
Exploring the growth patterns of medical demand for eye care: a longitudinal hospital-level study over 10 years in China
Introduction
Accumulating evidence suggests that an era of exploding medical demand has arisen globally and that people are visiting hospitals more frequently than ever before (1-4). These increases also inflict heavier burdens on the eye care system (5,6). Increasing outpatient visits reduce each patient’s meeting time with doctors and cause doctor overload, resulting in insufficient medical communication (7). Previous studies have revealed that uneven medical demand distributions, such as the weekend effect (8-10) and the July effect (11,12), are related to unsatisfactory medical outcomes. Thus, the magnitude of increases in medical demand and their growth patterns have critical management implications for optimizing medical supply and improving the safety and quality of medical services. However, there has been no systematic analysis of medical demand for eye care to detect the potential influences of demand on medical services for ophthalmology outpatients.
Eye care has advantageous features for studies of medical demand, including full coverage of age groups, diversity of demand in urgency and quality, and sensitivity of supply-demand matching (13). As the most reputed tertiary-level ophthalmic hospital in China, Zhongshan Ophthalmic Center (ZOC) received approximately 8 million person-times outpatient visits from 2008 to 2017, which provides a good sample for panoramic study. As the new ZOC campus opened in 2018, our analysis covers only the period before 2018 to control potentially related influences.
Here, by longitudinally observing and comparing these records, we present temporal and geographical atlases of medical demand for eye care at the hospital level. We show the dynamic relationship between the supply side and the demand side along with demand growth. Temporally, we checked the growth pattern evolution over the cycles of weeks and years. Geographically, we identified the proportions of non-local patients [from cities other than Guangzhou (GZ) in Guangdong (GD) Province, or from provinces other than GD Province in China] and measured flowing demand liquidity at both the provincial and national levels. We calculated the revisit interval as the stickiness of medical demand and present its changes. All of the analyses reflect the distribution of medical demand for eye care and indicate that the growth patterns of demand may bring diverse challenges for Chinese ophthalmologists in the era of exploding healthcare demand. We present the following article in accordance with the STROBE reporting checklist (available at http://dx.doi.org/10.21037/atm-20-2939).
Methods
Data collection and usage
Outpatient visit records were collected and exported from the electronic health record (EHR) system of ZOC. The records totalled over 8 million and covered the time period from 2008 to 2017. We regarded one piece of record as a visit to ZOC in our study. The variables of records included name, address, telephone number, department of appointment, doctors seen, ID, date of appointment and birthdate. The principles outlined in the Declaration of Helsinki (as revised in 2013) were followed throughout the study. The study protocol was approved by the ethics committee (2020KYPJ012). Patient information was anonymized before the analysis and restricted to sharing within the study group.
Individual patient identification
We first used ID as the key to classify the records as unique individuals and gave them new unique IDs. If the original ID was missing, we used name, birthdate, address and telephone number for alignment with known individuals. The above-aligned variables were used as keys to identify other individuals from unaligned records, which were given new unique IDs.
Revisit interval threshold setting
We calculated every revisit interval for each person if the unique ID appeared more than twice in our records. We used half of a year (183 days) as the upper threshold for the revisit interval to control the relationship between two visits. If the revisit interval was longer than half a year, we considered the two visits unrelated and did not include them in the revisit interval analysis.
Statistical analysis
The data analysis was mainly conducted with R (version 3.6.2). We set 0.05 as the significance threshold of the P value. Differences between groups were tested by the Wilcoxon rank-sum test. For any variable, we excluded the missing data during subgroup comparison.
Data retention and security
We retained patients’ personal information only as long as necessary for scientific research. We took precautions to safeguard patients’ personal information against loss, theft and misuse and unauthorized access, disclosure, alteration and destruction by appropriate technical and organizational measures.
