Robotic-assisted right middle lobectomy for poorly differentiated squamous cell carcinoma
Clinical data
History
The patient, a 73-year-old men, was admitted due to “sputum with blood for one month” and “mass in the right middle lung lobe”. One month ago, he developed cough and expectoration with blood-stained sputum. Two weeks ago, chest CT showed a soft-tissue mass with irregular border in the lateral segments of the right middle lung lobe. Bronchoscopy detected a mass at the bronchial orifice in the lateral segments of the right middle lung lobe. No malignant cell was detected at biopsy pathology. The patient’s complaints did not include low fever, night sweats, nausea, vomiting, abdominal distension, diarrhoea, heart palpitations, or discomfort of precordial area. His mental status, physical performance, appetite, and sleep were normal, and the body weight did not obviously change. Urination and defecation were normal.
Physical examination
Physical examinations upon admission showed no obviously positive signs. The cervical and supraclavicular lymph nodes were not abnormally enlarged.
Auxiliary examination
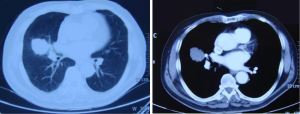
Chest CT: a soft-tissue mass sized 4 cm × 3 cm with irregular border and unclear margin was found in the right middle lung lobe (near the pulmonary hilum). The mediastinal lymph nodes were slightly swollen (Figure 1).
Epigastric ultrasound, bone ECT, and head MRI did not find the evidence of remote metastasis. Other surgical contraindications including thyroid nodules and breast nodules were ruled out after multidisciplinary consultations.
No obvious abnormality was found in ECG, echocardiography, pulmonary function test, blood gas analysis, and other biochemical tests.
Pre-operative preparation
Based on the imaging results, “a space-occupying lesion in the right middle lung lobe” was considered, and there was a high possibility of malignancy. Since the mass was close to the pulmonary hilum, making the wedge resection impossible. Thus, resection of the middle lobe was planned. The subsequent surgical protocol was determined based on the results of intraoperative frozen section biopsy. (If the lesion was found to be malignant in the frozen biopsy, lymph node dissection would be performed). The surgery was planned to be completed using da Vinci robotic system.
Surgical procedures
Anesthesia and body position
After the induction of general anesthesia, the patient was placed in a lateral decubitus position under double-lumen endotracheal intubation. With his hands put in front of head, he was fixed in a Jackknife position with single-lung (left) ventilation (Figure 2).

Surgical procedures
Distribution of incisions (“8857”): a 1.5-cm camera port was created in the 8th intercostal space (ICS) at right posterior axillary line, and two 1.0-cm working ports were separately made in the 5th ICS at right anterior axillary line and the 8th ICS at scapular line. A 4-cm auxiliary port was made in the 7th ICS at midaxillary line (Figure 3).
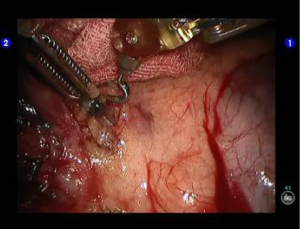
During the thoracic cavity inspection, the camera was inserted via the camera port and found no obvious adhesion or effusion in the thoracic cavity, and the pulmonary fissures were well developed.
The robot Patient Cart were connected over the patient’s head. A 12-mm trocar was placed at the camera port in the 8th ICS at posterior axillary line to be attached with the camera arm. The robot metal trocars were respectively attached to the 1# arm (left hand) and 2# arm (right hand) at the incisions in the 5th ICS anterior axillary line and the 8th ICS scapular line. Incision protector was applied in the auxiliary port.
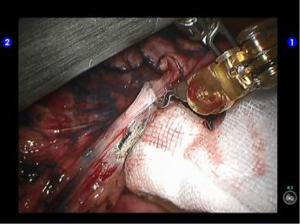
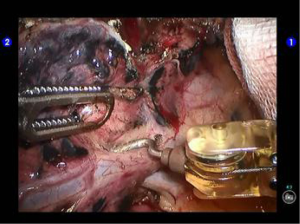
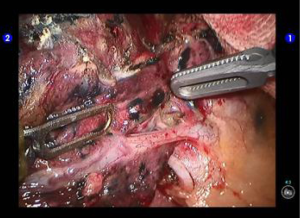
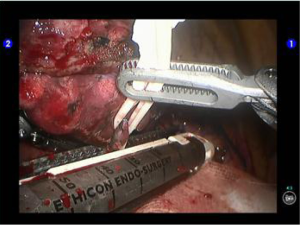
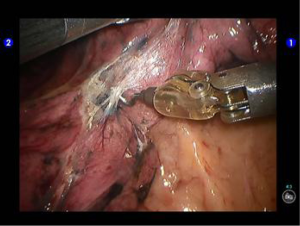
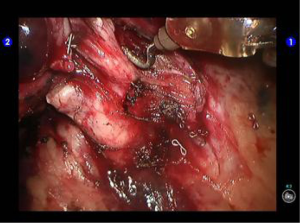
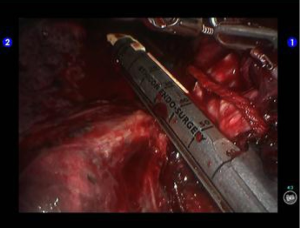
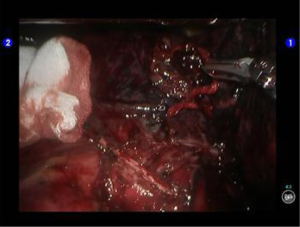
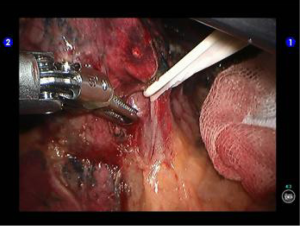
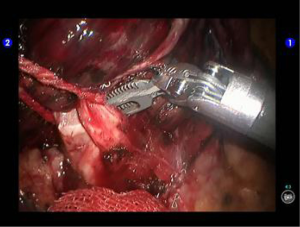
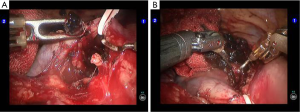
