
Polar value analysis of astigmatic change and rotational stability after implantation of V4c toric implantable collamer lens
Introduction
Uncorrected astigmatism is a common condition that distorts the vision of sufferers, resulting in a significant decline in visual performance (1,2). The toric implantable collamer lens (TICL, STAAR Surgical Company, Monrovia, CA, USA) is widely used to correct myopia and myopic astigmatism. The V4c TICL, which has a 360-µm central hole, is the most recently released product that allows aqueous humor to flow while avoiding the need for an iridotomy. Several studies have shown that implantation of the V4c TICL can safely and effectively correct myopia and myopic astigmatism (3-9).
Despite V4c TICL implantation demonstrating outstanding advantages in the treatment of myopic astigmatism, precise power calculation and accurate placement of the V4c TICL are crucial factors in optimizing visual performance. Moreover, analysis of postoperative astigmatism and accurate assessment of rotational stability (the difference between the achieved axis and intended axis) of the V4c TICL is also vital in obtaining satisfactory postoperative results and evaluating the performance of the V4c TICL in the posterior chamber.
Astigmatism is a vector with magnitude and direction, however, a lack of consideration of the vector nature of astigmatism might result in the omission of important information, leading to inaccurate conclusions (10). Although there are many methods of vector analysis to evaluate astigmatism correction, Næser’s polar value method (11) is an excellent way to understand the exact changes in the composition of astigmatism in refractive surgery. A number of studies (12-14) have applied this method to assess surgically induced astigmatism (SIA) and treatment errors, as well as size and orientation-related changes in astigmatism, following various refractive operations. To the best of our knowledge, no studies to date have used Næser’s method to evaluate the astigmatic results and postoperative rotation of the V4c TICL.
The present study aimed to conduct a retrospective evaluation of the quantitative results of V4c TICL implantation in patients with moderate to high myopic astigmatism with regard to refractive astigmatism and rotational stability.
We present the following article in accordance with the MDAR checklist (available at http://dx.doi.org/10.21037/atm-20-7835).
Methods
An observational study of 72 eyes belonging to 43 patients [13 males, 30 females; mean age, 25.57 years ±4.51 (SD), range, 18–42 years] who underwent V4c TICL implantation to treat myopic astigmatism was retrospectively conducted. All operations took place between June 2019 and September 2019. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by ethics board of Shenzhen Eye Hospital (NO.:b-07). All patients were healthy and met the criteria for refractive surgery. After explaining the nature of the procedure prior to surgery, all patients signed written informed consent. The exclusion criteria were: any previous eye surgery; an anterior chamber depth (ACD) from the endothelium to the lens of <2.8 mm, a corneal endothelial cell density (ECD) of <2,000 cells/mm2; patients with a history of these conditions (e.g., corneal diseases, cataract, amblyopia, glaucoma or ocular hypertension, retinopathy, uveitis) or patients with postoperative corrected distance visual acuity (CDVA) of 20/40 or worse.
Preoperative and postoperative evaluation
Patients were evaluated preoperatively and postoperatively according to the standard protocol. Examinations were conducted before the operation, on the first postoperative day, and at the 1-week and 1-month follow-ups. Uncorrected distance visual acuity (UDVA) and CDVA were assessed, and each follow-up visit entailed objective and subjective optometry. Slit-lamp microscopy, non-contact tonometry for measurement of the intraocular pressure (IOP), and dilated fundus examination were performed preoperatively and postoperatively. Pentacam (Pentacam HR; Oculus, Inc., Wetzlar, Germany) or Sirius (Costruzione Strumenti Oftalmici (CSO), Florence, Italy, software version 2.5) was used to measure the preoperative white-to-white distance, keratometric value, and ACD, while anterior segment optical coherence tomography was used for postoperative measurements. Preoperative axial length was measured using Pentacam. The central vault of the TICL was assessed using anterior segment optical coherence tomography (Tomey, SS-1000, Japan). Full postoperative examination was performed at the final visit.
Polar value analysis was used to assess the rotational stability of the V4c TICL. In this method, the intended axis of the targeted induced astigmatism (TIA) is perpendicular to the preoperative refractive cylinder axis. The axis of the SIA is the achieved axis, which is representative of the actual change in astigmatic direction obtained by surgery. The difference between the achieved axis and the intended axis at the last follow-up was taken as the rotation of the V4c TICL.