Results
Main types of visits to medical institutions in China from 2008 to 2017
By analysing the open data from the National Statistics Bureau, we found that the main types of visits to various levels of medical institutions increased continuously from 2008 to 2017 (Figure 1A). The number of visits to all medical institutions increased by 67%, from 49.01 in 2007 to 81.83 in 2018 (100 million person-times). Both basic medical institutions and hospitals are included in all medical institutions. For hospitals, visits increased stably by 93% each year, from 17.82 in 2008 to 34.39 in 2017 (100 million person-times). Within hospitals, comparing 2008 with 2017, the number of visits to general hospitals increased by 87%. However, although they also increased during 2009–2014, visits to basic medical institutions reached a plateau in 2014. Visits to specialized hospitals increased by 139% from 2008 to 2017, a greater increase than for any other kind of visits, but this category still accounted for a small proportion of the overall demand.
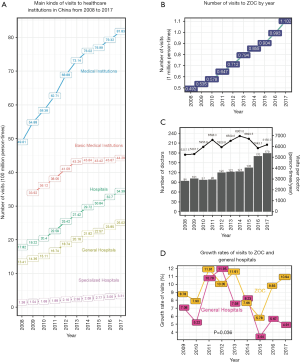
The growth of visits to ZOC and supply-demand relationships
Visits to ZOC increased rapidly over the 10 years from 2008 to 2017 (Figure 1B). All the records have the visit date variable and the visit subdepartment variable, while about 3.7 million (53.3%) visit records have the address variable. Starting with only 0.492 million visits in 2008, the number of visits reached 1.102 million in 2017, a 124% increase. Before 2010, the average rate of growth in the number of visits was 0.043 million per year. However, after 2010, the average growth rate was far higher, 0.075 million per year. We also found that the number of doctors increased rapidly during the 2011–2012 and 2015–2016 periods; both of these increases occurred after the number of visits per doctor increased (Figure 1C). Increases in doctors partially relieved the pressure brought by the increase in total visits in a short period but could not eliminate the regular rebounds of doctor workloads. As ZOC is one of the few tertiary ophthalmic hospitals in China, its size is more comparable to that of a typical general hospital. Compared with general hospitals, ZOC witnessed a similar growth pattern but had a far faster growth rate (paired Wilcoxon rank-sum test: P=0.036) (Figure 1D).
Temporal growth patterns
With regard to weekly cycles, ZOC received the largest number of visits on Monday. We found that the demand patterns of weekdays and weekends significantly differed (2,507.9±791.9 vs. 942.8±293.3 person-times/d, Wilcoxon rank-sum test: P<2.2e−16) (Figure 2A,B). Most increases in visits were caused by changes in weekday visits. There was a visit distribution pattern over the course of a week: Monday (2,775.1±897.6 person-times/d) was usually the most crowded day, followed by Tuesday (2,489.0±818.3 person-times/d), Thursday (2,396.4±743.3 person-times/d), Wednesday (2,002.2±610.7 person-times/d) and Friday (1,999.8±644.5 person-times/d) (Figure 2B, Figure S1). On weekends, patients visited ZOC more on Saturday (1,031.5±290.8 person-times/d) than on Sunday (757.8±251.5 person-times/d) (Wilcoxon rank-sum test: P<2.2e−16). Thus, a Monday peak phenomenon was observed in ZOC outpatients, and the Monday peaks became more evident.
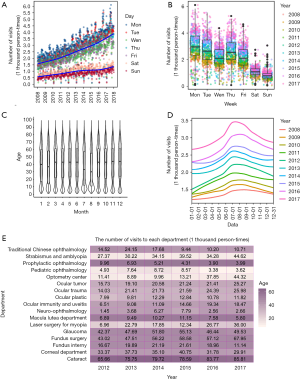
With regard to yearly cycles, the average age of patients visiting during two school vacation periods was lower than in the rest of the year: winter vacations in January and February and summer vacations in July and August (Figure 2C). By the local polynomial regression method, we fit the curves of visits to ZOC over the yearly cycles (Figure 2D). In recent years, as the baseline number of visits increased, vacation peaks in summer gradually became evident but decreased in dominance compared to the winter vacation peaks. During summer vacations, the declining average age of visiting patients can be explained by increases in the number of individuals under 20 years of age (Figure 2C). However, the declines in average patient age during winter vacations (which also include the traditional Chinese New Year holiday) were less evident, although they were also concurrent with increases in the number of patients under the age of 20 years. Because the patient birthday variable in the data lacked reliability before 2012, we analysed the age distribution only from 2012.
