Robotic Thoracic Surgery Column
Robotic thoracic surgery of the left pleural cupula mediastinal mass
Clinical data
- Medical history: the patient, a 67-year-old women, was admitted due to “thoracic back pain accompanied with chest tightness and shortness of breath for over 5 months”. She suffered from thoracic back pain 5 months ago, which was accompanied with chest tightness and shortness of breath after physical activities. Chest CT displayed the presence of a mediastinal mass. She then visited our hospital for surgical treatment. She complained that she had a previous history of angina pectoris for 2 years, which had not received any formal diagnosis or treatment. She had no previous history of other conditions.
- Physical examination: no positive sign was detected during the physical examination at admission.
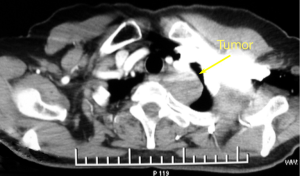
- Auxiliary examination: thoracic contrast-enhanced CT scan showed that the lesion had a close relationship with the left subclavian artery (Figure 1). Thyroid radionuclide scan suggested that the lesion was not originated from the thyroid.
Pre-operative preparation
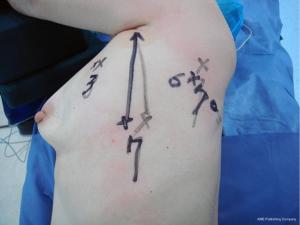
Conventional skin preparation was performed. The planned ports were marked on body surface.
Procedures
Anesthesia and body position
After the induction of general anesthesia, the patient was placed in a right lateral decubitus position under double-lumen endotracheal intubation. With his hands put in front of head, he was fixed in a Jackknife position.
Surgical procedures
- Incisions: a 1.5-cm camera port was created in the 7th intercostal space at left middle axillary line. Two 0.8-cm working ports were created in the 3rd intercostal space between the left anterior axillary line and the midclavicular line and in the 6th intercostal space between the posterior axillary line and scapular line, respectively (Figure 2).
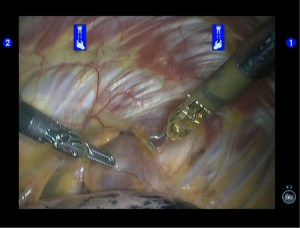
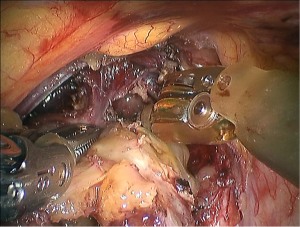
- Exploration of the thoracic cavity and insertion of the robot arms: the endoscopic airtight trocar was inserted through the camera port to establish 8-mmHg artificial pneumothorax, then the robotic endoscope was inserted for inspecting the thoracic cavity. Under the endoscopic monitoring, the robot trocars were separately inserted via the two working ports, so as to place the #2 robotic arm (left hand) and the #1 robotic arm (right hand). The #2 robotic arm was connected with the fenetrated bipolar forceps, and the #1 robotic arm with unipolar cautery hook (Figure 3).
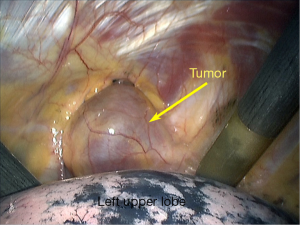
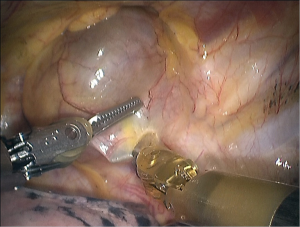
- Inspect the lesion and its relationship with the neighboring tissues/organs: the lesion was located in the oriface of the left upper mediastinal thoracic cavity, with its upper side deep inside the neck. It had normal morphology and smooth surface (Figures 4,5).
- Open the mediastinal pleura (Figure 6).
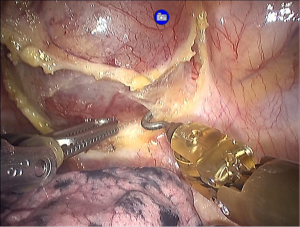
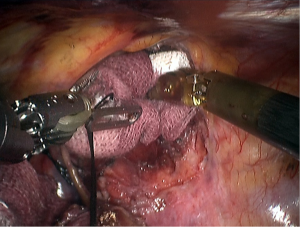
- Dissociate the tumor: sharp dissection of the tumor was performed along the tumor surface. The cautery hook should be close to the tumor surface to avoid hurting the nerves and vessels (Figure 7).
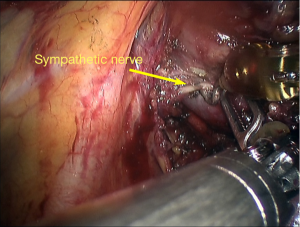
After the sympathetic nerve was carefully dissected, the sympathetic nerve was found to be with an unclear margin with the tumor (Figure 8). A tumor from the sympathetic nerve was considered.
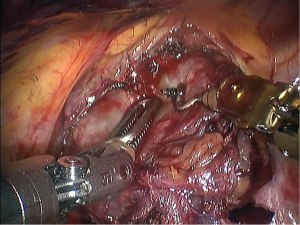
After generally pressing the tumor downwards, the operator could inspect and expose the upper side of the tumor, which was cautiously divided (Figures 9,10). - Resection of tumor (Figure 11).
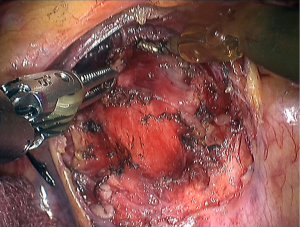
- Hemostasis of the tumor bed (Figures 12,13).
- Harvest the dissected tumor: an endoscopic retriever was inserted via the trocar connected with the left robotic arm to harvest the dissected tumor. After the robot system was withdrawn, the thoracic drainage tube was indwelled at the camera port. Close the chest after sputum suctioning and lung recruitment. The intraoperative blood loss was about 30 mL; no blood was transfused.
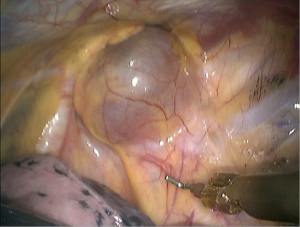
Figure 5 The tumor is located at the sympathetic trunk, which is approximately at the stellate ganglion.
Postoperative treatment
After the surgery, the patient received symptomatic treatment under routine general anesthesia. No antibiotic or hemostatic agent was applied.
Pathological diagnosis
The lesion was pathologically diagnosed as a ganglion cell neuroma at the left posterior upper mediastinum.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
Cite this article as: Xu S, Li B, Ding R, Liu B, Meng H, Wang T, Xu W, Liu X, Wang S. Robotic thoracic surgery of the left pleural cupula mediastinal mass. Ann Transl Med 2015;3(10):141. doi: 10.3978/j.issn.2305-5839.2015.03.04