Surgical technique
All surgical procedures were conducted by two experienced surgeons (X.H.L; Z.H.Y). The power and size of the V4c TICL were determined according to the manufacturer’s guidelines. Emmetropia was the target refraction after surgery in all cases. Taking cyclotorsion into account, with the patient placed in the supine position, a marker pen was used to mark the limbus at the 3- and 9-o’clock positions under the slit lamp before surgery.
After topical anesthesia, a 3.0-mm main temporal incision was made and paracentesis was carried out. Then, an injector cartridge was used to insert the V4c TICL via the main temporal incision. The anterior chamber was injected with hyaluronate sodium 1% (Hyal 2000; LG Life Sciences Ltd., Seoul, Korea), after which alignment of the V4c TICL with the cylinder axis of the patient’s eye was ensured. After validation of the V4c TICL axis, a balanced salt solution-filled syringe was used for the manual removal of the viscoelastic material.
After the operation, patients were prescribed dexamethasone 0.1% and ofloxacin 0.3% eyedrops, to be taken 4 times daily for 2 weeks. The patients also received sodium hyaluronate eye drops, for administration 4 times a day for 1 month.
Polar value analysis of refractive astigmatism
Net astigmatism was decomposed into two polar values: the meridional (AKP) and torsional (AKP+45) powers (11). Naeser (11) described the two polar values as follows;
[1]
[2]
The magnitude and axis of astigmatic change obtained through surgery is defined as the SIA vector. The difference in astigmatism postoperatively and preoperatively (expressed as AKP, AKP + 45) can be calculated. The errors of treatment were expressed as AKPerror and AKP + 45error, which were calculated through subtraction of the actual postoperative AKP and AKP + 45 from the intended keratometry or refraction. Undercorrection and overcorrection are represented by positive and negative AKPerror, respectively. A positive AKP + 45error indicates an anticlockwise torque, while a negative AKP + 45error indicates a clockwise torque. Furthermore, according to Naeser’s method, the net cylinder format was obtained by using the general equations set out below.
[3]
[4]
Statistical analysis
Data were documented in Microsoft Excel (Microsoft, Redmond, Washington, USA) and analyzed statistically in SPSS software version 23.0 for Windows (SPSS, Inc., Chicago, IL, USA). Data were described as mean ± standard deviation (SD), and the Kolmogorov-Smirnov test was employed to test for normality. Before comparing preoperative and postoperative data, the paired t-test was used. As previously reported, bivariate analyses of the combined mean polar values with calculation of two-dimensional confidence ellipses were performed using Hotelling T2 (15). One-way analysis of variance was used for subgroup evaluation. Spearman’s correlation was employed for correlation analysis. All P values were two-sided and statistical significance was considered to exist when the value was <0.05.
Results
Table 1 summarizes the patients’ demographic information. All surgeries were uneventful, with no intra- or post-operative complications recorded. The mean central vault was 641.18±261.91 µm (240–1,580 µm). The ECD reduced significantly (t test, P=0.002), from 2,950.07± 285.57 cells/mm2 before surgery to 2,819.90±418.87 cells/mm2 after surgery. During follow-up, no high IOP, anterior subcapsular cataract, or other complications occurred.
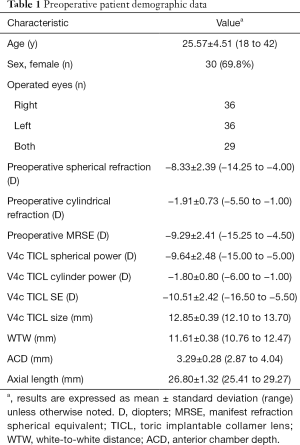
Full table
Visual and refractive outcomes
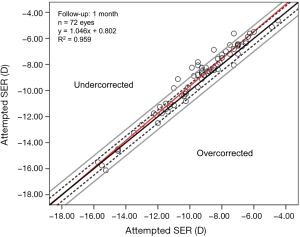
Table 2 describes patients’ visual and clinical parameters before and after surgery. The efficacy (mean postoperative UCVA/mean preoperative best-spectacle corrected visual acuity, BSCVA) and safety indices (mean postoperative BSCVA/mean preoperative BSCVA) were 1.13 and 1.17, respectively. A significant reduction of 8.92±2.58 D was observed in the spherical equivalent refraction (SER), from −9.29±2.41 D preoperatively to −0.37±0.55 D postoperatively, indicating slight undercorrection. Figure 1 displays the achieved SER at the 1-month follow-up against the attempted SER. The linear regression model of achieved vs. attempted SER produced a slope, intercept, and coefficient (R2) of 1.049, 0.815, and 0.957, respectively.