Growth patterns among the ocular disease spectrum
All sub-departments of ophthalmology maintained generally stable proportions of patient age groups, indicating that the epidemiology of sub-diseases was consistent (Figure 2E). The cataract department was the most-visited department over the 10-year study period, followed by the fundus surgery department and the glaucoma department. Compared with 2012, the myopia laser surgery department showed the largest increase (552%) by 2017, and the optometry center showed the largest absolute difference in the number of visits (32.91 thousand person-times). Visits to the traditional Chinese ophthalmology department, ocular plastics department, and fundus intern department also decreased greatly in recent years.
Geographical growth patterns
We analyzed the changes in the proportion of non-local patients at both the provincial scale (GD Province) and national scale and compared the geographical coverage of patient sources before and after 2012. We considered non-local patients from other cities or provinces as flowing demand to measure flowing demand liquidity. Within GD Province, we classified patients from cities other than GZ City as non-local patients. Within China, we classified patients from provinces other than GD Province as non-local patients. Within GD Province (Figure 3A), the proportions of non-local patients increased from 21.4%±1.2% in 2008–2010 to 38.2%±0.2% in 2015–2017 (Wilcoxon rank-sum test: P=0.077). Within China (Figure 3B), the proportions of non-local patients increased from 4.61%±0.25% in 2008–2010 to 17.77%±0.23% in 2015–2017 (Wilcoxon rank-sum test: P=0.077).
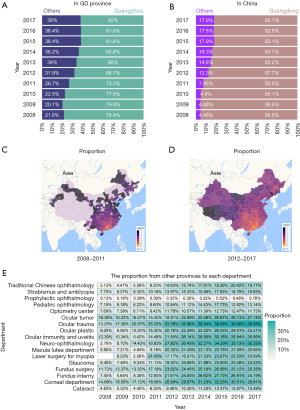
Additionally, we found that the coverage of patient sources increased with greater attraction of flowing demand (Figure 3C,D). As the leading ophthalmic hospital in southern China, ZOC is located in GZ, the capital city of GD Province. It is therefore reasonable that GD Province is the radiation center. In 2008–2011, the main sources of patients were concentrated in southern and eastern China and some less developed areas in more distant provinces. Compared with 2008–2011, patient sources covered almost all of China in 2012–2017, and the scope of radiation from GD Province also increased. Among all departments in 2017, the ocular trauma department had the highest proportion of patients from other provinces, and the neuro-ophthalmology department had the largest changes in the proportion of patients from other provinces (Figure 3E).
The stickiness of patient revisits
After identification alignment (see Methods), about 4.5 million (56%) records have enough identification information and were available for revisit interval analysis. We considered the revisit interval as the stickiness of medical demand and used the revisit interval within half a year (183 days) for measurement. Because the second half-year of 2017 was partly included and the records of 2018 were not included, the revisit intervals in 2017 were shorter than those in other years.
Both within GD Province and China, non-local patients visited ZOC more frequently than local patients each year after 2010 (Wilcoxon rank-sum test: **P<0.01, *P<0.05) (Figure 4A,B), which means that the stickiness of non-local patients was higher than that of local patients during the visiting process. From 2011 to 2012, the revisit interval to ZOC decreased dramatically. In GZ City, the revisit interval decreased from 26 [9, 71] days (2008–2011) to approximately 21 [7, 58] days (2012–2017) (Wilcoxon rank-sum test P<2.2e−16) (Figure 4A). In other cities in GD Province, the revisit interval decreased from 28 [9, 71] days (2008–2011) to 17 [7, 47] days (2012–2017) (Wilcoxon rank-sum test P<2.2e−16) (Figure 4A). Comparing the results among other provinces in China, the revisit interval in GD Province decreased from 26 [9, 71] days (2008–2011) to approximately 20 [7, 55] days (2012–2017) (Wilcoxon rank-sum test: P<2.2e−16) (Figure 4B), while in other provinces, the revisit interval decreased from 21 [7, 63] days (2008–2011) to approximately 13 [4, 35] days (2012–2017) (Wilcoxon rank-sum test: P<2.2e−16) (Figure 4B).