Lobectomy: the left arm was attached to bipolar cautery forceps, and the right arm to a unipolar cautery hook. The oblique fissure was dissected, the mediastinal pleura was cut open behind the phrenic nerve, and then the middle lobe branches of the upper pulmonary vein was dissociated (Figures 4,5). Since an abnormal vascular branch was found at the inner side of the vein, elastic cord was used to suspend and pull the middle lobe vein, and then the abnormal branch was sealed and handled with bipolar cautery forceps (Figures 6,7). The camera arm was inserted via the auxiliary port. Endoscopic flexible cutter/stapler was inserted from the camera port, and the middle lobe vein was transected using a white reload (Figure 8). Move the camera back to the camera port. Cut open the inferior part of the oblique fissure (Figure 9), remove the interlobar lymph nodes (Figure 10), and thoroughly dissociate the middle lobe bronchus. However, the stapler could not go through the small gap between the middle lobe bronchus and vessels (Figures 11,12). Since the tumor invaded the upper lobe, the involved site was divided at the upper margin using a blue reload (Figure 13A,B). Inspection showed that there was no residual lymph node around it. The middle lobe bronchus, middle lobe artery, and the residual horizontal fissure were clamped with a golden reload (Figure 14). An anesthesiologist was asked to suction sputum and ventilate the operated lung. After CXR revealed good expansion of the lower lobe, release the stapler to divide the middle lobe (Figure 15). An endoscopic retriever was inserted via the auxiliary port to harvest the dissected specimen. Frozen pathology showed that it was a lung cancer to be further classified.
Lymph node dissection: remove the hilar lymph nodes (Figure 16). After the inferior pulmonary ligament was divided till the inferior lung vein level, no swollen lymph node was seen at the pulmonary ligament or near the esophagus. Open the posterior mediastinal pleura to remove the subcarinal lymph nodes (Figure 17). Inspect and remove lymph nodes before the superior vena cava (Figure 18). Open the upper mediastinal pleura to remove the lymph nodes near the trachea (Figure 19). There were several swollen lymph nodes near the lower trachea and deep behind the azygos vein arch. Dissociate the azygos vein arch from two directions (upward and downward) using elastic cords and then thoroughly remove the lymph nodes (Figure 20A,B).
Wash the thoracic cavity. Air leakage was observed at the cut surface of lung after lung recruitment. It was satisfactorily managed using the bipolar cautery forceps. When no obvious bleeding was observed at all the trauma surfaces, the TISTAT absorbable hemostatic gauze was applied at each trauma surface and cut surface. The thoracic drainage tube was indwelled at the working port at the 5th ICS and at the camera port, respectively. Close the chest after lung recruitment.
Postoperative treatment
Postoperative treatment is similar to that after the conventional open lobectomy. The thoracic drainage tube was withdrawn 14 days after the surgery. The post-operative pathological stage was pT2aN0M0. Currently the patient was under follow-up.
Pathological diagnosis
Poorly differentiated squamous cell carcinoma at the right middle lung lobe, accompanied with adenoid differentiation. No cancer cell was detected at the bronchial stump or the hilar/mediastinal lymph nodes.
Comment
Anatomic resection of the middle lobe of right lung is often particularly difficult due to the aplasia of horizontal fissure/oblique fissure or the adhesion of inflammatory lymph nodes around vessels and bronchus. In our current case, adhesion of lymph nodes around vessels, invasion of tumor into the upper lobe, and aplasia of lobar fissure were observed; thus, the bronchus, middle lobe artery, and horizontal fissure were also transected and removed after the middle lobe vein transection and lymph node removal. A key point in this procedure is the resection scope. Efforts should be made to ensure thorough resection and meanwhile protect the inferior lobe bronchus and lung artery from being damaged. Also, removal of lymph nodes must also be thorough. In our current case, multiple lymph nodes around the inferior bronchus in the middle lobe of right lung became swollen. We dissociated the azygos vein arch and then thoroughly dissected the lymph nodes. In addition, the stapler inserted via the auxiliary port made in the 7th ICS at midaxillary line can conveniently handle the lobar fissures, arteries, and bronchus. However, since there is a large angle in handling the middle lobe vein, we need to move the camera to the auxiliary port and then insert the stapler via the camera port. This is a routine step in endoscopic surgeries but seems a bit complicated in the robotic surgeries. Thus, a skillful assistant who is familiar with the performances of the robotic arms is critically important.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.