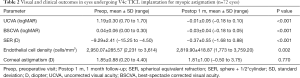
Full table
Polar analysis of refractive astigmatism
Table 3 summarizes the preoperative and postoperative astigmatic polar values with the steeper meridian of the preoperative refractive astigmatism as the reference plane. After surgery, a statistically significant flattening of the surgical meridian was observed (t=13.828, P<0.001). The minimum induced counterclockwise torque was 0.25±0.31 D. The SIA of the net cylinder format was obtained by using Eqs. [3] and [4] on the polar values, which was 1.39±0.51 @ 84.83º relative to the preoperative stronger meridian at 1 month. In combination, the mean SIA polar values for SIA showed a statistically significant difference from zero (Hotelling T2 =231.871; P<0.001). Figure 2 plots the TIA vs. SIA at 1 month, postoperatively. The achieved and intended astigmatic corrections were found to be statistically significantly correlated (R2 =0.612, P<0.001).
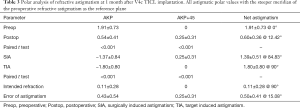
Full table
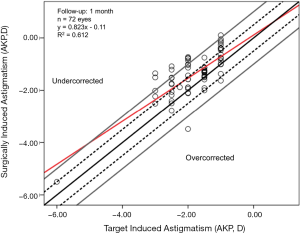
Figure 2 and Table 3 also show a significant undercorrection of astigmatism (t=3.892, P<0.001). In terms of postoperative residual astigmatism, the percentage of eyes with postoperative cylinder values within 0.50 D, 0.75 D, 1.00 D, and 1.50 D was 41.7% (30 eyes), 70.9% (51 eyes), 86.2% (62 eyes), and 98.7% (71 eyes), respectively. The difference between the intended postoperative and the actual refraction was defined as the error of treatment. The error of treatment was calculated to 0.50±0.41 @ 15.08° (net cylinder format) relative to the preoperative stronger meridian at 1 month postoperatively. At the 1-month follow-up, the mean absolute error was 0.54±0.43 D and the percentage of eyes with error within 0.25 D, 0.50 D, 0.75 D, and 1.00 D was 33.3% (24 eyes), 56.9% (41 eyes), 70.8% (51 eyes), and 86.1% (62 eyes), respectively.
According to the power of the V4c TICL, the eyes in this study were categorized into two groups for further analysis: the ≤2.0 D group and the >2.0 D group. Table 4 shows the polar values of each group. As the power of the V4c TICL increased, the error of treatment became greater.

Full table
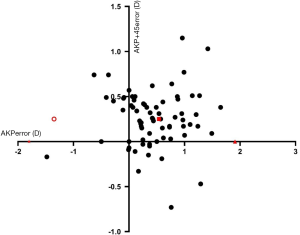
Besides the changes at the main meridian, astigmatism was also induced at the oblique meridian (expressed as AKP + 45). Thus, the error of target in AKP + 45 indicated a significant minor anticlockwise torsion of the cylinder axis (t=3.965, P<0.001). Figure 3 displays preoperative astigmatism and postoperative residual astigmatism of individual two polar values and the 95% tolerance ellipses are shown. When combined, the mean polar values for the dioptric error showed a significant difference from zero (Hotelling T2 =6.317; P=0.014).