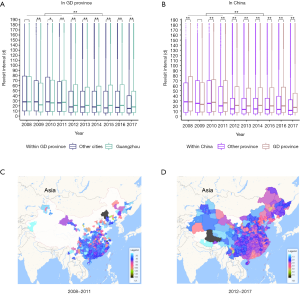
Before 2011, there were far fewer revisits from distant areas; visits from these areas were usually a single visit of a patient with a complicated disease (Figure 4C). After 2012, revisits from distant areas increased greatly and covered almost all of China (Figure 4D). In southern China and north-eastern China, the mean revisit interval was mostly within the range of 25–40 days (Figure 4C). In less developed areas, including western and southwestern China, the mean revisit interval fell mostly within a lower range (Figure 4D).
Discussion
The aging population and exploding medical demand further challenge the supply ability of hospitals and create burdens on doctors. The growth patterns of visits explain how the dynamic uneven distributions of medical demand exacerbates the supply-demand balance for outpatients and the safety and quality of medical services. Although a previous study also addressed the growth of outpatient visits (14), our research provides a more quantitative study of eye care demand fluctuation in terms of both temporal and geographical aspects. After illustrating the general explosion of medical demand in China, we examined the increases in medical demand at the hospital level (ZOC). The relationship between supply and demand was also analyzed during a 10-year period, which revealed periodic imbalances and regular rebounds. The temporal atlas revealed uneven distributions in the cycles of weeks and years, referred to as Monday peaks and vacation peaks, and these uneven distributions became more evident over time. The geographical atlas revealed the expanding coverage of patient sources with more visits and higher flowing demand liquidity. The stickiness of patients increased, and non-local patients presented higher stickiness than local patients. Diverse growth speeds and flowing demand liquidity existed among subdepartments of ophthalmology.
Based on the above analysis of the demand growth and its pattern, our research revealed that Chinese ophthalmologists may face three main challenges under imbalanced supply-demand conditions: (I) dynamic overload challenges over the cycles of weeks (Monday peaks) and years (vacation peaks) due to sustained increases and the uneven distribution of medical demand, which aggravates the psychological and physical health of the medical staff; (II) increases in the range of non-local patients seeking better medical treatment and traveling to distant top hospitals, which brings more diverse cultural differences for doctors; (III) increased stickiness of patients, which requires doctors to communicate with individuals more frequently and continuously.
Considering the feedback loop between supply and demand, the uneven distribution of demand in medical areas is becoming increasingly prominent. Favourable factors in China, such as the rising income of its citizens, popularization of mobile internet (15) and high-speed transportation network, not only empower patients to pursue better medical resources but also test the capacity of regional advanced medical centers. Moreover, these dominant hospitals still compete to serve more patients and thus expand their load capacity to the limit (16). Further strengthening the flexibility and effectiveness of the three-tier healthcare system in remote regions should help ease the overload of central hospitals.
Previous studies have provided methods to predict demand and optimize outpatient scheduling (17-19). Classic algorithms for predicting time-series medical demand, such as the auto-regressive integrated moving average (ARIMA) model and the single exponential smoothing (SES) model, are not precise or robust enough (20). Deep learning methods such as long short-term memory (LSTM), a kind of recurrent neural network (RNN), indicate the possibility of building more dynamic and accurate demand prediction models (21-23). A comprehensive system combining demand prediction and supply allocation is needed to mitigate the imbalance of supply-demand conditions. Recently, AI applications in eye disease screening and guidance have been able to sync high-quality healthcare services to individuals’ mobile terminal, providing a feasible method for tackling this increasing burden (24-27).
