TP, Marra AR, Camargo TZ, et al. Measuring hand hygiene compliance rates in different special care settings: a comparative study of methodologies. Int J Infect Dis 2015;33:205-8. [Crossref] [PubMed]
- Mahida N. Hand hygiene compliance: are we kidding ourselves? J Hosp Infect 2016;92:307-8. [Crossref] [PubMed]
- Sánchez-Carrillo LA, Rodríguez-López JM, Galarza-Delgado DÁ, et al. Enhancement of hand hygiene compliance among health care workers from a hemodialysis unit using video-monitoring feedback. Am J Infect Control 2016;44:868-72. [Crossref] [PubMed]
- Farmer CM, Wells JK. Effect of enhanced seat belt reminders on driver fatality risk. J Safety Res 2010;41:53-7. [Crossref] [PubMed]
- Srigley JA, Gardam M, Fernie G, et al. Hand hygiene monitoring technology: a systematic review of efficacy. J Hosp Infect 2015;89:51-60. [Crossref] [PubMed]
- Haubitz S, Atkinson A, Kaspar T, et al. Handrub Consumption Mirrors Hand Hygiene Compliance. Infect Control Hosp Epidemiol 2016;37:707-10. [Crossref] [PubMed]
- Lee YF, Merican H, Nallusamy R, et al. Hand hygiene compliance in Penang, Malaysia: Human audits versus product usage. Am J Infect Control 2016;44:e95-7. [Crossref] [PubMed]
- Srigley JA, Furness CD, Gardam M. Interventions to improve patient hand hygiene: a systematic review. J Hosp Infect 2016;94:23-9. [Crossref] [PubMed]
(English Language Editor: J. Reynolds)