Rotational stability after TICL implantation
The mean fixation angle in 56 eyes was 3.91°±2.76° (range, 1 to 10 degrees). For all cases included in the study, the mean V4c TICL fixation angle was 3.17°±2.92°. Based on the polar value analysis, the mean V4c TICL rotation after surgery was 7.09°±10.90° (median =4.95 degrees; range, −12.43 to 58.88 degrees). The mean absolute value of the V4c TICL rotation was 8.30°±10.00° (median =5.46 degrees; range, 0.00 to 58.88 degrees). Figure 4 shows the distribution of the V4c TICL rotation at 1 month after surgery.

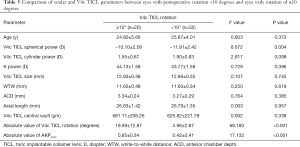
Based on the degree of the V4c TICL rotation, the cases were divided into two groups for subgroup analysis: group 1, a large amount of rotation (≥10°) and group 2, a small amount of rotation (<10°). As shown in Table 5, significant differences were observed in V4c TICL spherical power, the absolute value of AKPerror, and the absolute value of V4c TICL rotation between the two groups. No significant between-group differences were found for any other parameter.
Full table
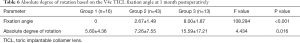
Another subgroup analysis was performed based on the fixation angle of the V4c TICL. The cases were assigned to one of three groups: group 1 (the alignment group, n=16 eyes) with the fixation angle of the V4c TICL on the horizontal axis; group 2 (misalignment group 1, n=43 eyes) with a fixation angle of the V4c TICL off the horizontal axis ≤5°; and group 3 (misalignment group 2, n=13 eyes) with a fixation angle of the V4c TICL off the horizontal axis >5°. Table 6 shows the V4c TICL fixation angle and absolute degree of rotation in each group. A significant difference was found in the fixation angle of the V4c TICL between groups 2 and 3; however, groups 1 and 2 showed no significant differences between them.
Full table
Discussion
We analyzed the visual and refractive results and rotational stability after V4c TICL implantation in 43 patients (72 eyes). Our results proved that the V4c TICL can be used to effectively and safely correct moderate to high myopic astigmatism. The efficacy and safety of TICL implantation in patients with medium and high astigmatism was studied in several previous articles, which reported safety and efficacy indices of 1.08 to 1.38 and 1.01 to 1.35, respectively (3,16,17).
Similar to these studies, our study found the safety and efficacy indices of visual outcomes to be satisfactory, standing at 1.17 and 1.13, respectively, at 1 month postoperatively. No eye lost lines of BSCVA, and 69.4% of eyes gained one or more lines of BSCVA. At the 1-month follow-up, a UCVA of 20/20 or better was seen in 82% of eyes, and 56.9% of eyes had a BSCVA of 20/20 preoperatively.
In most people with healthy eyes, uncorrected astigmatism results in a significant decrease in visual performance, even when only a small amount of residual astigmatism is present (1,2). For instance, in the current study, the mean logMAR UCVA was −0.01±0.05 at 1 month postoperatively. After correction of the residual astigmatism, visual acuity improved significantly to −0.03±0.04 (t=4.412, P<0.001). Therefore, it is necessary to analyze the causes of residual astigmatism after implantation of the V4c TICL.
Astigmatic power is expressed as magnitude in diopters and direction in degrees (10-15,18,19). Therefore, vector analysis should be used to evaluate the effect of the V4c TICL on astigmatic correction. Using Naeser’s method, we performed vector analysis in our study, and polar value analysis was adopted to obtain useful information on surgical outcomes. The steeper meridian of the preoperative refractive astigmatism (intended meridian) was fixed for procedures. In the current study, we found that in 58.3% of eyes, the astigmatism remained 0.50 D or more after the operation. With the preoperative stronger meridian as the reference plane, the mean postoperative astigmatism in net cylinder format was calculated to 0.60 D±0.36 @ 12.42° at 1 month postoperatively. These values were similar to those reported by Sanders et al. and Hashem et al., who found that the magnitude of the mean postoperative astigmatism was 0.51 D±0.48 and 0.63 D±0.75, respectively. However, the degree of the mean postoperative astigmatism relative to the preoperative stronger meridian was not reported in their studies. Moreover, there was a significant correlation between the achieved and intended astigmatic corrections (expressed as AKP). Thus, in our study, astigmatic undercorrection amounting to 18% per diopter was found by using linear regression analysis. In the subgroup analysis, as the V4c TICL cylinder magnitude increased, the error of treatment became higher (Table 4). In the subgroup with a V4c TICL cylinder power of more than 2 D, the highest mean absolute error of meridional power (expressed as AKP) was 0.75±0.49 D at 1 month postoperatively.