Prospective studies for precisely predicting demand growth and optimizing the allocation of medical resources on the supply side based on our findings will help reduce the supply and demand imbalance and improve the quality and safety of ophthalmology outpatients.
Limitations
Several limitations exist in our study. First, our study included records from only a single center, and future multi-center studies may obtain more credible results. Moreover, the numbers of patients from different destinations varied greatly, and few records were available for patients from some distant areas, which decreased the credibility of our conclusions regarding these areas.
Conclusions
In summary, this study implies several challenges brought by the increasing demand for ophthalmology outpatient. The growth patterns of demand for eye care indicate potential challenges for ophthalmologists at the hospital level, including regular workload peaks, a wider range of patients with diverse cultural backgrounds, and higher stickiness of patients.
Acknowledgments
We appreciate Information Department at ZOC for their roles in data acquisition, and our sponsors of funding.
Funding: This study is funded by the National Key R&D Program of China (2018YFC0116500), and the Science and Technology Planning Projects of Guangdong Province (2018B010109008). The sponsors played no role in the study.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at http://dx.doi.org/10.21037/atm-20-2939
Data Sharing Statement: Available at http://dx.doi.org/10.21037/atm-20-2939
Peer Review File: Available at http://dx.doi.org/10.21037/atm-20-2939
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/atm-20-2939). HL is the Vice President of Zhongshan Ophthalmic Center (ZOC), and reported grants from the National Key R&D Program of China (2018YFC0116500), and the Science and Technology Planning Projects of Guangdong Province (2018B010109008). YL is the President of ZOC. MY, WC are undergoing their internships at ZOC. YY and TW are PhD undergraduates at ZOC. The other authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy and integrity of any part of the work are appropriately investigated and resolved. All the procedures in this study were arranged strictly with the approval of the institutional review board of Zhongshan Ophthalmic Center of Sun Yat-sen University (IRB-ZOC-SYSU) (2020KYPJ012). The principles outlined in the Declaration of Helsinki (as revised in 2013) were followed throughout the study. Patient information was anonymized before the analysis and restricted to sharing within the study group. This study outcomes will help improve the quality of medical services and healthcare management in the future.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Deloitte. 2019 Global health care outlook. 2019. Available online: https://www2.deloitte.com/global/en/pages/life-sciences-and-healthcare/articles/global-health-care-sector-outlook.html. Accessed Nov 30, 2019.
- Babalola O. Consumers and Their Demand for Healthcare. J Health Med Econ 2017;3:6. [Crossref]
- Sundiatu Dixon-Fyle TK. Engaging consumers to manage health care demand. McKinsey. 2010. Available online: https://www.mckinsey.com/industries/healthcare-systems-and-services/our-insights/engaging-consumers-to-manage-health-care-demand. Accessed Nov 30, 2019.
- Rice TH, Unruh L; Association of University Programs in Health Administration. The economics of health reconsidered. 4th edition. Chicago, Illinois: Health Administration Press; Arlington, Virginia: Association of University Programs in Health Administration, 2016.
- Kotecha A, Turner S, Vasilakis C, et al. Improving care and increasing efficiency—challenges in the care of chronic eye diseases. Eye 2014;28:779-83. [Crossref] [PubMed]
- David K. Coats LPF, William L. Rich III. Growing demand for eye care services may highlight shortage of ophthalmologists. 2010. Available online: https://www.healio.com/news/ophthalmology/20120331/growing-demand-for-eye-care-services-may-highlight-shortage-of-ophthalmologists. Accessed Feb 17, 2020.
- Xiao SC, Wang L, Liu X, et al. Communication in the Chinese doctor–patient–family relationship: a qualitative study of expectations and experiences in a breast surgery setting. Lancet Glob Health 2018;6:S53. [Crossref]
- Kenton W. Weekend Effect. 2018. Available online: https://www.investopedia.com/terms/w/weekendeffect.asp. Accessed Nov 30, 2019.