According to the Alpins method (17), correction index (CI) is defined as the ratio of SIA to TIA. A value <1 represents undercorrection, a value >1 represents overcorrection. In our study, the CI was 0.75, which is lower than those reported in recent studies by Hyun et al. (0.82) (16) and Lee et al. (0.91). (17) The difference in results can be attributed to the difference in TICL rotation in these studies. Hyun et al. (16) reported a 3.39°±2.36° postoperative rotation, as measured by digital anterior segment photography, whereas Lee et al. (17) reported a 3.87°±3.07° postoperative rotation, which was obtained by OPD-Scan III. In achieving high efficacy in the correction of astigmatism, the rotational stability of the V4c TICL is well known to be a crucial factor. In our study, however, the mean absolute rotation by polar value analysis (8.30°±10.00°) was larger than those reported in Hyun et al. and Lee et al.’s studies. Furthermore, Mori et al. (20) also used vector analysis to report a 4.82°±6.98° (range, 0.0 to 47.2°) postoperative rotation, which is less than that reported the mean absolute rotation in our study. With an absolute degree of rotation of 15.59°±17.21° in eyes with a fixation angle more than 5° at 1 month postoperatively, which is significantly higher than that in eyes with an angle less than or equal to 5° (P=0.016).
As shown in Table 5, the absolute value of rotation and the spherical power of the V4c TICL were significantly correlated. This result is similar to that of a previous study by Park et al. (4). However, two recent studies found no significant correlation between the absolute value of rotation and the spherical power of the toric ICL (16,20). These differences in results may be due to differences in participant characteristics, such as the different types of torus ICL used.
Apart from postoperative rotation of the V4c TICL, another key factor in determining the tendency of undercorrection after V4c TICL implantation is intended refraction. The mean absolute difference between preoperative cylinder power and V4c TICL cylinder power was 0.18±0.25 D (range, 0.00 to 1.00 D). Therefore, to develop a nomogram to improve astigmatic outcomes, the preoperative refraction should be consistent with the attempted refraction. However, further research is needed to assess the astigmatism using this new nomogram.
This study has limitations, and further research is still required. First, the study had a small number of cases and short follow-up period. We are currently conducting a longer-term follow-up study, the results of which will be reported in the future. Second, V4c TICL rotation was mathematically calculated and not directly measured. To validate our results, slit-lamp microscopy to directly observe the V4c TICL location should be performed.
In conclusion, V4c TICL implantation could provide good astigmatic outcomes in patients with moderate to high myopic astigmatism. After the implantation of a TICL to treat myopia and myopic astigmatism, corneal astigmatism remained unchanged. Polar value analysis can be used to guide the construction of a nomogram to optimize postoperative astigmatic outcomes in TICL.
Acknowledgments
The authors thank Bryan Spencer for polishing the language of this article.
Funding: The authors gratefully acknowledge grant support from SanMing Project of Medicine in Shenzhen, Shenzhen, Guangdong, China (SZSM201812091) and the Science and Technology Planning Projects of Guangdong Province (grant no. 2018B010109008).
Footnote
Reporting Checklist: The authors have completed the MDAR checklist. Available at http://dx.doi.org/10.21037/atm-20-7835
Data Sharing Statement: Available at http://dx.doi.org/10.21037/atm-20-7835
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/atm-20-7835). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by ethics board of Shenzhen Eye Hospital (NO.:b-07). All patients signed written informed consent.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Wolffsohn J, Bhogal G, Shah S. Effect of uncorrected astigmatism on vision. J Cataract Refract Surg 2011;37:454-60. [Crossref] [PubMed]
- Kamiya K, Kobashi H, Shimizu K, et al. Effect of pupil size on uncorrected visual acuity in astigmatic eyes. Br J Ophthalmol 2012;96:267-70. [Crossref] [PubMed]
- Alfonso JF, Lisa C, Alfonso-Bartolozzi B, et al. Collagen copolymer toric phakic intraocular lens for myopic astigmatism: one-year follow-up. J Cataract Refract Surg 2014;40:1155-62. [Crossref] [PubMed]
- Park SC, Kwun YK, Chung ES, et al. Postoperative astigmatism and axis stability after implantation of the STAAR Toric Implantable Collamer Lens. J Refract Surg 2009;25:403-9. [Crossref] [PubMed]
- Sanders DR, Schneider D, Martin R, et al. Toric Implantable Collamer Lens for moderate to high myopic astigmatism. Ophthalmology 2007;114:54-61. [Crossref] [PubMed]
- Hashem AN, El Danasoury AM, Anwar HM. Axis alignment and rotational stability after implantation of the toric implantable collamer lens for myopic astigmatism. J Refract Surg 2009;25:S939-43. [Crossref] [PubMed]
- Schallhorn S, Tanzer D, Sanders DR, et al. Randomized prospective comparison of visian toric implantable collamer lens and conventional photorefractive keratectomy for moder ate to high myopic astigmatism. J Refract Surg 2007;23:853-67. [Crossref] [PubMed]
- Kamiya K, Shimizu K, Igarashi A, et al. Comparison of Collamer toric implantable [corrected] contact lens implantation and wavefront-guided laser in situ keratomileusis for high myopic astigmatism. J Cataract Refract Surg 2008;34:1687-93. [Crossref] [PubMed]
- Sanders DR, Sanders ML. Comparison of the toric implantable collamer lens and custom ablation LASIK for myopic astigmatism. J Refract Surg 2008;24:773-8. [Crossref] [PubMed]
- Naeser K. Surgically induced astigmatism is characterized by optical vectors, not by ratios. J Cataract Refract Surg 2016;42:347-8. [Crossref] [PubMed]
- Næser K. Assessment and statistics of surgically induced astigmatism. Acta Ophthalmologica 2008;86:5-28. [Crossref] [PubMed]
- Ivarsen A, Næser K, Hjortdal J. Laser in situ keratomileusis for high astigmatism in myopic and hyperopic eyes. J Cataract Refract Surg 2013;39:74-80. [Crossref] [PubMed]
- Qian Y, Huang J, Zhou X, et al. Comparison of femtosecond laser small-incision lenticule extraction and laser-assisted subepithelial keratectomy to correct myopic astigmatism. J Cataract Refract Surg 2015;41:2476-86. [Crossref] [PubMed]
- Rho CR, Kim MJ, Joo CK. Polar Value Analysis of Corneal Astigmatism in Intrastromal Corneal Ring Segment Implantation. J Ophthalmol 2016;2016:7127534. [Crossref] [PubMed]
- Naeser K, Hjortdal J. Multivariate analysis of refractive data: mathematics and statistics of spherocylinders. J Cataract Refract Surg 2001;27:129-42. [Crossref] [PubMed]
- Hyun J, Lim DH, Eo DR, et al. A comparison of visual outcome and rotational stability of two types of toric implantable collamer lenses (TICL): V4 versus V4c. PLoS One 2017;12:e0183335. [Crossref] [PubMed]
- Lee H, Sung Yong Kang D, Jin YC, et al. Rotational stability and visual outcomes of V4c toric phakic intraocular lenses. J Refract Surg 2018;34:489-96. [Crossref] [PubMed]
- Savini G, Versaci F, Vestri G, et al. Influence of posterior corneal astigmatism on total corneal astigmatism in eyes with moderate to high astigmatism. J Cataract Refract Surg 2014;40:1645-53. [Crossref] [PubMed]
- Yan P, Du Z, Zhang Y. Polar Value Analysis of Low to Moderate Astigmatism with Wavefront-Guided Sub-Bowman Keratomileusis. J Ophthalmol 2017;2017:5647615. [Crossref] [PubMed]
- Mori T, Yokoyama S, Kojima T, et al. Factors affecting rotation of a posterior chamber collagen copolymer toric phakic intraocular lens. J Cataract Refract Surg 2012;38:568-73. [Crossref] [PubMed]