- Black N. Higher Mortality in Weekend Admissions to the Hospital: True, False, or Uncertain? JAMA 2016;316:2593. [Crossref] [PubMed]
- Clarke MS, Wills RA, Bowman RV, et al. Exploratory study of the 'weekend effect' for acute medical admissions to public hospitals in Queensland, Australia. Intern Med J 2010;40:777-83. [Crossref] [PubMed]
- Englesbe MJ, Pelletier SJ, Magee JC, et al. Seasonal Variation in Surgical Outcomes as Measured by the American College of Surgeons-National Surgical Quality Improvement Program (ACS-NSQIP). Ann Surg 2007;246:456-62. [Crossref] [PubMed]
- Inaba K, Recinos G, Teixeira P, et al. Complications and Death at the Start of the New Academic Year: Is There a July Phenomenon? J Trauma 2010;68:19-22. [Crossref] [PubMed]
- Ansah JP, De Korne D, Bayer S, et al. Future requirements for and supply of ophthalmologists for an aging population in Singapore. Hum Resour Health 2015;13:86. [Crossref] [PubMed]
- Abrams K, Balan-Cohen A, Durbha P. Growth patterns in outpatient Medicare hospital services. 2018. Available online: https://www2.deloitte.com/us/en/insights/industry/health-care/outpatient-hospital-services-medicare-incentives-value-quality.html. Accessed Jan 9, 2020.
- Zhang W, Deng Z, Evans R, et al. Social Media Landscape of the Tertiary Referral Hospitals in China: Observational Descriptive Study. J Med Internet Res 2018;20:e249. [Crossref] [PubMed]
- Yip WC, Hsiao W, Meng Q, et al. Realignment of incentives for health-care providers in China. Lancet 2010;375:1120-30. [Crossref] [PubMed]
- Cayirli T, Veral E. Outpatient Scheduling in Health Care: A Review of Literature. Prod Oper Manag 2003;12:519-49. [Crossref]
- Lin WC, Goldstein IH, Hribar MR, et al. Secondary Use of Electronic Health Record Data for Prediction of Outpatient Visit Length in Ophthalmology Clinics. AMIA Annu Symp Proc 2018;2018:1387-94. [PubMed]
- Hribar MR, Read-Brown S, Reznick L, et al. Evaluating and Improving an Outpatient Clinic Scheduling Template Using Secondary Electronic Health Record Data. AMIA Annu Symp Proc 2018;2017:921-9. [PubMed]
- Luo L, Luo L, Zhang X, et al. Hospital daily outpatient visits forecasting using a combinatorial model based on ARIMA and SES models. BMC Health Serv Res 2017;17:469. [Crossref] [PubMed]
- Choi E, Bahadori MT, Schuetz A, et al. Doctor AI: Predicting Clinical Events via Recurrent Neural Networks. JMLR Workshop Conf Proc 2016;56:301-18. [PubMed]
- Guan G, Engelhardt BE. Predicting Sick Patient Volume in a Pediatric Outpatient Setting using Time Series Analysis. Proc Mach Learn Res 2019;106:1-16.
- Ashfaq A, Sant’Anna A, Lingman M, et al. Readmission prediction using deep learning on electronic health records. J Biomed Inform 2019;97:103256. [Crossref] [PubMed]
- Du XL, Li WB, Hu BJ. Application of artificial intelligence in ophthalmology. Int J Ophthalmol 2018;11:1555-61. [PubMed]
- Ting DSW, Pasquale LR, Peng L, et al. Artificial intelligence and deep learning in ophthalmology. Br J Ophthalmol 2019;103:167-75. [Crossref] [PubMed]
- Ting DSJ, Ang M, Mehta JS, et al. Artificial intelligence-assisted telemedicine platform for cataract screening and management: a potential model of care for global eye health. Br J Ophthalmol 2019;103:1537-8. [Crossref] [PubMed]
- Lin H, Li R, Liu Z, et al. Diagnostic Efficacy and Therapeutic Decision-making Capacity of an Artificial Intelligence Platform for Childhood Cataracts in Eye Clinics: A Multicentre Randomized Controlled Trial. EClinicalMedicine 2019;9:52-9. [Crossref] [PubMed]


